-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 1263-1266
doi:10.5923/j.ajmms.20251504.86
Received: Feb. 20, 2025; Accepted: Mar. 16, 2025; Published: Apr. 29, 2025

Immunologic Manifestations of Exudative Otitis Media in Children on the Background of Immunocorrection
M. T. Nasretdinova , Dustboboyev D. S. , Normuradov N. A.
Samarkand State Medical University, Samarkand, Uzbekistan
Copyright © 2025 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The results of conservative treatment of 42 children suffering from exudative otitis media were analyzed. All patients received complex treatment including medication and mechanotherapy. Patients of the observation group (n = 20) additionally received immunocorrection with intranasal spray Imunofan. Patients of the comparison group (n = 22) were not immunocorrected. Against the background of Immunofan administration the clinical result evaluated in points according to the results of questionnaire was 1.6 times better in a month and 2.2 times better in 3 months than in children of the comparison group. Neutrophil myeloperoxidase activity under immunocorrection was significantly higher by the end of the 1st month (2.2 vs. 1.8) and by the 3rd month (2.9 vs. 1.5) and reached the level of physiologic norm.
Keywords: Exudative otitis media, Hearing loss, Myeloperoxidase, Immunophan
Cite this paper: M. T. Nasretdinova , Dustboboyev D. S. , Normuradov N. A. , Immunologic Manifestations of Exudative Otitis Media in Children on the Background of Immunocorrection, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1263-1266. doi: 10.5923/j.ajmms.20251504.86.
Article Outline
1. Introduction
- The problem of hearing loss in pediatric practice at present remains urgent and acquires not only medical, but also socioeconomic significance, since hearing loss in childhood can be the cause of impaired auditory and intellectual development, learning difficulties, and can lead to social maladaptation of the child [1,3,7]. In the structure of pediatric hearing loss, as is known, the largest share belongs to the conductive form, represented mainly by auditory tube dysfunction and exudative otitis media [2,5]. Over the last twenty years, the number of children with exudative otitis media has increased 2.5-fold [4,6,8]. Exudative otitis media (EOM) is a polyetiologic non-purulent inflammatory disease of the middle ear, accompanied by the accumulation of exudate in its cavities and symptomatically manifested by conductive or mixed hearing loss. Despite advances in the study of the etiology and pathogenesis of the disease, the problems associated with the treatment of ESO, to date, remain very relevant. The role of chronic inflammation of the pharyngeal tonsil and decreased activity of local mucosal immunity as triggering factors in the development of EOM in children is being actively discussed [9]. The status of mucosal immunity is largely determined by the structural organization and functional capabilities of subepithelial lymphoid tissue, as well as the state of nonspecific defense factors (epithelial cover, functional properties of macrophages and neutrophils). It is known that one of the main participants of nonspecific defense of the organism, realized in childhood, are neutrophil granulocytes (NG). Functional capabilities of these blood cells determine the protection of mucous membranes and adequate inflammatory response. In this connection, we selected one of the main lysosomal enzymes of neutrophils, myeloperoxidase (MP), which causes oxidation of chlorine anion by hydrogen peroxide to hypochlorite, a substance with a strong antibacterial effect, to assess the state of innate immunity. The content of myeloperoxidase is an adequate indicator of the functional capabilities of neutrophils and the state of nonspecific defense of the organism.The aim of the study was to investigate the indices of innate immunity and to evaluate the effectiveness of treatment of exudative otitis media in children against the background of immunomodulatory drug application.
2. Material and Methods of the Study
- There were 42 children (25 boys and 17 girls) with ESO at the age of 3 to 7 years who underwent the course of treatment in the department of otorhinolaryngology of Samarkand State Medical University. As a control group, 16 practically healthy children (8 boys and 8 girls) aged 3 to 7 years were examined. The examination of all patients included questionnaires, otorhinolaryngological examination, instrumental (tympanometry and tonal audiometry), cytochemical (determination of myeloperoxidase activity in peripheral blood neutrophils) methods.The criteria for patient selection were as follows: uni- or bilateral hearing loss, otoscopically - exudate in the tympanic cavity without signs of acute inflammation, tympanogram type “B”, according to threshold and game audiometry - conductive hearing impairment, bone-air interval in the zone of speech frequencies ≥ 20 dB, informed consent of the legal representative. Among the concomitant pathology in the examined children in 100% of cases was diagnosed pharyngeal tonsil hypertrophy of II or III degree. All children attended preschool institutions. By randomization all patients were divided into two groups: comparison group (22 children who received only traditional therapy) and observation group (20 children who additionally received immune-correcting therapy). Traditional treatment included: antihistamines (desloratadine), mucolytic (acetylcysteine), vasoconstrictors (phenylephrine hydrochloride), mechanotherapy (Politzer blowing of auditory tubes, pneumatic massage of tympanic membranes), laser therapy in the nasal cavity and endaural electrophonophoresis with 3% potassium iodide solution. All drugs were administered in ageappropriate doses. Patients of the observation group were additionally treated with intranasal spray Imunofan: 1 dose (50 mcg) in each half of the nose 2 times a day daily for 7 days, then 1 dose (50 mcg) in each half of the nose once a day (at night) daily for 14 days and then again 1 dose (50 mcg) in each half of the nose 2 times a day daily for 7 days.To assess hearing loss, we developed a questionnaire for parents of children. This questionnaire includes ten questions. The first five questions verify the symptoms of nasal and nasopharyngeal pathology as triggers for otitis media development in children. The second section of the questionnaire consists of five questions that aim to identify symptoms of hearing loss and speech impairment in the child. Each questionnaire item includes five progressive response options (1-5) to assess the severity of the corresponding symptom. Convergent validation of the questionnaire was performed beforehand. MР activity in neutrophils was determined cytochemically on peripheral blood smears stained according to the Gracham-Knoll method, with microscopic evaluation of the content of specific granules and calculation of the average cytochemical coefficient. Statistical processing of the results was performed using Statistica 8,0 program. Variance analysis took into account the calculation of medians (Me) and quartile shifts [T25%-T75%]. Quantitative data were analyzed by comparison of independent samples using the Mann-Whitney test. Dynamics during treatment was evaluated using the Wilcoxon rank criterion. The results were considered reliable at p<0.05.
3. Results and Their Discussion
- All patients had symptoms of uni or bilateral hearing loss, sensation of stuffiness in the ears, nasal congestion. Otoscopic examination in all children showed retraction or bulging of the tympanic membrane, absence or shortening of the light cone, change in the color of the tympanic membrane (pink, yellowish, livid).According to acoustic impedanceometry before treatment, all children had tympanogram type “B”, acoustic reflex was not registered. The results of tonal threshold and game audiometry in all examined patients indicated a conductive hearing impairment; the bone-air interval in the speech frequency zone averaged 36 ± 12 dB.Evaluation of treatment results in all patients was carried out 1 and 3 months after the beginning of therapy. The results of questionnaire survey of parents of children of both clinical groups (point estimation) are presented in Fig. 1.
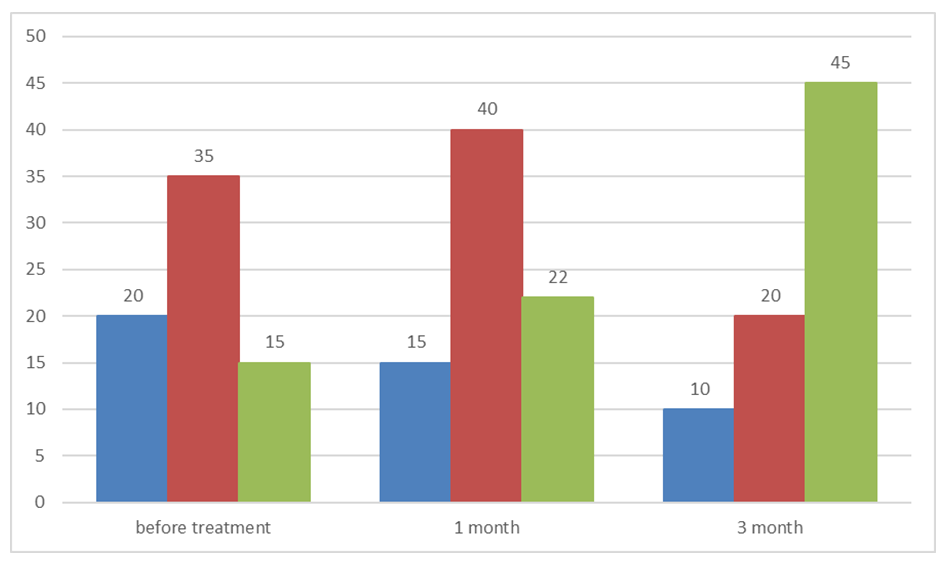 | Figure 1. Questionnaire results in dynamics before and after treatment |
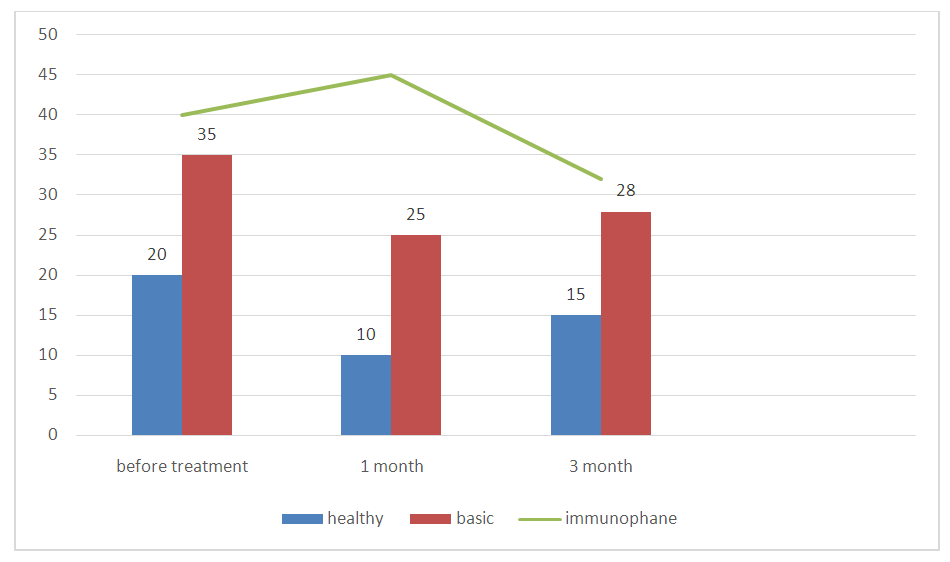 | Figure 2. Myeloperoxidase activity in blood neutrophils before and after treatment |
4. Conclusions
- 1. The use of screening questionnaires helps to diagnose ESO in children at earlier stages and to evaluate the effectiveness of treatment of this disease.2. The results of the study indicate functional inferiority of blood neutrophils in children with pharyngeal tonsil hypertrophy, which may be a pathogenetic basis for the development of ESO.3. Application of the preparation Imunofan for the purpose of local immunocorrection allows to restore the activity of MF of blood neutrophils to physiologic values.4. Increased efficiency of treatment of ESO in children with the use of immunomodulating drug Imunofan is confirmed by objective clinical dynamics and faster decrease in the severity of symptoms in the nasopharynx and hearing.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML