-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 1239-1242
doi:10.5923/j.ajmms.20251504.81
Received: Mar. 16, 2025; Accepted: Apr. 17, 2025; Published: Apr. 26, 2025

Assessment of Psychoemotional and Cognitive State in Patients with Ischemic Stroke on the Background of Metabolic Syndrome Using Tests
Teshaeva Malika Qahramonovna 1, Khodjieva Dilbar Tadjievna 2
1Bukhara State Medical Institute, Bukhara, Uzbekistan
2Doctor of Medical Sciences, Professor of the Department of Neurology, Bukhara State Medical Institute, Bukhara, Uzbekistan
Copyright © 2025 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Metabolic syndrome can be evaluated as an independent factor that aggravates the course of ischemic stroke and increases the risk of developing psychoemotional and cognitive disorders. It is necessary to apply regular testing methods to assess the psychoemotional and cognitive state in patients with metabolic syndrome who have had a stroke, and to develop early rehabilitation measures.
Keywords: Metabolic syndrome, Ischemic stroke, Psychoemotional state, Cognitive disorders, Depression, Anxiety, MMSE, MoCA, Beck scale, Spielberg-Khanin scale
Cite this paper: Teshaeva Malika Qahramonovna , Khodjieva Dilbar Tadjievna , Assessment of Psychoemotional and Cognitive State in Patients with Ischemic Stroke on the Background of Metabolic Syndrome Using Tests, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1239-1242. doi: 10.5923/j.ajmms.20251504.81.
1. Introduction
- Stroke occupies one of the leading positions among the causes of disability and death worldwide. According to the World Health Organization, more than 15 million people worldwide suffer strokes each year, and approximately one-third of them die, while another third suffers permanent disability [1,2]. One of the main factors determining the quality of life of patients in the post-stroke period is their psychoemotional and cognitive state[7,8]. In recent years, numerous studies have been conducted on metabolic syndrome (MS) and its effect on stroke progression. Metabolic syndrome is a complex pathological condition that includes components such as central obesity, arterial hypertension, dyslipidemia, and impaired glucose tolerance, all of which increase the risk of cerebrovascular diseases [3,4]. Scientific works devoted to the relationship between ischemic stroke developed against the background of metabolic syndrome and psychoemotional and cognitive disorders are limited. Additionally, post-stroke depression, anxiety, and cognitive impairments are closely interconnected, reduce the effectiveness of rehabilitation, and negatively affect the level of functional recovery of patients [5,6].The purpose of this study is to assess the psychoemotional and cognitive state of patients with ischemic stroke developed against the background of metabolic syndrome using standardized tests and to determine their significance in the clinical course.
2. Materials and Methods
- The study was conducted during 2023-2024 at the Republican Specialized Center of Neurology and Stroke. 120 patients diagnosed with ischemic stroke were included in the study. Metabolic syndrome was identified in 76 of them (63.3%), who formed the main group, while 44 patients (36.7%) without signs of metabolic syndrome were included in the comparison group.The diagnosis of metabolic syndrome was established according to the criteria of the International Diabetes Federation (IDF, 2005). According to the criteria, central obesity (waist circumference ≥94 cm in men, ≥80 cm in women) and at least two of the following criteria must be present:• triglyceride level >1.7 mmol/L or treatment for hyperlipidemia;• high-density lipoprotein level <1.03 mmol/L in men, <1.29 mmol/L in women;• arterial blood pressure ≥130/85 mm Hg or treatment for hypertension;• fasting plasma glucose level ≥5.6 mmol/L or previously diagnosed type 2 diabetes.The diagnosis of stroke was confirmed by brain CT or MRI examinations. Inclusion criteria for the study were: acute ischemic stroke, age 45-75 years, moderate neurological deficit (5-15 points on the NIHSS scale), and informed consent. Exclusion criteria included severe post-stroke condition (NIHSS>15), severe somatic diseases, psychiatric disorders, brain dementia or severe cognitive impairments in the anamnesis, alcoholism and drug use, and inability to establish verbal contact.The assessment of psychoemotional and cognitive state in patients was carried out using the following tests:Tests for assessing cognitive functions:1. MMSE (Mini-Mental State Examination) - a 30-point scale that assesses orientation, memory, attention, calculation, speech, and constructive praxis. 24-30 points - normal, 18-23 points - mild cognitive impairment, 10-17 points - moderate cognitive impairment, less than 9 points - severe cognitive impairment.2. MoCA (Montreal Cognitive Assessment) - a 30-point test that assesses executive functions, visual-spatial abilities, attention, memory, and others. 26-30 points - normal, 19-25 points - mild cognitive impairment, 11-18 points - moderate cognitive impairment, less than 10 points - severe cognitive impairment.Tests for assessing psychoemotional state:1. Beck Depression Inventory (BDI-II) - a questionnaire consisting of 21 questions, with each question rated from 0 to 3. Total scores: 0-13 - no depression, 14-19 - mild depression, 20-28 - moderate depression, 29-63 - severe depression.2. Spielberg-Khanin Anxiety Scale - a test that allows the assessment of reactive (situational) and personal (trait) anxiety. Each scale consists of 20 questions. Total scores: 0-30 - low level, 31-45 - medium level, 46 and above - high level.Examinations were conducted twice - 7-10 days after the stroke and 3 months later. The obtained data were statistically analyzed, mean values were expressed with standard deviation (M±SD). Intergroup differences were assessed using Student's t-test and Mann-Whitney U-test. Differences were considered statistically significant at p<0.05.
3. Results of the Study
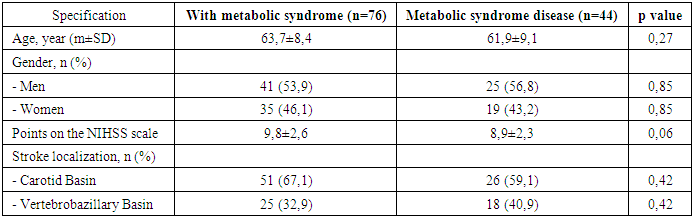
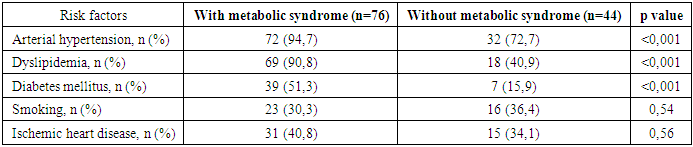
- The demographic and clinical characteristics of the patients included in the study are presented in Table 1. No statistically significant differences were observed between the two groups in terms of age and gender distribution. It was found that the severity of stroke according to the NIHSS scale was slightly higher in the main group, but this difference was not statistically significant.
|
|
|
|
|
4. Conclusions
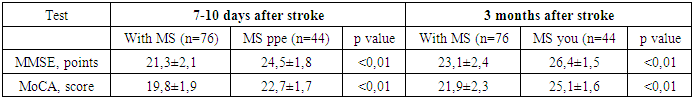
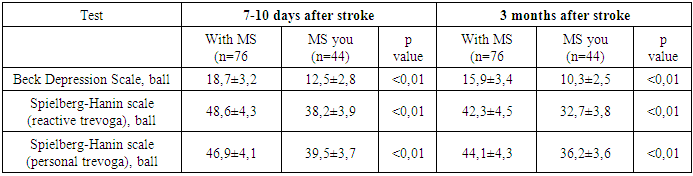
- In ischemic stroke, which develops against the background of metabolic syndrome, cognitive disorders are significantly more severe (21.3±2.1 points on the MMSE scale, 19.8±1.9 points on the MoCA test). Even in the 3-month post-stroke period, patients with metabolic syndrome have a high level of cognitive impairment, and this is observed in 61.8% of patients. The MoCA test has been found to be more sensitive to MMSE in detecting mild post-stroke cognitive impairment, especially when evaluating performance functions. In patients with metabolic syndrome, clinically significant depression in the post-stroke period (68.4% of cases) and high levels of trevoga (64.5% of cases) are significantly more common compared to the control group. There is a direct relationship between depression and trevoga levels and the severity of cognitive impairment (r = -0.62 to -0.68; p<0.01). Post-stroke depression was of a persistent nature and no complete regression was observed for 3 months, indicating the need for long-term psychological support.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML