-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 1198-1200
doi:10.5923/j.ajmms.20251504.71
Received: Apr. 2, 2025; Accepted: Apr. 22, 2025; Published: Apr. 26, 2025

Detection of Dental Diseases in Women of Fertile Age with Breast Cancer
Nurova Shohsanam
PhD., Bukhara State Medical Institute of Orthopedic Dentistry and Orthodontics Department, Uzbekistan
Correspondence to: Nurova Shohsanam , PhD., Bukhara State Medical Institute of Orthopedic Dentistry and Orthodontics Department, Uzbekistan.
| Email: |  |
Copyright © 2025 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In women with breast cancer, in women with early menopause, there is a development of a high level of dental diseases in the adaptation phase of the body, with a lack of the hormone estrogen or its abrupt complete absence after radiation, chemotherapy and hormone therapy (1) Background: thus, changes in bones caused by the use of endocrine therapy, chemotherapy and surgical methods in the treatment of breast cancer are currently an urgent problem. It has also been proven that estrogen deficiency negatively affects the condition of the hard tissues of the tooth and especially the condition of periodontal tissue (2) Metods: The objective condition of periodontal tissues was studied based on the dynamics of the following tests (3) Conclusions: Among the examined patients, with an average periodontal disease of 65%, severe periodontitis was diagnosed in 35% against the background of osteopenia (4).
Keywords: Generalized periodontitis, Dental defects, Hormones, Menopause, Chemotherapy, Breast cancer, Estrogen, Hygiene index, Degree of bleeding, RMA, PI, The depth of the periodontal pocket, Postmenopausal osteoporosis, Osteopenia
Cite this paper: Nurova Shohsanam , Detection of Dental Diseases in Women of Fertile Age with Breast Cancer, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1198-1200. doi: 10.5923/j.ajmms.20251504.71.
1. Introduction
- Menopause is the main cause of chronic generalized periodontitis after radiation and chemical therapy in women with breast cancer. One of the factors of the development of the disease during menopause is changes in the microcirculation system. Microcirculation disorders, chronic hypoxia in periodontal tissues, and nutritional disorders contribute to the destruction of periodontal tissues. On the other hand, microcirculation is primarily caused by inflammation of the tissues of their endothelial walls, ischemia and excessive damage in others, which eliminates the protective barrier, helping the periodontium to become one of the pathomechanisms of the disease.With long-term treatment, patients with breast cancer develop large and small pain syndromes of the spine of the bones, prolonged and persistent joint pain were observed during dispensary control. The pathogenesis of pain syndrome in patients is often caused by osteoporosis (OP) in breast cancer. Chemotherapy and hormone therapy are factors with a pronounced effect on the metabolic process of the bone structure [1,3,5].Chemotherapy also affects bone mineral density by affecting the dysfunction of the ovaries with bone tissue against the background of cytostatic therapy, which at one time causes the rapid development of early menopause and osteoporosis.In breast cancer (BC), drugs that act on tumors that occur in a hormone-dependent manner affect the patient's menstrual cycle, and at the same time, there is a change in bone density. For adjuvant treatment of breast cancer, tamoxifen hormone antagonists or gonodotropin-releasing antagonists are used, leading to bone loss of up to 7% during one year of treatment [9].
2. Background
- Surgical intervention also leads to artificial menopause according to the indications of ovarektomy, which increases the risk of fractures characteristic of osteoporosis. [8]. Thus, changes in bones caused by the use of endocrine therapy, chemotherapy and surgical methods in the treatment of breast cancer are currently an urgent problem. [9]. Osteoporosis causes unpleasant symptoms, negatively affecting patients with this type of cancer. [6]. Solving the problem of the spread of periodontal tissue diseases is one of the most important and urgent tasks of modern dentistry. 12% of the population has a healthy periodontal disease. In people over 35 years of age, the proportion of initial periodontal changes gradually decreases by 26-15%, at the same time, an increase in the number of changes from moderate to severe to 75% was observed. This, in turn, leads to the appearance of functional disorders in the dental and maxillary system. According to WHO, tooth loss as a result of periodontal diseases, functional disorders of the dental system develop five times faster than complications of caries, and is the second most common among all dental diseases. According to WHO, the incidence of periodontal disease is 55-69% in adolescents, 86.2% at the age of 35-44 years, and increases significantly at the age of 40-50 years (65-98%). In this regard, the diagnosis, treatment and prevention of these diseases will be of general medical and social importance. The issues of etiology and pathogenesis of periodontal diseases are explained in terms of the general influence of local and widespread factors, among them hormonal changes are pronounced, especially during postmenopause. It has been proven that insufficient estrogen levels during postmenopause cause an imbalance between resorption and bone formation, and this leads to rapid changes in bone structure, the development of osteoporosis and its complications. At the present stage, the relationship between the bone mineral density in various parts of the bones of the body and the height of the alveoli in the interproximal sections has been determined. According to the results of the study, a decrease in bone mineral density leads to a decrease in the interalveolar height, to a bend in the alveolar process that attaches to the gum or to the transitional fold. Osteoporosis during postmenopause is a dangerous factor in the development of periodontal diseases.The study was conducted in 2021-2023 at the Bukhara branch of the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology and at the Dental Scientific and Practical Center at the Bukhara State Medical Institute. The total number of examined patients was 703, of which 154 were control patients.
3. Methods
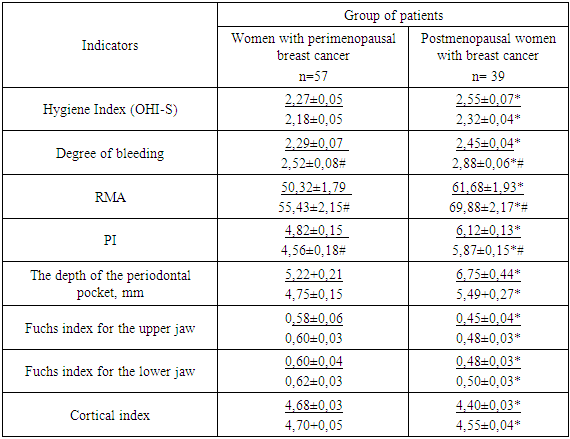
- 154 patients aged 55 to 65 years with diffuse periodontitis of moderate and severe severity, whose postmenopause lasted at least 5 years, were examined and treated. The examined patients are divided into groups:Group 1 consisted of 55 patients with CKD on the background of general osteoporosis (average age 58.30±0.65), menopause age 49.23±0.85, menopause duration was noted.Group 2 of 40 patients with CKD on the background of osteopenia (mean age 57.73±0.42 years), menopause age 48.65±0.69, menopause duration 9.5±0.88.In the comparative group, bone mineral density was normal (average age 57.92±0.49 years) at menopausal age 48.37±0.92 years, with menopause duration 9.47±0.59 years, in 40 patients with moderate menopausal CKD, and with moderate and severe CKD aged 25 to 45 years, 30 patients are in reproductive age (average age 39.5 ± 1.2 years), in whom bone tissue disorders were not noted. 20 women of reproductive age from the control group are practically healthy (average age 37.8 ± 1.1).To participate in the study, patients who had been diagnosed with breast cancer for at least 5 years, postmenopausal women with osteoporosis or CKD on the background of osteopenic syndrome were involved, and consent was obtained from them to participate in the study. A clinical examination of the oral cavity of women with breast cancer was conducted in order to determine the condition of the teeth, hard tissues of teeth, type of bite, protruding fold, presence of subgingival and supra-gingival solid carious deposits, condition of the oral mucosa (edema, hyperemia, bleeding), exudate condition, presence and depth of periodontal pockets, determination of the degree of pathological mobility of teeth. Attention was paid to the timing of the appearance of inflammatory changes in periodontal tissue and their connection with the onset of menopause. The results of the survey are presented in the table below.The objective condition of periodontal tissues was studied based on the dynamics of the following tests:- simplified hygienic index (OHI-S);- determination of the level of bleeding gums (Cowell I., 1975).- - papillary-marginal-alveolar index (PMA) (Parma G., 1960);- periodontal index (Russel A., 1967);- measurement of the depth of the periodontal pocket – (WHO data, 1989);- determination of the degree of pathological tooth movement (Fleszar T. J. et al., 1980).
|
|
4. Conclusions
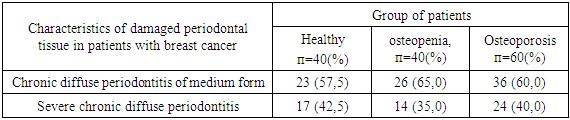
- Among patients with chronic diffuse periodontitis and postmenopausal osteoporosis, according to clinical and radiological data, 60% had moderate periodontal disease, and 40% had severe periodontal disease. Among the examined patients, with an average periodontal disease of 65%, severe periodontitis was diagnosed in 35% against the background of osteopenia. No significant difference was found in the statistical comparison of patients by group.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML