-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 1195-1197
doi:10.5923/j.ajmms.20251504.70
Received: Mar. 30, 2025; Accepted: Apr. 22, 2025; Published: Apr. 26, 2025

Preventive Measures for Liver Cirrhosis Caused by HDV Infection
Elmurodova A. A.
Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan
Correspondence to: Elmurodova A. A. , Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2025 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Liver cirrhosis caused by Hepatitis Delta Virus (HDV) infection remains a global health challenge, particularly in endemic regions. This study aims to evaluate and propose effective preventive measures to mitigate the progression of HDV-related liver cirrhosis. The research highlights immunological markers, antiviral strategies, and lifestyle modifications that contribute to the prevention of disease progression. Additionally, a detailed literature review on global trends, regional disparities, and novel therapeutic approaches is provided.
Keywords: Hepatitis, Liver cirrhosis, Prevention, HDV infection, Antiviral drugs, HCC, CD 4, CD 3, IL 4, IL 17
Cite this paper: Elmurodova A. A. , Preventive Measures for Liver Cirrhosis Caused by HDV Infection, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1195-1197. doi: 10.5923/j.ajmms.20251504.70.
1. Introduction
- Hepatitis Delta Virus (HDV) is a defective RNA virus that requires Hepatitis B Virus (HBV) co-infection for replication. First discovered in 1977, HDV is considered the most severe form of viral hepatitis due to its aggressive progression to liver cirrhosis and hepatocellular carcinoma (HCC). HDV superinfection in individuals already infected with HBV leads to a more rapid and severe course of liver disease, with a higher likelihood of decompensated cirrhosis and liver failure [1,2,3].HDV infection is a major global health concern, affecting an estimated 12 to 15 million people worldwide [4]. The World Health Organization (WHO) has identified HDV as a significant contributor to the global burden of liver disease, particularly in regions where HBV is endemic [5]. Despite progress in HBV vaccination programs, HDV prevalence remains high in parts of sub-Saharan Africa, the Middle East, Central Asia, and Eastern Europe, where healthcare access is limited, and prevention efforts are inadequate. The lack of targeted antiviral treatments exacerbates the situation, increasing the urgency for comprehensive preventive measures [6,7,8].The disease burden of HDV-related cirrhosis is further amplified by its association with severe liver complications, including liver failure and HCC [9]. Studies indicate that HDV-infected individuals have a threefold higher risk of developing HCC compared to those with HBV monoinfection. Moreover, liver transplantation remains the only viable treatment option for end-stage HDV-induced cirrhosis, placing additional strain on healthcare systems worldwide [10]. Therefore, prevention through early intervention, public health policies, and patient education is crucial in reducing HDV-associated morbidity and mortality.The absence of a direct antiviral therapy for HDV infection has made preventive strategies the most effective approach to controlling the disease. Current interventions include HBV vaccination, early antiviral treatment, and lifestyle modifications to reduce the risk of cirrhosis progression. Emerging therapies, such as entry inhibitors and immune-based treatments, offer potential solutions but remain under investigation [11]. Public health initiatives, including awareness campaigns, screening programs, and harm reduction strategies, are essential to curbing HDV transmission and minimizing its impact on affected populations [12].This paper reviews the epidemiology, risk factors, and pathogenesis of HDV, alongside an evaluation of existing and emerging preventive strategies. A particular focus is placed on immunological markers and liver function assessments, which provide insights into disease progression and treatment efficacy [13,14]. Understanding these factors is crucial for the development of comprehensive public health policies aimed at reducing HDV-related liver cirrhosis worldwide [15].
2. Materials and Methods
- This study includes statistical data from patients aged 18-74 diagnosed with HDV infection. Immunological markers such as Interleukin 4, Interleukin 17A, and CD markers (CD3, CD4, CD8, CD16, CD20, CD25, CD95) were analyzed in serum samples. Liver condition was assessed using ultrasound and Fibroscan. The effectiveness of preventive interventions, including antiviral therapy, dietary modifications, and public health initiatives, was evaluated using a comparative statistical approach.
3. Results
- The study included 197 patients with HDV-related liver disease. The age distribution was divided into three groups: 18-39 years, 40-59 years, and 60-74 years. Among these patients, males accounted for a higher percentage in each age group compared to females.In the main group (n=105), the largest proportion of patients belonged to the 40-59 age category, with 25.71% males and 20.95% females. The elderly group (60-74 years) also had a significant share, with 21.9% males and 20.0% females. The youngest age group (18-39 years) had the smallest representation, with 5.3% males and 3.8% females.In the comparison group (n=62), a similar trend was observed, with 20.97% of males and 19.71% of females falling within the 40-59 age range. The proportion of elderly patients was slightly lower than in the main group, with 13.7% males and 12.9% females.The control group (n=30) exhibited a more balanced age distribution. The 18-39 age group accounted for 26.7% males and 16.7% females. In the 40-59 age category, 16.7% of males and 20.0% of females were recorded, while in the 60-74 age group, males represented 23.3% and females 20.0%.Overall, the total population analysis showed that among the 197 patients, 6.6% of males and 3.0% of females were in the youngest age group (18-39 years). The highest concentration of patients was observed in the 40-59 age range, with 23.3% males and 20.8% females. In the elderly category (60-74 years), 21.9% of males and 20.0% of females were recorded.This distribution suggests that the highest burden of HDV-related liver cirrhosis is seen in middle-aged and older individuals, with a slightly higher prevalence among males.The study analyzed the distribution of patients based on their living environment, distinguishing between rural and urban settings. The findings reveal that a significant proportion of patients in the main group reside in rural areas (72 individuals) compared to urban dwellers (33 individuals). Similarly, in the comparison group, rural residents (32 individuals) slightly outnumber urban residents (30 individuals). These statistics suggest a higher prevalence of HDV-related liver cirrhosis in rural populations, possibly due to limited healthcare access, lower awareness, and delayed diagnosis.The disparity in living environments emphasizes the need for targeted public health interventions in rural areas, including enhanced screening programs, increased awareness campaigns, and improved access to antiviral therapies. Moreover, environmental and lifestyle factors prevalent in rural settings, such as dietary habits, occupational exposure, and healthcare infrastructure limitations, may contribute to disease progression, warranting further investigation.
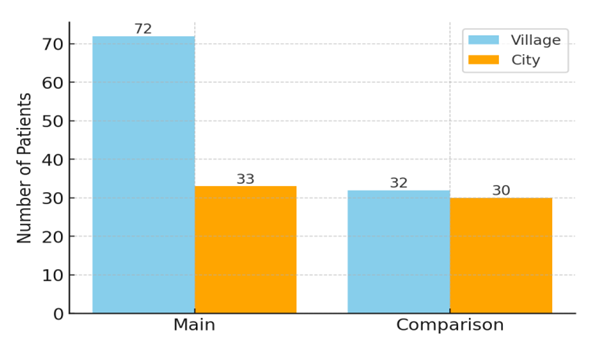 | Figure 1. Lifestyle of patients |
4. Discussion
- Preventive strategies such as antiviral therapy (e.g., pegylated interferon and bulevirtide), lifestyle interventions (dietary modifications, alcohol cessation), and HBV vaccination play a crucial role in mitigating HDV-associated cirrhosis. Immunological monitoring and early intervention significantly improve prognosis. Emerging treatments, including novel entry inhibitors and RNA interference therapies, offer new hope in HDV management.
5. Conclusions
- Comprehensive preventive measures, including antiviral therapy, vaccination, public health campaigns, and lifestyle modifications, are essential to reduce HDV-related liver cirrhosis. Further studies are required to explore novel immunotherapeutic approaches and enhance accessibility to effective treatments worldwide.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML