-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 1178-1180
doi:10.5923/j.ajmms.20251504.65
Received: Feb. 18, 2025; Accepted: Mar. 22, 2025; Published: Apr. 24, 2025

Cardiovascular Damage in Acute Pneumonia in Children
Karimjanov IA , Mirrakhimova MX, Gaziyeva A., Israilova NA
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2025 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

From the development of criteria for the diagnosis of damage to the cardiovascular system in acute pneumonia in childrenimproving the methods of treatment of this pathology and using new ones is one of the urgent tasks of pediatrics. In early childhoodmyocarditisit is necessary to study the clinical characteristics of the course of acute pneumonia complicated by Also various diseasesdecreased reactivity of the child's organism associated withIt is important that the risk factors for the development of cardiovascular system injuries in young children with acute pneumonia.
Keywords: Cardiovascular system, Children, Pneumonia, Complications
Cite this paper: Karimjanov IA , Mirrakhimova MX, Gaziyeva A., Israilova NA , Cardiovascular Damage in Acute Pneumonia in Children, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1178-1180. doi: 10.5923/j.ajmms.20251504.65.
1. Introduction
- Viral-microbial infections of the respiratory tract make up 10-15% of the causes of children's death in the world [2,5]. Severe pneumonia in young children is an indication for urgent intensive care. In complicated pneumonia, changes in the cardiovascular system are also observed, and a joint infectious-inflammatory process is observed. Cardio- and hemodynamic disorders in pneumonia in children of early age, as the main link of pathogenesis, aggravate its course, worsen the outcome, and often (in 5-50% of cases) become one of the causes of death [1].WorldwideAmong the exogenous factors leading to the development of myocarditis, a number of scientific studies aimed at determining the superiority of viral infectious-allergic diseases (53%) and increasing the scientific and practical effectiveness of the obtained results are being carried out [2,3,4]. In this regard, it is important to determine the structure of cardiovascular system disorders in acute pneumonia in children, to develop methods for its early diagnosis and pathogenetically based treatment measures. Evaluating the clinical course of myocarditis due to acute pneumonia at an early age, determining the consequences and risk factors for the development of myocarditis, improving the methods of treatment of this pathology and developing new ones are urgent tasks of pediatrics.
2. The Purpose of the Study
- It consists in developing criteria for diagnosing damage to the cardiovascular system in acute pneumonia in children aged 6-12 years.
3. Results of the Study
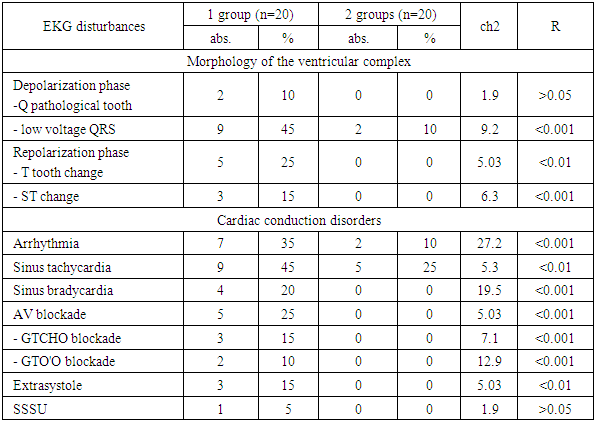
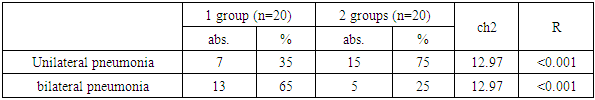
- The study is based on clinical and laboratory examinations of 40 children who were treated inpatiently in the pediatric pulmonology department of the 1st clinic of the Tashkent Medical Academy for acute pneumonia in 2021-20223.They were divided into 2 groups: group 1: 20 children with acute pneumonia complicated by myocarditis; Group 2 consisted of 20 children with acute pneumonia without myocarditis. The comparison group consists of 20 practically healthy children of the same age.The study of the risk factors for the development of myocarditis in early-aged children with acute pneumonia showed that the following are most important in the occurrence of this complication: the transmission of cardiovascular pathology from generation to generation, severe gestosis, nephropathy during pregnancy, anemia, ARVI, complications during childbirth, birth asphyxia, GIE, background diseases - OEYe, anemia, thymomegaly, allergies, the presence of retransmitted pneumonia and sepsis.The following are the characteristic features in the course of acute pneumonia complicated by myocarditis in children of early age: lethargy, rapid fatigue, profuse sweating, restlessness, complaints of disturbed sleep, pallor of the skin, peripheral cyanosis, shortness of breath with the involvement of additional muscles. such as intensification of symptoms of hypoxia, prolongation of the return of symptoms of the main disease. Enlargement of heart borders, reduction of heart tones, bradycardia, hepatomegaly, signs of circulatory disordersestablished specific cardiological symptoms in children of early age with acute pneumonia. Typical laboratory features for pneumonia complicated by myocarditis in children of early age are a strong development of anemia, leukocytosis, an increase in the amount of AST and de Ritis coefficient. Violation of the activity of myocardial enzymes in the blood serum is an indicator of a complex process that includes the activation of the body's protective-adaptive reactions, changes in the metabolism of cardiomyocytes, and injury to the myocardium. This process, which develops due to inflammation or non-inflammatory alteration, hypoxia and other factors, is aimed at maintaining biological homeostasis.The presence of bilateral focal-combining pneumonia, KTII and IIprogressive enlargement is the X-ray features of pneumonia complicated by myocarditis in children of early age. In the ECG examinationSinus tachycardia - simultaneous disturbance of rhythm and conduction in the form of bradyarrhythmia, incomplete blockade of the right leg of the bundle of Hiss, a decrease in the amplitude of the teeth of the QRS complexfor myocarditisis characteristic (Table 1).
|
|
4. Conclusions
- 1. Development of signs of hypoxia (cyanosis - 60%, paleness of the skin - 70%), shortness of breath with the involvement of auxiliary muscles– 55%, rapid fatigue - 80%, laxity - 40%, profuse sweating - 30%, restlessness, restless sleep - 50%, bilateral inflammatory process– 35%) in early age childrenmyocarditisare clinical features of acute pneumonia complicated by.2. Aggravated heredity for cardiovascular diseases - 40%, extragenital pathology in the mother during pregnancy- 85%, perinatal pathology in the child - 45%, transferred (pneumonia - 50%) and concomitant diseases (anemia - 75%, protein-energy deficiency - 65%, thymomegaly - 30%) decreased reactivity of the child's organism associated withrisk factors for the development of cardiovascular system injuries in children of early age with acute pneumonia.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML