-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 1169-1173
doi:10.5923/j.ajmms.20251504.63
Received: Apr. 1, 2025; Accepted: Apr. 17, 2025; Published: Apr. 24, 2025

Effectiveness of Molecular-Genetic and Bacteriological Research Methods in Drug-Resistant Forms of Pulmonary Tuberculosis
Jumaev Mukhtor Fatullaevich
Bukhara State Medical Institute, Department of Phthisiology and Pulmonology, Bukhara, Uzbekistan
Correspondence to: Jumaev Mukhtor Fatullaevich , Bukhara State Medical Institute, Department of Phthisiology and Pulmonology, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2025 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Numerous scientific studies on the effectiveness of treatment are being conducted worldwide. The issue of drug resistance of Mycobacterium tuberculosis is the subject of numerous studies by domestic and foreign authors. The meaning of the term drug-resistant strain has changed as knowledge about the mechanisms of drug resistance formation has accumulated. At the stage of introducing anti-tuberculosis drugs, it was proposed to designate a strain as resistant if it was isolated from a patient for whom treatment did not improve. This approach lost its significance after the complete rejection of monotherapy. Currently, in our country, special attention is paid to the problems of improving the activities of the healthcare system, including a healthy lifestyle of the population, early diagnosis of diseases, treatment and prevention of tuberculosis.
Keywords: Molecular genetic diagnostics, Treatment effectiveness, Drug resistance, Tuberculosis
Cite this paper: Jumaev Mukhtor Fatullaevich , Effectiveness of Molecular-Genetic and Bacteriological Research Methods in Drug-Resistant Forms of Pulmonary Tuberculosis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1169-1173. doi: 10.5923/j.ajmms.20251504.63.
Article Outline
1. Introduction
- Tuberculosis (TB) remains a major global health challenge, particularly with the emergence of drug-resistant strains, such as multidrug-resistant (MDR) and extensively drug-resistant (XDR) Mycobacterium tuberculosis. The rise of these resistant forms complicates treatment strategies, leading to higher morbidity and mortality rates. Accurate and timely diagnosis is crucial for effective patient management and preventing further transmission.Traditional bacteriological methods, such as sputum smear microscopy and culture-based techniques, have been the cornerstone of TB diagnosis for decades. However, these methods have limitations, including long turnaround times and variable sensitivity, particularly in cases of drug resistance. In contrast, molecular-genetic techniques, such as polymerase chain reaction (PCR), whole-genome sequencing (WGS), and line probe assays (LPAs), offer rapid and precise detection of resistance-conferring mutations.This study evaluates the effectiveness of molecular-genetic and bacteriological research methods in diagnosing drug-resistant pulmonary tuberculosis. By comparing their sensitivity, specificity, speed, and clinical applicability, we aim to determine the optimal diagnostic approach for improving patient outcomes and TB control programs. The findings will contribute to the ongoing efforts to combat antimicrobial resistance in tuberculosis and enhance diagnostic protocols in high-burden settings.
2. Materials and Methods of the Study
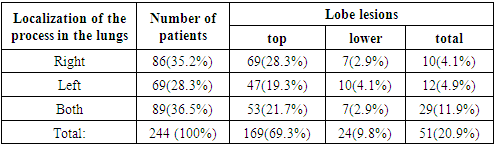
- The work is based on the data of examination of 244 patients from the southern regions of the Republic of Uzbekistan, who received treatment in the centers of phthisiology and pulmonology of the Bukhara region - 148 (60.7%), Navai region - 30 (12.3%), Kashkadarya region - 32 (13.1%) and Surkhandarya region - 34 (13.9%) cases in the period from 2016 to 2020.The age of patients ranged from 18 to 86 years, the average age was 52.1±2.9 years. Men were ill 2.2 times more often than women, and the incidence of patients was 65.2% at the age of 19-59 years (working age), 18.4% at 60-69 years and 16.4% over 70 years.It should be noted that the most frequent incidence of the disease occurred after forty years - 75.4% of patients and the peak age period was noted from 50 to 59 years in 23.4% of cases. Patients of the rural population were observed - in 185 (75.8%), the urban population - in 56 (23.0%) and homeless people - in 3 (1.2%) cases. When analyzing, it is noted that the disease was 3.3 times more common in rural populations. Of the 244 patients - 73 (29.9) patients had an employee profession, 13 (5.3%) - agricultural workers, 4 (1.6%) - students, a single (0.4%) case - medical personnel, and most often people without a certain job, who often do not undergo preventive medical examination - in 153 (62.8%) cases.
|
3. Results and Discussion
- When analyzing statistical data, it is noted that drug-resistant pulmonary tuberculosis, often develops in people living with chronic diseases, weakened immunity or with background diseases. The disease is most often detected in patients with concomitant diseases of the cardiovascular, hematopoietic, hepatobiliary system and diabetes. The clinical course was severe and the treatment of patients in this category was quite complex.In diagnostics and treatment of LU forms of pulmonary tuberculosis, bacteriological verification of mycobacteria with determination of sensitivity to anti-tuberculosis drugs plays a particularly important role. There is treatment without determination of sensitivity or bacteriologically without verification of diagnosis, based on indirect instrumental methods or clinical. In many cases, these irrational activities lead to the emergence of more resistant forms of mycobacterium tuberculosis, while the general condition of patients worsens. Targeted timely adequate treatment serves to cure this severe pathology and prevents its spread among the population.In modern times, molecular genetic research methods are a particularly important method for studying infectious diseases, as well as tuberculosis caused by Mycobacterium tuberculosis - Koch's shelf. PCR (polymerase chain reaction) diagnostics is based on the detection of mycobacterium DNA in pathological material, such as sputum, pus, pleural fluid, urine. The purpose of detection of the MTB complex + resistance to rifampicin and the determination of MDR-TB and there is no need for a separate detection stage, allows multiplexing, internal control can confirm negative results, high resolution, high specificity, very good reproducibility. Molecular genetic methods are used to multiply and detect genes of interest.
|
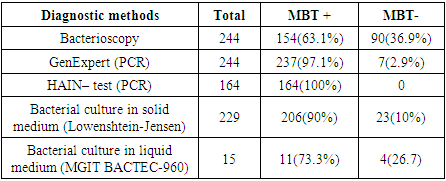
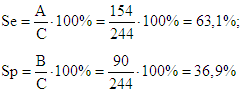 The sensitivity of bacterioscopic examination of sputum is 63.1%, and the specificity is 36.9%.PCR diagnostics were performed using the Genе / Xpert device – Mycobacterium tuberculosis DNA was detected in 244 (100%) patients and 237 (97.1%) cases.
The sensitivity of bacterioscopic examination of sputum is 63.1%, and the specificity is 36.9%.PCR diagnostics were performed using the Genе / Xpert device – Mycobacterium tuberculosis DNA was detected in 244 (100%) patients and 237 (97.1%) cases.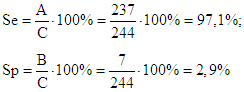 The sensitivity of molecular genetic testing of sputum on the GenExpert device is 97.1%, and the specificity is 2.9%.PCR diagnostics in the HAINtest device were performed in 164 (67.2%) cases and 100% of cases were positive. The most effective methods are those based on hybridization with DNA probes - DNA strip technology and the most widely used in the world is the HAIN test. This method allows: to differentiate mycobacteria of the tuberculosis complex - M.tuberculosis complex: M.tuberculosis, M.bovis, M.africanum, M.microti allows to determine drug sensitivity to isoniazid, rifampicin, fluoroquinolones, aminoglycosides, cyclic peptides and ethambutol.
The sensitivity of molecular genetic testing of sputum on the GenExpert device is 97.1%, and the specificity is 2.9%.PCR diagnostics in the HAINtest device were performed in 164 (67.2%) cases and 100% of cases were positive. The most effective methods are those based on hybridization with DNA probes - DNA strip technology and the most widely used in the world is the HAIN test. This method allows: to differentiate mycobacteria of the tuberculosis complex - M.tuberculosis complex: M.tuberculosis, M.bovis, M.africanum, M.microti allows to determine drug sensitivity to isoniazid, rifampicin, fluoroquinolones, aminoglycosides, cyclic peptides and ethambutol.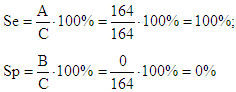 The sensitivity of the molecular genetic study of sputum on the HAINtest device is 100%, and the specificity is 0%. It should be noted that in these cases the study was carried out on patients who excrete MBT with sputum in 100% of cases.Sowing of pathological material was carried out on a solid Lowenstein - Jensen medium - in 229 (93.9%) patients and in 206 (90%) cases an increase in colonies of Mycobacterium tuberculosis was noted.
The sensitivity of the molecular genetic study of sputum on the HAINtest device is 100%, and the specificity is 0%. It should be noted that in these cases the study was carried out on patients who excrete MBT with sputum in 100% of cases.Sowing of pathological material was carried out on a solid Lowenstein - Jensen medium - in 229 (93.9%) patients and in 206 (90%) cases an increase in colonies of Mycobacterium tuberculosis was noted.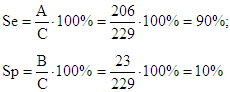 -Jensen solid medium culture method was 90%, and the specificity was 10%.Sowing pathological material on liquid BACTEC medium МGite 960 was performed – 15(6.1%) cases and 11(73.3%) cases had a positive result. Purpose of BACTEC МGite 960: Mycobacterium detection and recovery, principle: bacterial growth in appropriate liquid media, semi-automated liquid medium system, reduction of time to result - reduced from 8 weeks to 14 days.
-Jensen solid medium culture method was 90%, and the specificity was 10%.Sowing pathological material on liquid BACTEC medium МGite 960 was performed – 15(6.1%) cases and 11(73.3%) cases had a positive result. Purpose of BACTEC МGite 960: Mycobacterium detection and recovery, principle: bacterial growth in appropriate liquid media, semi-automated liquid medium system, reduction of time to result - reduced from 8 weeks to 14 days.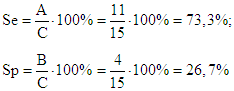 The sensitivity of sputum testing using the MGIT–BACTEC-960 liquid medium culture method was 73.3%, and the specificity was 26.7%.
The sensitivity of sputum testing using the MGIT–BACTEC-960 liquid medium culture method was 73.3%, and the specificity was 26.7%.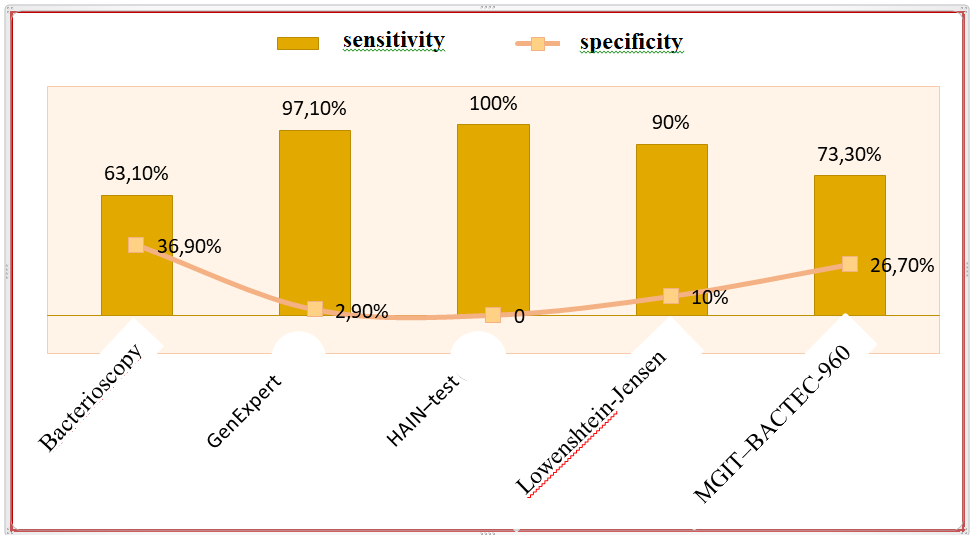 | Diagram 1. Comparison of sensitivity and specificity of bacteriological research methods |
4. Conclusions
- Timely diagnostics and adequate treatment of LU forms of pulmonary tuberculosis remains a very urgent problem in phthisiology and society. This section examines the clinical type of the disease, the mistakes made in both somatic and phthisiological medical institutions, the advantages and disadvantages of diagnostic research methods.The sensitivity of bacterioscopic examination of sputum is 63.1%, and the specificity is 36.9%.The sensitivity of molecular genetic testing of sputum on the GenExpert device is 97.1%, and the specificity is 2.9%.The sensitivity of the molecular genetic study of sputum on the HAINtest device is 100%, and the specificity is 0%. It should be noted that in these cases the study was carried out on patients who excrete MBT with sputum in 100% of cases.-Jensen solid medium culture method was 90%, and the specificity was 10%.The sensitivity of sputum testing using the MGIT–BACTEC-960 liquid medium culture method was 73.3%, and the specificity was 26.7%.Molecular genetic methods are highly effective diagnostic methods, this is due to the fact that PCR diagnostics detect mycobacterial DNA regardless of whether the mycobacteria are alive or dead, while bacteriological culture methods do not form colonies from dead mycobacteria.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML