-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 1067-1073
doi:10.5923/j.ajmms.20251504.44
Received: Mar. 20, 2025; Accepted: Apr. 10, 2025; Published: Apr. 12, 2025

Synthetic Cathinone Dependence and Suicidal Behavior: A Multi-Factor Analysis of Risk Factors
Ravshanov Jakhongir Azimjon Ugli1, Ashurov Zarifjon Sharifovich2, Abdukakharova Gulnoza Kurbanovna3, Khayredinova Inara Ilgizovna4, Tadjibaev Uktam Askarovich5, Sotnikova Olga Igorevna6
1Assistant, Department of Psychiatry and Narcology, Tashkent Medical Academy, Tashkent, Uzbekistan
2DSc, Professor, Department of Psychiatry and Narcology, Tashkent Medical Academy, Tashkent, Uzbekistan
3PhD Сandidate, Clinical Department for the Treatment of Drug Addiction and Substance Abuse, Republican Specialized Scientific-Practical Medical Center of Mental Health, Tashkent region, Uzbekistan
4PhD, Senior Lecturer, Department Psychiatry and Narcology, Tashkent Medical Academy, Tashkent, Uzbekistan
5PhD Сandidate, Clinical Department for the Treatment of Alcoholism, Republican Specialized Scientific-Practical Medical Center of Mental Health, Tashkent Region, Uzbekistan
6Medical Doctor, Department of Medical and Social Rehabilitation, Republican Specialized Scientific-Practical Medical Center of Mental Health, Tashkent Region, Uzbekistan
Correspondence to: Ravshanov Jakhongir Azimjon Ugli, Assistant, Department of Psychiatry and Narcology, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Synthetic cathinones (SC) use has been associated with severe psychiatric consequences, including an increased risk of suicidal behavior. This study investigates the relationship between SC dependence and suicidality risk. Methods: a retrospective observational cohort study was conducted at the Republican Specialized Scientific-Practical Medical Center of Mental Health in Uzbekistan from 2022 to 2024. The study included 138 patients, divided into two groups: 98 individuals with synthetic cathinone dependence (ICD-10: F15.2) and 40 individuals dependent on other psychoactive substances (pregabalin, gabapentin, carbamazepine, tropicamide). Suicidality risk was assessed using the Columbia-Suicide Severity Rating Scale (C-SSRS), and statistical analyses included logistic regression models, linear regression, and forest plot analysis to identify key risk and protective factors. Results: unadjusted analysis indicated a significant association between Alfa-PVP use and increased suicidality risk (OR = 2.76, p = 0.026). Other substances showed no significant effects on suicidality. However, after adjusting for demographic and psychosocial factors, no psychoactive substance remained a significant predictor of suicidality. Conclusions: while synthetic cathinones contribute to psychiatric instability, their direct effect on suicidality is overshadowed by psychosocial determinants. The findings emphasize the importance of family-centered interventions, mental health education, and targeted prevention strategies to mitigate suicidality risk among individuals with substance use disorders.
Keywords: Synthetic cathinones, Suicidality, Alfa-PVP, Pregabalin, Suicidal behavior, Substance use disorder, Psychosocial factors
Cite this paper: Ravshanov Jakhongir Azimjon Ugli, Ashurov Zarifjon Sharifovich, Abdukakharova Gulnoza Kurbanovna, Khayredinova Inara Ilgizovna, Tadjibaev Uktam Askarovich, Sotnikova Olga Igorevna, Synthetic Cathinone Dependence and Suicidal Behavior: A Multi-Factor Analysis of Risk Factors, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1067-1073. doi: 10.5923/j.ajmms.20251504.44.
1. Introduction
- The emergence and increasing prevalence of new psychoactive substances (NPS) have become a growing global concern [1]. One particularly alarming aspect is the expansion of the NPS market, which persists despite stabilization or even reductions in the use of internationally controlled drugs. A crucial factor contributing to this trend is the role of the Internet, which facilitates the rapid dissemination of NPS, particularly among younger demographics [2]. Among the most commonly distributed NPS categories, synthetic cathinones (SCs) have gained significant traction in the illicit drug market [3]. Given the widespread and growing consumption of these substances, a comprehensive evaluation of their consequences is imperative.In the past decade, synthetic cathinones have increasingly displaced traditional substances of abuse, drawing greater attention from researchers and public health officials [4]. Their widespread availability and affordability, coupled with misconceptions about their legality and perceived safety, contribute to their increasing use. Many users mistakenly believe that SCs pose minimal health risks, leading to an underestimation of their addictive potential and long-term consequences [5,6]. However, clinical observations frequently reveal that SC use often occurs alongside other substances, complicating both the clinical presentation and the severity of associated medical and social consequences [7]. Individuals consuming SCs often exhibit rapid-onset psychopathological changes, including neurotoxic damage to the central nervous system, personality deterioration, an increased likelihood of intoxication-induced psychosis, and severe behavioral disturbances [6].SC consumption has been linked to a notable rise in mortality rates among dependent individuals. These fatalities are not always solely attributed to somatic complications but may result from external factors such as accidental overdoses, life-threatening behavioral consequences, or suicides, which remain underexplored in scientific literature [8,9]. This underscores the necessity of a more thorough examination of the risk factors associated with SC dependence, with a particular focus on suicidal tendencies among affected individuals.Thus, the present study aims to examine the relationship between synthetic cathinone use and suicidal behavior.
2. Materials and Methods
- Study DesignThis study utilizes a retrospective observational cohort approach to examine the association between synthetic cathinone (SC) use and suicidal behavior. The research includes two patient groups who received treatment at the Republican Specialized Scientific-Practical Medical Center of Mental Health, under the Ministry of Health of the Republic of Uzbekistan, during the 2022–2024 period. Data were obtained from clinical records, patient questionnaires, and statistical analyses to ensure a comprehensive assessment.Study PopulationThe study included 138 patients, stratified into two groups: main group included 98 patients diagnosed with dependence on synthetic cathinones (ICD-10 code F15.2); comparison group consisted of 40 patients with dependence on other substances (such as pregabalin, gabapentin, carbamazepine or tropicamide). Comparison group was selected based on the similarity of clinical effects. Patients were selected based on pre-defined inclusion and exclusion criteria.Inclusion Criteria:1. Verified diagnosis of dependence on psychostimulants (ICD-10 code F15.2), established according to ICD-10 criteria.2. Age: Between 16 and 65 years.3. Informed consent to participate in the study.Exclusion Criteria:1. Presence of severe comorbid somatic diseases in the decompensation stage.2. Acute infectious diseases.3. Specific mental disorders, including:ο Epilepsy.ο Schizophrenia, schizotypal, and delusional disorders (ICD-10 codes F20–F29).4. Other psychotic disorders caused by alternative factors (e.g., traumatic brain injury).5. Refusal to participate in the study.Data Collection MethodsData collection was conducted using multiple methodologies. Clinical records and documentation were reviewed retrospectively, including psychiatric evaluations, substance use history, and treatment outcomes. Additionally, questionnaires and structured clinical interviews were administered, incorporating standardized tools to assess substance use patterns, suicidality, and psychosocial factors. The Columbia-Suicide Severity Rating Scale (C-SSRS) was employed to evaluate suicidality risk, while additional questionnaires were used to collect demographic information and substance use history.The confirmation of psychoactive substance use was based on a comprehensive verification process utilizing multiple data sources. Self-report questionnaires were initially used to document substance consumption patterns. To ensure objective validation, rapid urine drug screening was conducted to detect the presence of synthetic cathinones and other substances. Furthermore, medical records were examined to retrieve documented evidence regarding past substance use and prior treatment history.Independent and Dependent VariablesThe study analyzed multiple independent and dependent variables to explore the association between psychoactive substance use and suicidality risk. The independent variables included the type of psychoactive substances consumed, specifically Alfa-PVP, mephedrone, pregabalin, gabapentin, carbamazepine, and tropicamide. In addition, demographic characteristics such as age (evaluated both as a continuous and categorical variable) and gender (male/female) were taken into account.The primary dependent variable was the risk of suicidality, categorized into high-risk and low-risk groups. Classification was based on psychiatric evaluations and scores obtained from the Columbia-Suicide Severity Rating Scale (C-SSRS).Statistical Data AnalysisA multi-step analytical approach was employed to assess the relationship between synthetic cathinone (SC) use and suicidality risk. The analysis incorporated both unadjusted and adjusted statistical models, as well as visualization techniques to identify key predictors and potential risk factors.1. Unadjusted AnalysisTo establish a preliminary association between SC use and suicidality risk, odds ratios (ORs) and relative risks (RRs) were calculated. These measures provided insights into the likelihood of suicidal behavior among SC users compared to non-users. Additionally, chi-square tests were applied to assess differences between categorical variables, identifying significant demographic or behavioral patterns within the study population.2. Adjusted Logistic Regression ModelsTo account for potential confounding factors, logistic regression models were implemented. These models controlled for key sociodemographic variables, including age, sex, education level, family environment, and marital status. By adjusting for these factors, the study aimed to isolate the independent effects of SC and other psychoactive substances on suicidality risk, while considering the influence of psychosocial determinants.3. Linear Regression AnalysisFurther statistical evaluation was conducted using linear regression models to explore predictors of suicidality severity. The model fit was assessed using R², adjusted R², and F-tests, ensuring that the explanatory variables contributed meaningfully to the variance in suicidality risk. Additionally, ANOVA tests were used to identify the most significant predictors among sociodemographic and behavioral factors, providing a deeper understanding of the underlying determinants of suicidal behavior.4. Forest Plot AnalysisTo visually represent key findings, forest plot analysis was used to illustrate the relative influence of protective and risk factors associated with suicidality. This approach allowed for a clear and intuitive comparison of the variables contributing to increased or decreased suicidality risk.Statistical Significance and LimitationsA p-value < 0.05 was considered statistically significant for all analyses. While the study employed rigorous statistical techniques, multicollinearity was not explicitly tested, and sensitivity analysis was not conducted, which represents a limitation in the interpretation of the findings.Use of Large Language Models (LLMs)To refine the text in English and ensure proper citation formatting, Large Language Models (LLMs) were utilized.
3. Results and Discussion
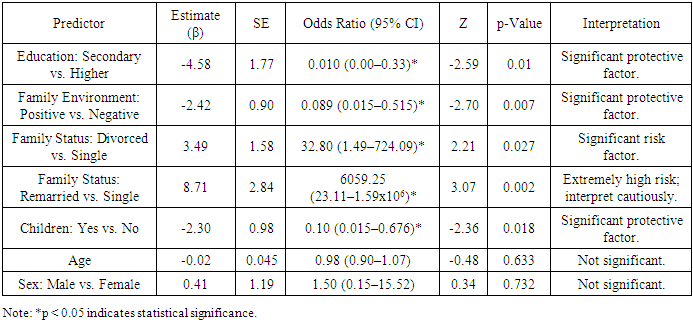
- Descriptive Statistics and Demographic Characteristics of the SampleThis study examined 138 patients, divided into two distinct groups based on their substance dependence. The main group consisted of 98 individuals diagnosed with synthetic cathinone dependence (ICD-10 code F15.2), while the comparison group included 40 patients with dependence on other psychoactive substances, such as pregabalin, gabapentin, carbamazepine, or tropicamide. By analyzing demographic factors, we aimed to identify potential differences between these groups.Age Distribution. The patients' ages varied widely, with a median age of 29 years across the entire sample. A closer look revealed a slight difference between groups: the median age in the main group was 30 years (with an interquartile range of 26 to 35 years), while in the comparison group, it was 28.5 years (ranging from 24 to 35 years). However, statistical analysis indicated that these variations were not significant, suggesting a similar age profile between the two groups.Sex Distribution. The vast majority of participants were male, accounting for 93.48% of the total sample. Specifically, men made up 90.82% of the main group and 100% of the comparison group. Interestingly, all nine female patients were found in the main group, with none in the comparison group. While this distribution suggests a possible trend, statistical analysis did not confirm a significant association between substance type and gender. Nevertheless, the predominance of male patients aligns with existing research indicating that men are more frequently diagnosed with substance dependence.Education Level. Educational backgrounds varied among the participants, with the majority having completed secondary special education (57.97%). A smaller portion had attained higher education (14.49%), while 20.29% had completed only secondary education. Additionally, 7.25% of patients had some incomplete higher education. When comparing the groups, the proportion of individuals with a university degree was slightly higher in the comparison group (20.00%) than in the main group (12.24%), though this difference was not statistically significant. These findings suggest that education level does not appear to play a decisive role in determining the type of substance a person becomes dependent on.Marital Status. The analysis of family status revealed that slightly more than half of the participants were married (52.90%), while a significant proportion remained single (36.96%). Additionally, 6.52% of the sample had experienced divorce, and 3.62% had remarried. When comparing the two groups, no meaningful statistical differences emerged, indicating that relationship status was not a distinguishing factor between patients with different substance dependencies.Substance Use and Suicidality Risk (Unadjusted Analysis)The initial analysis assessed the unadjusted associations between six substances and binary suicidality. Key results are summarized in Table 1, which reports odds ratios (OR), relative risks (RR), and the number needed to treat (NNT).
 | Table 1. Unadjusted Analysis of Substances' Impact on Binary Suicidality |
|
|
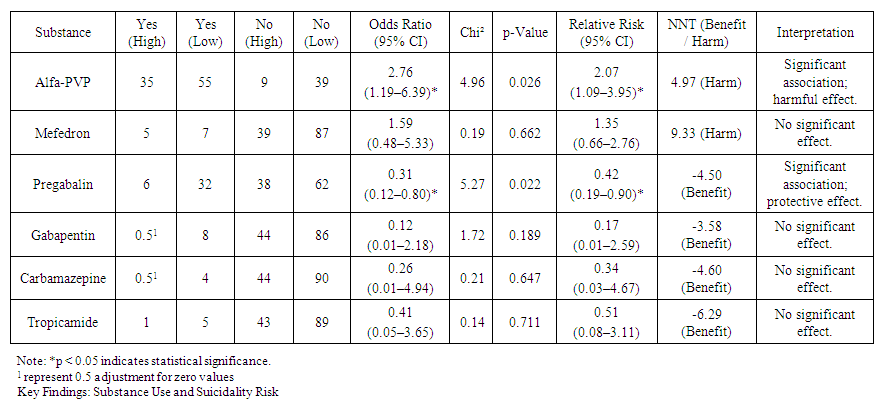
 | Figure 1. Forest Plot of Key Predictors from Fully Adjusted Model |
4. Conclusions
- The study highlights the multifaceted nature of suicidality, demonstrating that substance use alone is not a direct predictor but rather a factor that interacts with underlying social and psychological vulnerabilities. The strong impact of family dynamics, marital status, and parental roles suggests that addressing suicidality requires a shift from an individual-centered approach to a family-centered one.From a policy perspective, the findings emphasize the need for targeted prevention programs focusing on both substance use education and family resilience. In clinical practice, integrating family assessments into psychiatric care could enhance early detection and intervention for at-risk individuals. Finally, further research is needed to understand the long-term trajectories of suicidality, particularly in relation to early-life experiences and socio-cultural influences.By acknowledging the complex interplay of biological, psychological, and social factors, future interventions can become more effective, personalized, and impactful, ultimately reducing the burden of suicidality among vulnerable populations.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML