-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 1060-1062
doi:10.5923/j.ajmms.20251504.42
Received: Mar. 21, 2025; Accepted: Apr. 10, 2025; Published: Apr. 12, 2025

Morphological Characteristics in the Treatment of Multidrug-Resistant Pulmonary Tuberculosis and Optimization of Treatment Efficacy
Teshayev Shuhrat Jumayevich1, Usmonov Isomiddin Haydarovich2, Yitmasova Tuhfa Davlatovna1
1Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan
2Republican Specialized Scientific and Practical Medical Center of Phthisiology and Pulmonology, Tashkent, Uzbekistan
Correspondence to: Teshayev Shuhrat Jumayevich, Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Multidrug-resistant pulmonary tuberculosis (MDR-TB) remains a pressing global health challenge, with rising incidence rates and suboptimal treatment outcomes in many high-burden regions. This study conducts a comprehensive analysis of the histopathological and morphological alterations in lung tissue affected by MDR-TB, employing advanced imaging and microscopic techniques to characterize disease progression and tissue damage. Furthermore, we evaluate current treatment protocols through a systematic review of clinical outcomes, leveraging statistical data on treatment success rates, adverse drug reactions, and long-term patient recovery across different therapeutic regimens. By correlating morphological findings with clinical response data, this research identifies key pathological markers that influence treatment efficacy and proposes evidence-based strategies to optimize drug combinations, dosage adjustments, and adjunct therapies. The findings aim to contribute to the development of more effective, personalized treatment approaches for MDR-TB, ultimately improving patient survival rates and reducing the global burden of drug-resistant tuberculosis.
Keywords: Multidrug-resistant tuberculosis, Lung morphology, Treatment optimization, Histopathology, Drug resistance, Statistical analysis
Cite this paper: Teshayev Shuhrat Jumayevich, Usmonov Isomiddin Haydarovich, Yitmasova Tuhfa Davlatovna, Morphological Characteristics in the Treatment of Multidrug-Resistant Pulmonary Tuberculosis and Optimization of Treatment Efficacy, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1060-1062. doi: 10.5923/j.ajmms.20251504.42.
1. Introduction
- Tuberculosis (TB) is a widespread infectious disease, with MDR-TB posing severe therapeutic difficulties due to resistance to first-line drugs. According to WHO, approximately 500,000 new cases of MDR-TB are reported annually, with treatment success rates varying between 50-60% globally. Understanding the morphological changes in lung tissue during MDR-TB progression and treatment can provide insights into improving therapeutic interventions and increasing recovery rates [1].The problem of tuberculosis (TB), an infectious disease caused by Mycobacterium tuberculosis (MTB), has been known to humanity since ancient times and remains relevant even in the 21st century. TB is transmitted primarily through airborne droplets and airborne dust. The main source of infection in society is patients in whose sputum MTB is detected using conventional microscopy [3]. An effective measure to prevent the spread of TB is the treatment of patients who release the pathogen into the environment. One of the main methods of comprehensive treatment is anti-tuberculosis chemotherapy, which, when applied correctly, ensures recovery in patients with contagious forms of TB and interrupts the transmission pathways of the pathogen [2].Currently, the global community is seriously concerned about the increase in tuberculosis with multidrug-resistant Mycobacterium tuberculosis (MDR-TB) [4]. This disease is caused by MTB that is resistant to at least two primary anti-tuberculosis drugs, with possible resistance or susceptibility to other drugs [5]. The results of a study on resistance to anti-tuberculosis drugs conducted by the WHO and the International Union Against Tuberculosis and Lung Disease in 1994-1997 showed that 2.2% of TB cases worldwide were caused by MDR strains [6].Throughout the early 20th century, there were no effective medications for the treatment of tuberculosis. At that time, sanatorium treatment was practiced, including rest, fresh air, and enhanced nutrition, in the hope of spontaneous recovery [8-9]. Although some hospitalized patients showed improvement as a result of such therapy, long-term outcomes remained insufficiently favorable. More than 60% of patients discharged from hospitals died of tuberculosis within six years. The situation slightly improved after the development and implementation of surgical interventions such as artificial pneumothorax and thoracoplasty, which caused the collapse of affected lung areas [7].
2. Materials and Methods
- The study was conducted based on data from 184 patients with pulmonary tuberculosis exhibiting multidrug and extensively drug-resistant (MDR/XDR) strains. These patients underwent inpatient treatment at the Bukhara Regional Center for Phthisiology and Pulmonology, as well as at the Republican Specialized Scientific and Practical Medical Center for Phthisiology and Pulmonology, during the period from 2020 to 2023. The patients were carefully selected according to established inclusion criteria, which required laboratory-confirmed bacterial excretion and the presence of multidrug or extensively drug-resistant Mycobacterium tuberculosis. The age range of participants was from 18 to 75 years, including both men and women.All patients provided informed consent to participate in the study, ensuring compliance with all ethical standards. The study was approved by the Local Ethics Committee (LEC) of the Bukhara Regional Center for Phthisiology and Pulmonology, as well as the Republican Specialized Scientific and Practical Medical Center for Phthisiology and Pulmonology.Data from patients who did not meet the inclusion criteria were excluded from the analysis. The exclusion criteria included age below 18 or above 75 years, the presence of comorbidities in the stage of decompensation, pregnancy and lactation, HIV infection, generalized forms of tuberculosis, inability to undergo treatment, the necessity of surgical intervention at the time of study inclusion, as well as patient refusal to participate or participation in other studies.
3. Results
- The study, conducted at the Bukhara Regional Center for Phthisiology and Pulmonology and the Republican Specialized Scientific and Practical Medical Center for Phthisiology and Pulmonology, included 184 patients with multidrug and extensively drug-resistant tuberculosis pathogens. Among them, 112 were men (60.9%), and 72 were women (39.1%).Among the various clinical forms of tuberculosis, the most frequently diagnosed was fibrocavernous tuberculosis, which was identified in 68 patients (37%). The second most common form was infiltrative tuberculosis, recorded in 52 patients (28.3%). This was followed by disseminated tuberculosis in 34 patients (18.5%) and caseous pneumonia in 30 patients (16.3%).A study has shown that the spectrum of drug resistance of the tuberculosis pathogen in the examined patients is diverse. Bacteriological research data revealed significant resistance levels to various anti-tuberculosis drugs, as presented in Figure 1.
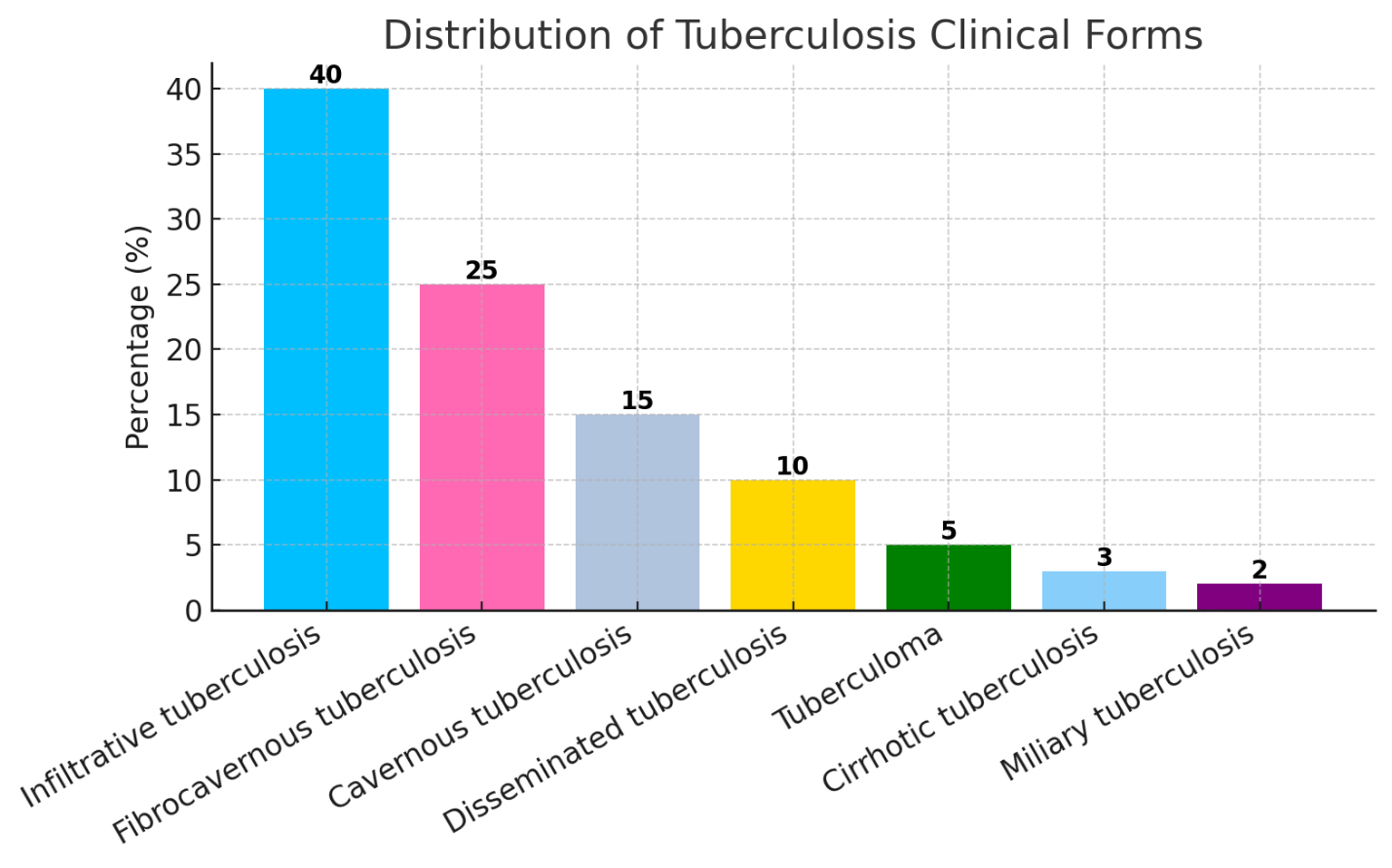 | Figure 1. Distribution of Clinical Forms of Pulmonary Tuberculosis Among Patients (%) |
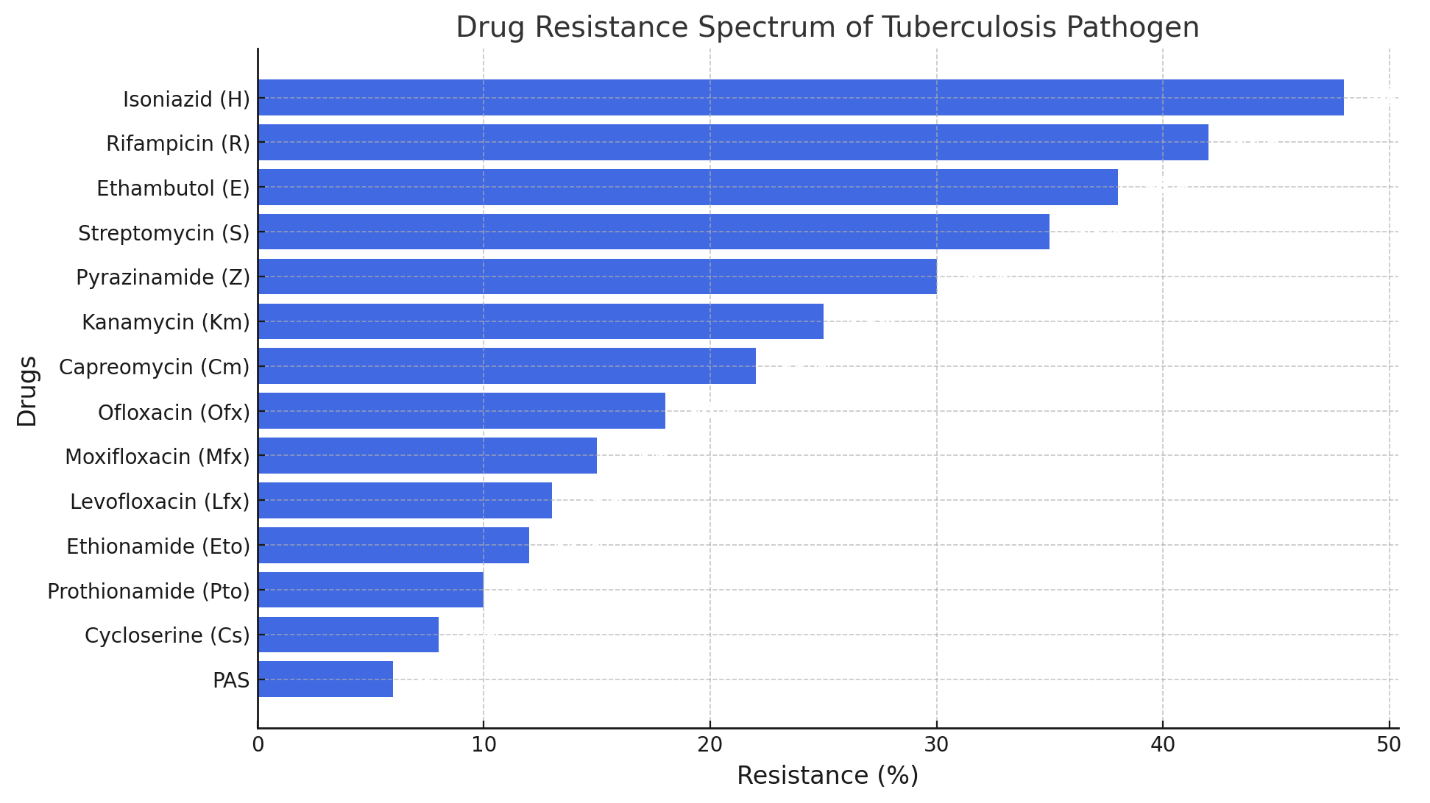 | Figure 2. Spectrum of Drug Resistance of Tuberculosis Pathogen |
4. Discussion
- Optimizing MDR-TB treatment requires a multi-faceted approach, including precise drug selection, host-directed therapies, and regular monitoring of morphological changes. Statistical analysis indicates that drug susceptibility-guided treatment leads to a 30% improvement in treatment success. The role of adjunct therapies such as immunomodulators and alternative antimicrobials (e.g., silver-based compounds) is also considered. Further studies on long-term lung function outcomes post-treatment are recommended.
5. Conclusions
- Morphological assessment of lung tissue provides critical insights into the progression and treatment response in MDR-TB. Statistical analysis supports that integrating histopathological evaluation with advanced therapeutic strategies can enhance treatment efficacy and patient outcomes, potentially increasing global MDR-TB treatment success rates.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML