-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 1050-1053
doi:10.5923/j.ajmms.20251504.40
Received: Jan. 9, 2025; Accepted: Feb. 8, 2025; Published: Apr. 12, 2025

Surgical Correction of Postoperative Ventral Hernias After Non-Tensioned Hernioalloplasty
Ismailov Obid Tashtemirovich, Sherbekov Ulugbek Akhrarovich
Samarkand State Medical University, Samarkand, Uzbekistan
Correspondence to: Sherbekov Ulugbek Akhrarovich, Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Relevance. The incidence of postoperative ventral hernia (PVH) in patients with hernias ranges from 3 to 19%. In patients after laparotomy, PVHs occur in 20-26% of cases and are the second most common after inguinal hernias. Purpose of the study. To improve the results of treatment of patients with recurrent postoperative ventral hernias by improving the methods of their surgical treatment. Material and methods. The study was carried out in Samarkand State Medical University at the department of general surgery and were treated in surgical departments of the city clinical hospital No.2 of Samarkand and multidisciplinary clinic of Samarkand State Medical University. Results and their discussion. Prosthetic tension plasty was not performed again among patients in group 2. Prosthetic non-tensioning plasty by improved methods was performed in all 26 patients with recurrence in 1 (3.8%) patient. In this case onlay hernioalloplasty without suturing the defect with implantation of the endoprosthesis with U-shaped sutures was performed in 18 patients (recurrence - 1), onlay+sublay hernioalloplasty without suturing the defect with creation of duplication in 8 patients. Clinical and statistical analysis of the results showed that the use of non-tensioned advanced methods of plasty in patients with recurrent ventral hernias after operations, prosthetic non-tensioned plasty significantly reduces the risk of recurrence of the disease up to 3.8%. Conclusions. In surgical treatment of postoperative ventral hernias it is recommended to use improved methods of hernioalloplasty - on lay without suturing the defect with implantation of endoprosthesis with U-shaped sutures (at W1-W2) or on lay+sub lay with creation of duplicate prosthesis (at W3-W4), which was performed in 56,9% and 19,8% of patients respectively. The proposed improved methods of non-tensioned prosthetic plasties in patients with recurrent ventral hernias allowed to improve significantly the results of treatment by reducing the recurrence of the disease to 3.8%.
Keywords: Postoperative ventral hernia, Recurrence
Cite this paper: Ismailov Obid Tashtemirovich, Sherbekov Ulugbek Akhrarovich, Surgical Correction of Postoperative Ventral Hernias After Non-Tensioned Hernioalloplasty, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1050-1053. doi: 10.5923/j.ajmms.20251504.40.
Article Outline
1. Relevance
- The incidence of postoperative ventral hernia (PVH) in patients with hernias ranges from 3 to 19% [4,7,11]. In patients after laparotomy, PVHs occur in 20-26% of cases and are the second most common after inguinal hernias [3,14]. In the USA more than 4 million laparotomies are performed annually for various indications, and 2-30% of patients develop PVH, which leads to 150-250 thousand herniorrhaphies per year. At the same time, more than 100 thousand patients require reoperations due to hernia recurrence [1,12]. In the Netherlands, according to national medical registry data, for every 100,000 laparotomies there are about 4,000 hernioplasty for PVH [8,12]. Ventral hernias of median localisation occur in 57-83% of patients. The number of reoperations due to PVH recurrences varies from 2.5 to 54.8% [2,5,8,9]. The causes of hernia recurrences after primary hernioplasty are diverse. They are divided into general predisposing factors associated with impaired reparative processes and a decrease in the general nonspecific reactivity of the organism; producing factors that weaken the abdominal wall and affect intra-abdominal pressure; local factors associated with surgery; and indirect factors caused by wound complications.
2. Purpose of the Study
- To improve the results of treatment of patients with recurrent postoperative ventral hernias by improving the methods of their surgical treatment.
3. Material and Methods
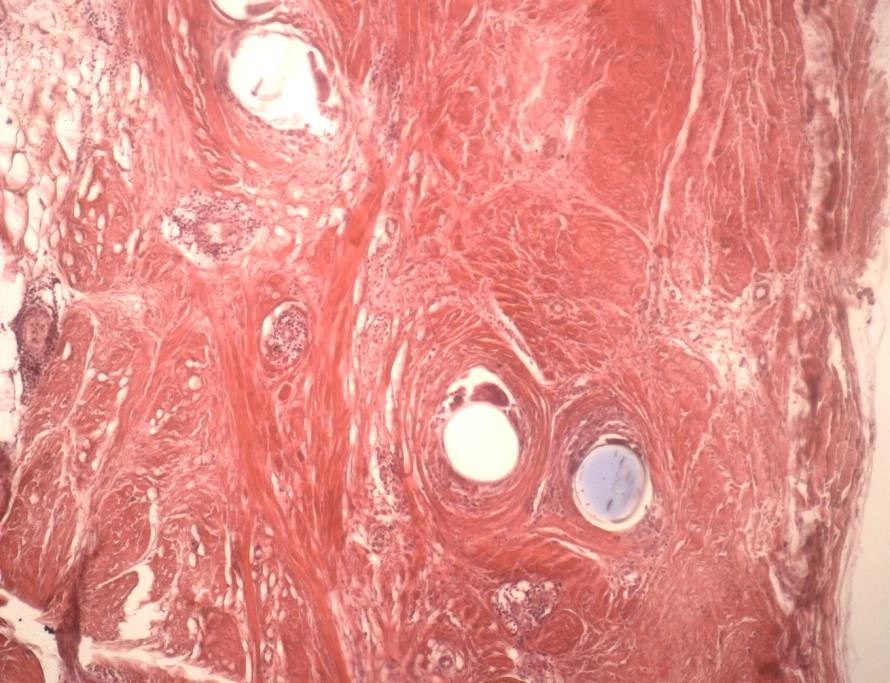
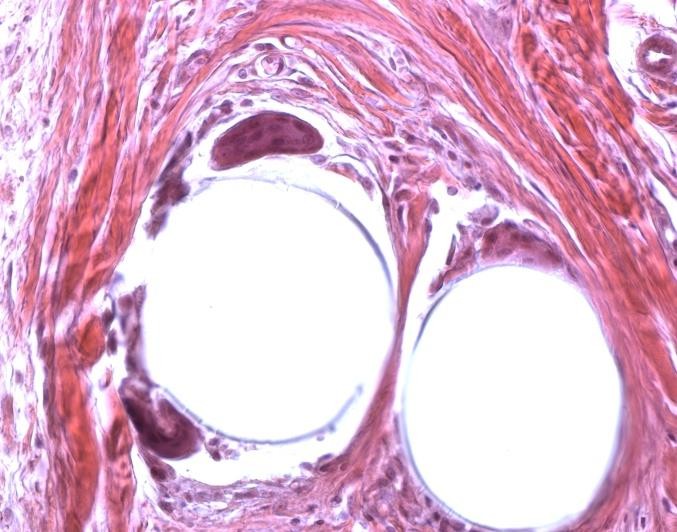
- The study was carried out in Samarkand State Medical University" at the department of general surgery and were treated in surgical departments of the city clinical hospital No.2 of Samarkand and multidisciplinary clinic of Samarkand State Medical University. All 26 patients aged from 30 to 68 years (the average age was 53,2±8,1 years) with recurrent postoperative ventral hernias, in whom the hernia recurrence developed after non-tensioned methods of hernioplasty. Of 26 patients, 22 had ventral hernias of median localization (epigastric - in 6 patients, mesogastric - in 2 patients, hypogastric - in 10 patients, in 4 patients localization was not specified). 2 patients had recurrent hernias of anterolateral and 2 - lateral localization’s.Recurrent hernias of small size (W1) were in 10 patients, medium (W2) - in 7 patients, large (W3) - 7 and giant (W4) - 2. It should be noted that hernia recurrences after prosthetic plasty by combined method were in patients with multiple recurrences after previous operations performed by different methods. Out of 26 patients 12 had 2 recurrences, 8 - 4, 2 - 8 and 4 - 14, which indicates significant abdominal wall tissue abnormalities contributing to the development of the disease recurrence.When performing surgery in patients with recurrent hernias after non-tensioned prosthetic combined plasty and skin dissection in the subcutaneous tissue, the prosthesis integrated into the tissue was clearly identified, forming the anterior walls of the vaginas of the rectus abdominis in case of midline hernias. Regardless of the location (epi-, meso-, hypogastric, as well as anterolateral, lateral) recurrent hernias were localized in 20 patients along the lower, in 4 - along the lower lateral, in 2 - along the upper contour of the prosthesis. Therefore, the hernia gate along the upper or lower contour was represented by the prosthesis, along the lower and upper contour - by the aponeurosis of rectus abdominis muscles, respectively, and the hernia sac was formed by overstretched peritoneum and hypertrophied transverse fascia. In none of the 26 observations, the hernia sac contained a prosthesis placed during the previous operation. No suture material could be found in the hernia gate at the site of prosthesis fixation, as the patients used resorbable suture material (Vicryl or polyglycolide) during surgery.The size of the hernia depended on the time of its onset. The longer the period was, the larger were the hernia sizes, increasing both due to the hernia gate and the hernia sac. Moreover, the hernial gate expanded along the lower contour due to stretching and tearing of the tissues from which the slippage of the prosthesis occurred. This is evidenced by the dense fibrous ring along its lower and lateral contours. On the upper contour the herniation ring was represented by the edge of the prosthesis without fibrous tissue sprouting into it.Clinical observations showed that in patients of group II recurrences developed within 6 months to 1.5 years. Intraoperatively it was confirmed that all recurrent hernias were incomplete and developed most often along the lower contour of the prosthesis fixation. Morphological studies of the recurrence zones showed that there was a thick capsule of mature connective tissue with fibrous transformation and diffuse focal lipomatosis around the prosthesis. The first "line of interaction" with the fibres of the material were giant cells of foreign bodies with the number of nuclei from 18 to 38 and only in one plane of the histological slice. Signs of granulomatous inflammation were in all observations, but the most pronounced in the places of fibre intertwining, which caused the presence of a 263+44.5 μm luft. The immediate zone of recurrence was represented by full-blooded granulation tissue moderately infiltrated with lymphocytes (Picture 1, 2).
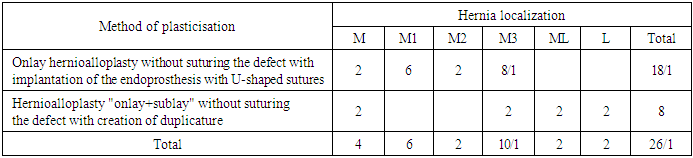
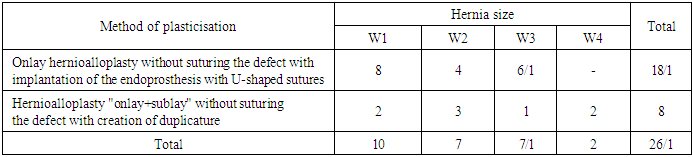
4. Results and Their Discussion
- Tables 1 and 2 present information about the methods and the number of operations performed on patients with hernia recurrences after non-tensioned prosthetic combined methods of plasty.
|
|
5. Conclusions
- 1. Clinical manifestations of the disease in patients with recurrent ventral hernias depend on the technique of previous hernioplasty. Partial recurrence of hernias along the lower and upper contours of fixation of the prosthesis to the tissues, as well as hernias through the defects of the damaged prosthesis are characteristic of the non-tensioned prosthetic method of plasty.2. Mature connective tissue with fibrous transformation phenomena, diffuse focal lipomatosis and moderate lymphocytic infiltration are characteristic in patients after non-tensioned combined methods of plasty. The above factors together with the increase in intra-abdominal pressure are the basis for the formation of hernia recurrence.3. In surgical treatment of postoperative ventral hernias it is recommended to use improved methods of hernioalloplasty - "on lay" without suturing the defect with implantation of endoprosthesis with U-shaped sutures (at W1-W2) or "on lay+sub lay" with creation of duplicate prosthesis (at W3-W4), which was performed in 56,9% and 19,8% of patients respectively. 4. The proposed improved methods of non-tensioned prosthetic plasties in patients with recurrent ventral hernias allowed to improve significantly the results of treatment by reducing the recurrence of the disease to 3.8%.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML