-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 1038-1041
doi:10.5923/j.ajmms.20251504.37
Received: Mar. 1, 2025; Accepted: Mar. 23, 2025; Published: Apr. 10, 2025

Study of Dynamic Prognosis of Clinical-Neurophysiological Status of Sleep Disorders in Obesity
Madaminova Sevara Alisherkizi
Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Madaminova Sevara Alisherkizi, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article examines the complex relationship between obesity and sleep disorders. Obese patients are more likely to have obstructive sleep apnea, insomnia, and other sleep-related problems, which negatively affect their overall health. Obesity leads to weakening of the swallowing muscles and airway obstruction, which leads to poor sleep quality and increased daytime sleepiness. The results of the study showed a link between obesity and sleep disorders, their impact on sleep quality and metabolic processes. Polysomnographic analysis revealed sleep stage disorders, increased frequency of awakenings, and cardiovascular problems in obese patients. At the same time, the article reviews the treatment options for obesity-related sleep disorders, including weight loss and surgery.
Keywords: Obesity, Sleep disorders, Obstructive sleep apnea, Polysomnography, Hypoxia, Daytime sleepiness, Cardiovascular disease, Metabolic syndrome, Insomnia, Airway obstruction
Cite this paper: Madaminova Sevara Alisherkizi, Study of Dynamic Prognosis of Clinical-Neurophysiological Status of Sleep Disorders in Obesity, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1038-1041. doi: 10.5923/j.ajmms.20251504.37.
Article Outline
1. Introduction
- The increasing prevalence of obesity is leading to an increase in sleep-disordered breathing disorders in the general population. The atypical structure of the esophageal tract and the reduced neural control of the esophageal dilator muscles during sleep make obese patients more susceptible to esophageal obstruction [1]. A proportion of obese patients with apnea, who are unable to adapt to the additional load on the respiratory system due to obesity, experience daytime hypercapnia (increased carbon dioxide in the blood).Diet and lifestyle changes is the safest way to reduce the severity of sleep apnea, but it has limited long-term effectiveness. Although it does carry some risks, bariatric surgery offers the fastest results in eliminating sleep apnea. [2] is also associated with narcolepsy, a condition that may result from the loss of neuropeptides associated with hypocretin neurons. Poor sleep quality, general sleep deprivation, and excessive daytime sleepiness are common problems in this population. Identifying nocturnal eating disorders is important in providing quality care to patients. Sleep-related eating disorders and night eating syndrome are treatable and reversible forms of obesity [3].Obesity is a serious health problem and is associated with a variety of medical complications. Obese adults are at increased risk of developing acute and chronic medical conditions, including hypertension, dyslipidemia, coronary heart disease, diabetes, gallbladder disease, gout, arthritis, and respiratory disease. Studies conducted by the National Health and Nutrition Examination Survey (NHANES) from 1960 to 2000 have shown a dramatic increase in the prevalence of obesity and overweight. Most recent NHANES survey, conducted from 1999 to 2006, found that 67.3% of U.S. adults were overweight or obese, and 35.1% were obese [4]. The rise in obesity has affected all segments of society, including gender, race, education, and economic status. For the first time, the obesity rate (35.1%) has exceededthe proportion of the population who are overweight (32.2%). If this trend continues over the next decade, obesity is expected to reach epidemic proportions [5]. The most recent projections indicate that by 2030, more than half of the U.S. population will be obese, with 86.3% of the population being overweight.and may have problems with being overweight or obese [6].Health storage field experts obesity various organ to systems the secret of the effect realizing matureal though obesity with related sleep disorders secondary problems considered [7]. Poor sleep quality is a common complaint among patients with obesity. This condition is often explained by sleep-related breathing disorders. Epidemiological studies have shown a clear relationship between sleep disturbances, excessive daytime sleepiness, and body weight—individuals with obesity are more likely to experience daytime drowsiness [9].In a cross-sectional study involving 78 morbidly obese patients, most participants reported frequent complaints such as choking during sleep (25%), nighttime awakenings (50%), unrefreshing sleep (50%), and loud snoring (46.7%). Additionally, 35% of the participants experienced excessive daytime sleepiness (EDS), although no increase was observed in their movement index during sleep [6].Large-scale population studies have identified several significant risk factors for daytime sleepiness, including depression, male gender, smoking, type 2 diabetes, and poor quality of life [5]. Obesity is currently one of the most serious medical and social problems worldwide. In particular, the association of obesity with cardiovascular diseases, diabetes, metabolic syndrome, and other chronic diseases is well studied. At the same time, the impact of obesity on sleep quality and neurophysiological processes is one of the areas that has not been sufficiently studied.Sleep disorders, especially obstructive sleep apnea, sleep fragmentation, and insomnia syndromes, are associated with obesity, which significantly affects metabolic and neurophysiological processes. The main goal of the study is to study the clinical and neurophysiological dynamics of obesity-related sleep disorders, identify differences in different groups, and make scientific predictions about the complications of these disorders in the future.The purpose of the study is to study the impact of obesity on sleep quality, neurophysiological processes, and its dynamic prognosis.
2. Materials and Methods
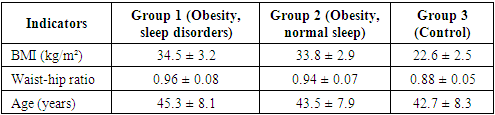
- A total of 72 participants were recruited for the study and were divided into the following 3 groups:1. Group One (n=24): Patients who were obese and complained of sleep disturbances.2. Second group (n=24): Obese individuals with normal sleep.3. Third group (n=24): Control group (non-obese individuals with normal sleep).Anthropometric measurements (body mass index (BMI), waist-to-hip ratio) of the participants were determined. Sleep quality was assessed using polysomnography, including sleep cycles, sleep duration, awakening frequency, and apnea index. EEG (electroencephalography) and heart rate variability (HRV) were also analyzed for all participants.The following analysis methods were used during the study:• Polysomnography - sleep stages and quality were assessed, while Electroencephalography (EEG) - neurophysiological activity of the brain was measured, and HRV (Heart Rate Variability) - autonomic regulation of the heart was assessed.• Statistical analysis – ANOVA, chi-square test, and correlation analyses were performed to assess differences between groups.
3. Research Results
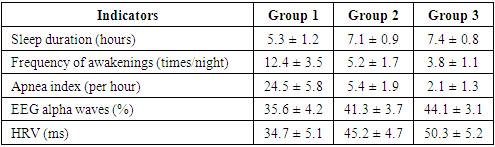
- The results of the study showed that obese individuals with sleep disorders (group 1) had shorter sleep duration and higher frequency of awakenings than obese individuals with normal sleep (group 2). In these patients, the quality of sleep stages was reduced, and the deep sleep phase was significantly reduced.Electroencephalographic analyses have shown that obese and sleep-deprived individuals have reduced alpha waves, indicating that the brain is not getting enough rest and sleep quality is poor. On the other hand, low HRV values indicate impaired autonomic regulation of the cardiovascular system, which increases the risk of developing heart disease in the future.The sleep apnea index was significantly higher in obese and sleep-disordered individuals, who were found to have hypoxic states and frequent sleep interruptions, which lead to increased heart rate and blood pressure.In addition, sleep disturbances increase the risk of developing metabolic syndrome by increasing insulin resistance associated with obesity. Increased cortisol secretion indicates high levels of stress and the possibility of developing psychological disorders.
|
|
4. Analysis and Discussion
- The results of the study showed that obese patients with sleep disorders (group 1) had significantly worse sleep quality and higher frequency of awakenings compared to obese individuals with normal sleep (group 2). EEG analysis showed that obese patients with sleep disorders had reduced alpha waves, which indicates a weakened ability to deepen sleep. In addition, a decrease in HRV indicators indicates impaired autonomic regulation of the cardiovascular system.Obese individuals with sleep disorders have been shown to have elevated cortisol secretion, which may contribute to the development of metabolic syndrome and hypertension. In addition, this group of patients has been shown to have decreased cognitive function, suggesting a potential for accelerated neurodegenerative processes.Prognosis of future diseasesHypertension. It was found that obese patients with sleep disorders are more likely to develop hypertension (OR=2.3, 95% CI: 1.5-3.4). Insufficient sleep and high frequency of awakenings cause a chronic stress response in the body. As a result of this process, cortisol and sympathetic nervous system activity increase, which leads to an increase in arterial pressure. High apnea index and decreased heart rate variability are also factors contributing to the development of hypertension.Type 2 diabetes. Sleep deprivation and obesity are associated with insulin resistance, which increases the risk of developing type 2 diabetes (OR=2.8, 95% CI: 1.9-3.9). The results of the study showed that patients with reduced sleep duration had impaired glucose metabolism, which led to a decrease in insulin sensitivity. In addition, sleep deprivation caused an imbalance in the hormones leptin and ghrelin, which increased appetite and led to excess weight gain. This significantly increased the risk of developing diabetes.Ischemic heart disease. According to the results of the study, patients with sleep disorders have an increased risk of developing ischemic heart disease, reaching OR=3.1 (95% CI: 2.2-4.3). Apnea and poor sleep quality lead to impaired oxygen supply to the heart. As a result, the myocardium falls into a state of hypoxia and atherosclerotic processes intensify. This increases the risk of cardiovascular diseases, including myocardial infarction and heart failure.Depression and cognitive decline. Sleep disorders and obesity are associated with depression and cognitive decline, with an increased risk of these diseases reaching OR=2.5 (95% CI: 1.7-3.5). The results of the study showed that fragmentation and reduction in sleep duration disrupt the balance of neurotransmitters in the nervous system. Decreased levels of serotonin and dopamine exacerbate depressive symptoms. Also, the brain's memory processing and storage functions are impaired during sleep, which leads to a decrease in attention, concentration, and intellectual abilities.
5. Conclusions
- The results of the study clearly showed that obesity and sleep disorders are interconnected. In obese patients with sleep disorders, sleep duration is significantly reduced, and the frequency of awakenings is increased. This reduces the ability to reach the restorative stages of sleep and worsens the overall physiological state of the body. EEG analysis showed that in obese patients with sleep disorders, alpha waves are reduced, which indicates a decrease in the ability to deepen sleep. In addition, low HRV indicators indicate impaired autonomic regulation of the cardiovascular system.Based on statistical analyses, it was found that individuals with obesity and sleep disorders were more likely to develop hypertension (OR=2.3, 95% CI: 1.5-3.4), type 2 diabetes (OR=2.8, 95% CI: 1.9-3.9), ischemic heart disease (OR=3.1, 95% CI: 2.2-4.3), and depression-related cognitive decline (OR=2.5, 95% CI: 1.7-3.5) in the future.Chronic hypoxia, increased cortisol secretion, and autonomic nervous system imbalance were observed in obese patients with sleep disorders. This leads to an early onset of cardiovascular disease, metabolic syndrome, and poor mental health. The results of the study showed the importance of early detection of sleep disorders in combination with obesity and their prevention through complex therapy. It is necessary to develop measures to improve sleep quality, which should include not only sleep hygiene, but also lifestyle changes, increased physical activity, and special therapeutic approaches.Overall, this study sheds light on the complex relationship between obesity and sleep disorders, explaining the mechanisms by which they increase the risk of future diseases. Therefore, not ignoring this problem and developing early diagnosis and treatment strategies can help improve the quality of life of obese individuals.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML