Pulatova Shakhzoda Karimovna
Assistant of the Department of Surgical Dentistry, Abu Ali Ibn Sina Bukhara State Medical Institute, Uzbekistan
Correspondence to: Pulatova Shakhzoda Karimovna, Assistant of the Department of Surgical Dentistry, Abu Ali Ibn Sina Bukhara State Medical Institute, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The study groups included 157 patients with mandible fractures, including 121 men and 36 women. The scientific and practical novelty of the work lies in the fact that the intermaxillary fixation of the victims of the main group was carried out by means of orthodontic mini-implants, known in the literature as cortical screws. In addition, local treatment of patients in this group was supplemented by the action of an infrared laser and the use of Traumeel-S ointment. The correctness of the choice of tactics for the complex treatment of patients with fractures of the lower jaw is substantiated by the indicators obtained as a result of the various research methods presented in the article.
Keywords:
Mandibular fractures, Stimulation of non-specific protective factors, Oral microflora, Consolidation of fragments, Rehabilitation period
Cite this paper: Pulatova Shakhzoda Karimovna, Rationale for the Correctness of the Tactics of Combined Treatment of Victims with Mandibular Bone Fractures, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1031-1037. doi: 10.5923/j.ajmms.20251504.36.
1. Introduction
In connection with the increase in the level of technical equipment of society, the growth of external traumatic factors, the treatment of non-gunshot fractures of the lower jaw is an urgent task of clinical maxillofacial surgery [5,4,9]. According to WHO estimates, facial bone fractures account for about 3% of all human skeletal bone injuries. Isolated injuries to the lower jaw are the most common type of facial bone fracture. Hese data do not show a downward trend and account for up to 85% of cases. Road traffic accidents account for more than 50%, falls from height 25%, and domestic trauma up to 20%.Workplace injuries account for only 4%, accidental gunshot wounds more than 1%, and other injuries less than 1%.According to the majority of authors, the age range in which the largest number of mandibular fractures occur is from 18 to 40 years [1,6,8].The lower jaw is a unique bone in its structure, which is the only movable bone in the facial skeleton, which is a massive arch. All parts of the lower jaw are covered with a thin layer of soft tissue and are the most protruding parts of the human body, therefore they are more often subject to injury. The weaker parts of the mandible are the midline of the body of the jaw, the canine region, the angle region and the base of the condylar process. It is in these places that a fracture often occurs due to mechanical impact. The complex geometry of the lower jaw and its mobility predispose to reflected, indirect fractures with significant displacement of fragments, and the location of the jaw in the lower part of the face creates more conditions for mechanical damage [2,7,10].The main condition for treating patients with fractures of the lower jaw is to create immobility of bone fragments, consolidate the fragments in the correct position in the shortest possible period, create favorable conditions for the course of reparative regeneration in bone tissue and prevent complications in surrounding tissues. The volume of therapeutic treatment of patients with mandibular fractures is extremely high, which makes it difficult for narrow-profile specialists to choose the correct management tactics and leads to monotherapy. This is a reason for the development of new fundamental clinical and theoretical studies [3,8,9,10].Taking into account the above, it becomes obvious that it is advisable to develop new gentle methods of conservative treatment of patients with fractures of the lower jaw, their systematization and algorithm within the framework of complex therapy.The aim of the study is to investigate the effectiveness of methods of complex treatment of patients with fractures of the lower jaw with the inclusion of bioregulatory and physiotherapy in its local component against the background of immobilization of the jaws using cortical screws.
2. Materials and Methods
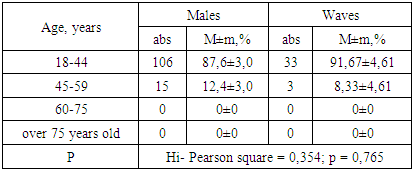
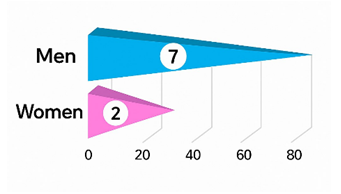
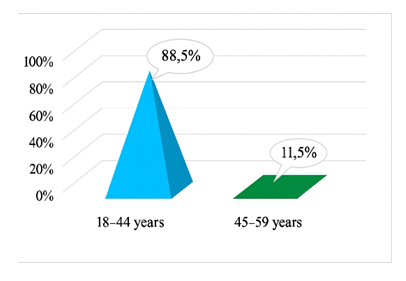
Clinical studies were conducted on the basis of the maxillofacial surgery department of the Bukhara Regional Multidisciplinary Medical Centre. Observations were based on clinical and laboratory study of 157 patients diagnosed with mandibular fracture (single, double and multiple; unilateral and bilateral), of which:• 1stgroup: 46 patients (29.30%)• 2ndgroup: 54 patients (34.39%)• 3rdgroup: 57 patients (36.31%).Among the total number of patients, males were 121 (77.07%) and females were 36 (22.93%) aged between 18 and 60 years. The control group included 30 conditionally healthy individuals. As shown in Table 1, mandibular fractures were more common in those aged 18 to 44 years (65% of patients). 85% of the hospitalised patients were admitted for emergency indications. All cases of mandibular fractures had different origins. The main cause of mandibular fracture was trauma due to impact or fall. Such injuries could occur in a variety of situations, such as car accidents, sports injuries, fights, or workplace accidents. Often, a mandibular fracture could occur from a fall on the chin due to the head hitting a hard surface (in epileptic patients). Also, mandibular fractures have been observed in people over 60 years of age due to age-related changes in bone tissue.Table 1. Distribution of patients of the examination groups (n=157) by sex and age
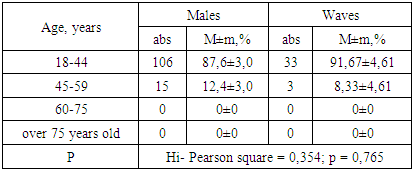 |
| |
|
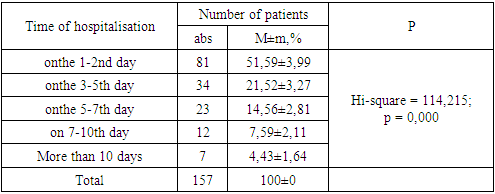
Analysis of the average hospitalisation time (Table 2) showed that the greatest number of referrals occurred on the 1-3rd day after injury. This is due to the fact that in the first days after the injury, patients seek medical assistance from emergency physicians and traumatologists. After that, in the presence of complex fractures or complications, they were referred to the maxillofacial surgery department for treatment.Table 2. Periods of hospitalisation of patients with mandibular fractures (n=157) from the moment of injury
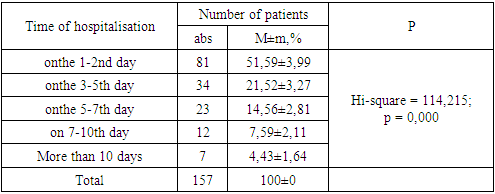 |
| |
|
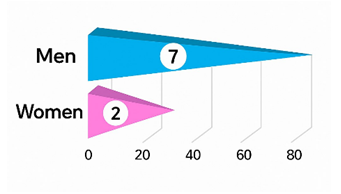 | Figure 1. Distribution of patients by gender (%) |
It was also observed that some patients presented on the 7th-10th day after injury, indicating a delay in receiving medical attention. This can lead to additional complications and longer treatment and rehabilitation times.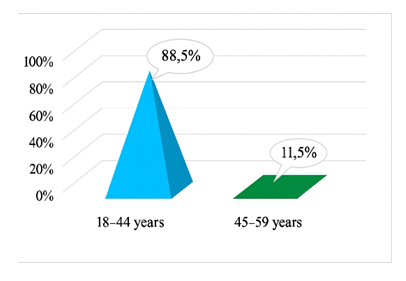 | Figure 2. Distribution of patients by age (%) |
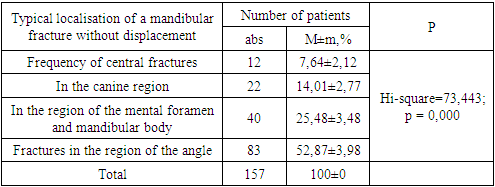
The average hospitalisation period was 7-10 days, with some patients being treated for up to 2-3 weeks, depending on the severity and nature of the fracture.The study of mandibular fracture localisation revealed that in the majority of patients, the fracture line is located in the angle region (52.5% of cases), followed by fractures in the mental foramen and mandibular body (25.4% of cases, respectively), with fractures in the canine region occurring less frequently (13.9%). The frequency of central fractures is 8.2% (Table 3).Table 3. Distribution of patients (n=157) by localisation of mandibular fracture within the dentition at the time of patient hospitalisation
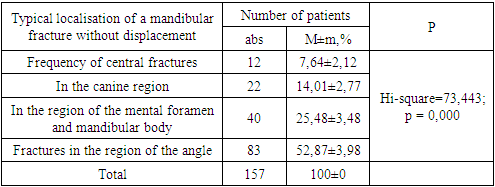 |
| |
|
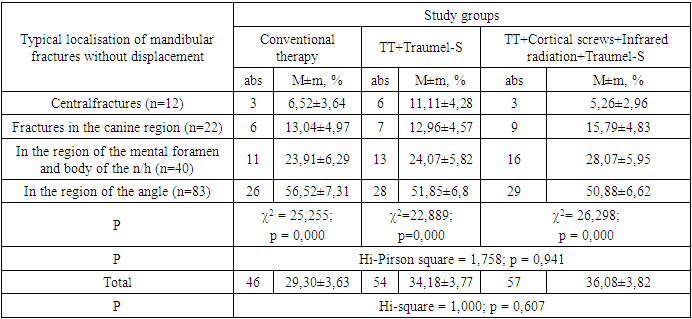
Based on the objectives of the study, 157 patients with mandibular fractures were randomly divided into 3 groups depending on the type of local therapy (Table 4):Table 4. Distribution of patients by study groups (n=157) depending on the applied complex of local treatment
 |
| |
|
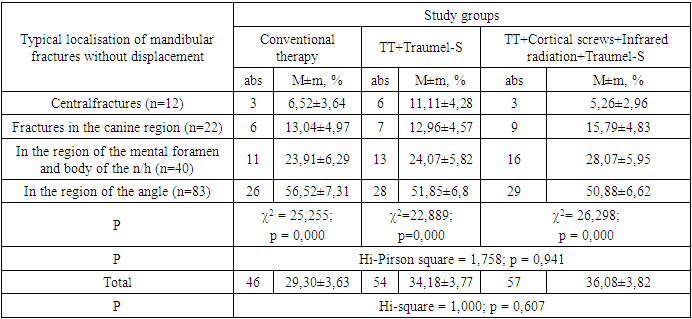
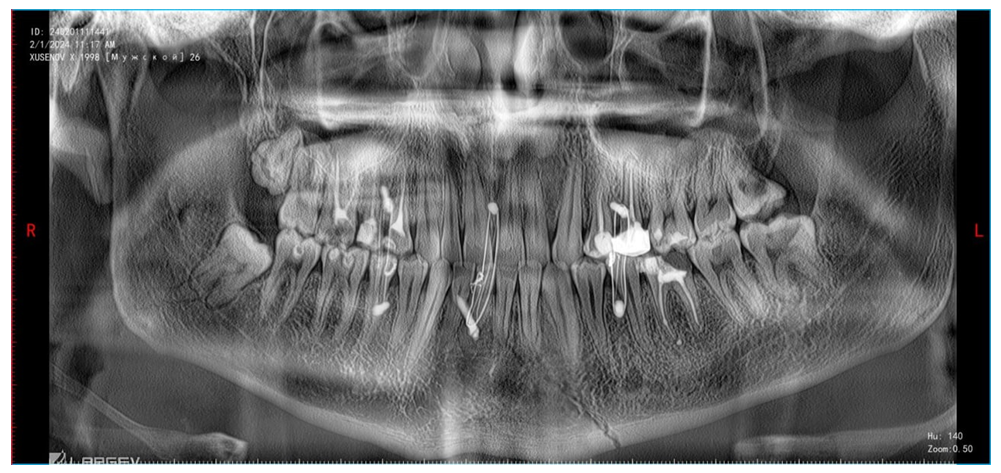
The 1st comparison group consisted of 46 patients in whom local treatment consisted of bimaxillary splinting with Tigerstedt splints, prophylactic administration of antibacterial therapy in the form of intramuscular injections of various antibiotics - cefazolin, ceftriaxone, designed for bactericidal action on Gram-positive and Gram-negative microorganisms. In cases of haematomas and pronounced edema of regional soft tissues intravenous infusions of Metrogil were used. Rinsing of the oral cavity with furacilin solution in dilution 1:5000. Vitamin therapy in the form of parenteral administration of vitamin preparations was prescribed for the purpose of general strengthening therapy and prevention of dysbacteriosis development. The 2nd comparison group consisted of 54 patients who received applications of Traumel-C ointment in the fracture area as part of the local therapeutic complex after traditional splinting of the jaws according to Tigerstedt and antiseptic treatment of the oral cavity; The 3rd - main group consisted of 57 patients in whom jaw immobilisation was carried out with cortical screws, the complex local therapy daily after the previous antiseptic treatment (traditional therapy) included applications of ointment ‘Traumel-C’ containing active components of plant and mineral origin, in the form of application to the damaged area and massaging until its complete absorption, and infrared radiation therapy (IRT). | Figure 3. Application of cortical screws with intermaxillaryimmobilisation with orthodontic wire |
 | Figure 4. Orthopantomogram of a patient with a central oblique fracture of the mandible and a fracture in the region of its angle on the right side without displacement with applied cortical screws |
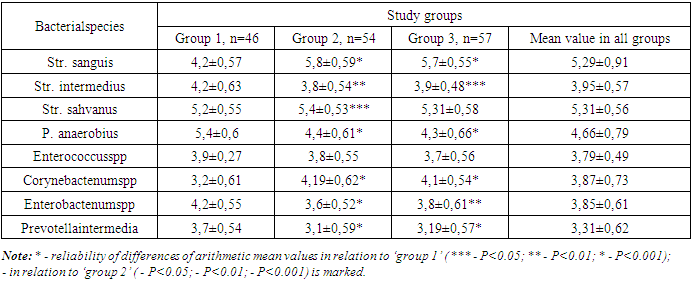
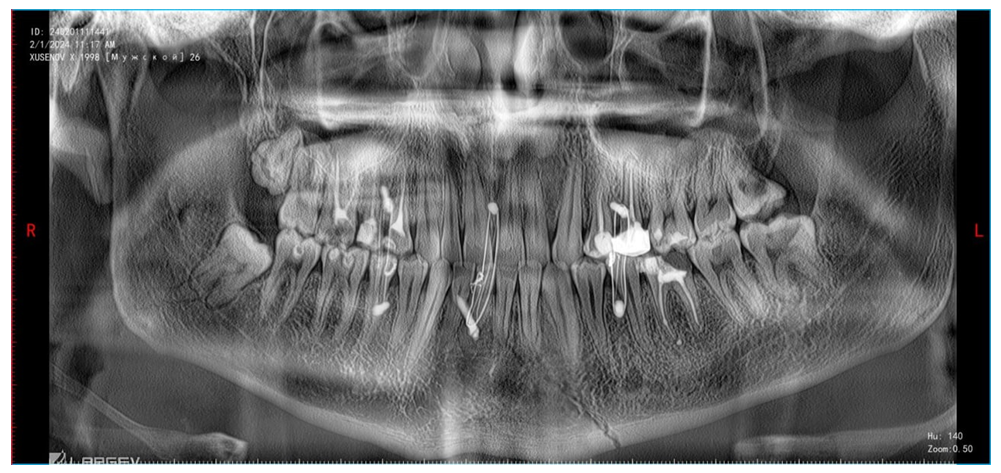
Taking into account the nature of the mandibular fracture and the course of the disease, all patients were prescribed complex treatment: in the first day after hospitalisation - therapy with broad-spectrum antibacterial drugs, and then selective administration of antibiotics taking into account the composition and sensitivity of the microflora, detoxification therapy was prescribed to prevent toxic complications and accelerate the healing process and included colloidal and crystalline solutions (glucose solution 5%, saline solutions - 0.9% sodium chloride, haemodez, reopolyglucin), desensitising therapy was recommended to reduce allergic reactions that may accompany traumatic conditions and included antihistamines such as dimedrol, suprastin and others. Vitamin therapy was used to increase general and local immunity and to prevent dysbacteriosis. Symptomatic treatment included analgesics and non-steroidal anti-inflammatory drugs to reduce pain, as well as other necessary means depending on the disease clinic.In local treatment of mandibular fractures, in cases of hematoma opening, dressing with antiseptic treatment and drainage replacement was performed. For this purpose, 3% hydrogen peroxide solution, furacilin 1:5000, chlorophyllipt 5% and other antimicrobial agents were used. Further, the patients of the 2nd and 3rd groups (after the TII procedure) were used applications of ointment of vegetable and mineral elements containing active components ‘Traumel-S’ in the form of application to the damaged area and massaging until its complete absorption.“Traumel-S” is a combined preparation. The main components of “Traumel-S” are plant extracts including arnica, calendula, chamomile, as well as other natural substances such as methylparaben, propylparaben and dimethyl sulfoxide. The action of ‘Traumel-S’ is based on its antimicrobial, anti-inflammatory, local anaesthetic, regenerating and anti-edema properties. The drug increases local blood circulation, stimulates tissue regeneration and reduces oedema.Local therapy with infrared radiation was used to accelerate healing in mandibular fractures. The procedure was carried out with the help of a special device ‘INFRARED RADIATOR S.A. MED HOLDING OOO’ (Republic of Uzbekistan), Wavelength: approximately from 800 nm to 2500 nm, with the main range around 900-1000 nm. Radiation power: in the range of 20 to 200 mW/cm2, but may depend on the model of the device used. Duration of the procedure: 5 to 10 minutes, depending on the patient's individual response. Therapy was performed in the physiotherapy department of the Bukhara Regional Multidisciplinary Medical Centre with a maximum absorption λmax of 100 J/cm² with an exposure time of 5 minutes. Infrared laser radiation was locally applied to the fracture area using a device operating at a wavelength of 808 nm with radiation energy of 2 W/cm².The distance from the end of the light guide to the skin surface in the area of localisation of the traumatic jaw injury was 0.5-2.0 cm depending on the patient's thermal discomfort. Total irradiation time was 5 minutes, in cases of double fractures polypositional irradiation was performed by smooth movement of the terminal over the entire surface of the damaged area.The procedure was performed once a day, the duration of the session depended on individual needs and was determined by the rehabilitation physician. The number of treatments varied depending on the severity of the fracture and the rate of bone consolidation. Infrared radiation affects the tissues, increasing their metabolic processes and accelerating cell regeneration. This helped to accelerate wound healing, reduce swelling and inflammation, and reduce pain.The clinical effectiveness of therapy was determined by the following characteristics: fracture healing time, reduction of pain, improvement of general condition, normalisation of body temperature, bone fragment consolidation time, improvement of microcirculation, reduction of oedema, acceleration of tissue regeneration, reduction of the risk of complications, data of blood laboratory tests (quantitative and qualitative composition of leukocytes, COE), biochemical, microbiological and immunological studies.The clinical efficacy of therapy of mandibular fractures with infrared radiation depended on many factors, including the type and characteristics of the fracture, duration and mode of treatment, as well as individual characteristics of the patient.In the study involving patients from groups I, II and III, microbiological analysis was performed using aerobic and anaerobic culturing methods. The material was collected 1, 7, 14 and 30 days after the start of treatment on an empty stomach at the same time in the morning. Samples for research were taken from the oral cavity, delivered to the laboratory of the Department of Microbiology, Virology and Immunology of BGMI within 24 hours. Various media were used for culturing including 5% blood hemin agar, AC medium and medium for the determination of Enterococcus spp. Identification was performed using API-20A test kit. For anaerobic cultures, an anaerostat with a gas mixture of N2, H2 and CO2 in certain proportions was used. The analysis revealed a sharp increase in colonisation of the oral mucosa in patients (Table 5).Table 5. Dynamics of microflora in patients of all studied groups before treatment (M±σ)
 |
| |
|
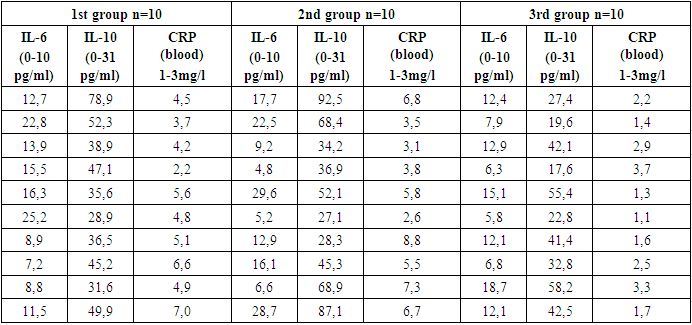
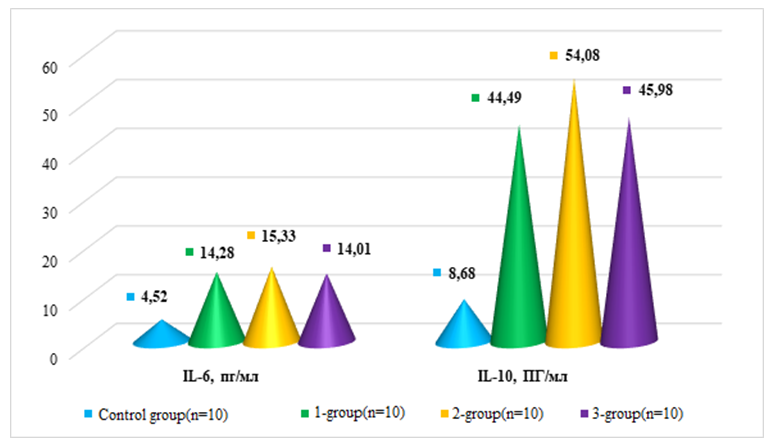
According to the data presented in Table 5, the initial quantitative estimates of Streptococcus sanguis were 5.27±0.24, P. anaerobius 4.73±0.45, Corynebactenumspp 3.87±0.18, Streptococcus intermedius 3.93±0.29, and Prevotella intermedia 3.34±0.22, indicating a significant presence of anaerobic microorganisms in the oral cavitary environment. The study of cytokine profile of oral fluid revealed an increase in key cytokines including IL-6 (14.81±1.12 pkg/ml, norm 7.2±0.37 pkg/ml) and IL-10 (34.94±2.27, norm 26.04±1.17) indicating intense inflammatory processes. The level of C - reactive protein (CRP) (5.2±0.80, norm 2.2±0.33), reflecting general inflammatory activity, was also increased. The data are presented in Table 6.Table 6. Results of cytokine content analyses in all clinical groups before treatment
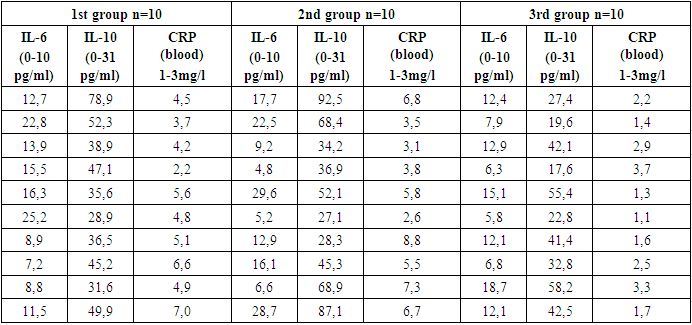 |
| |
|
All groups show a strong positive correlation between IL-6, IL-10 and CRP, which may indicate a relationship between these biochemical parameters p < 0.001.
3. Results and Their Discussion
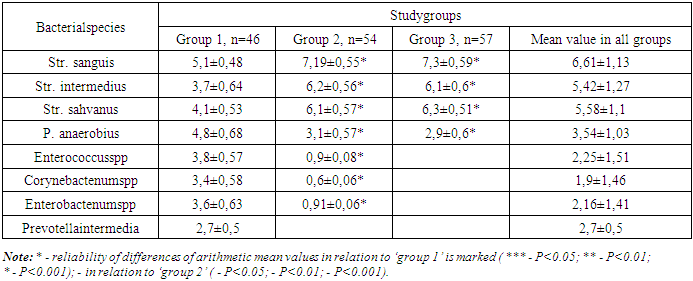
Assessment of the progress of the treatment process in mandibular fractures included monitoring of various parameters. This included the dynamics of clinical symptoms (edema, pain, functional disorders), radiological data to assess the position of bone fragments and fracture consolidation, as well as laboratory and functional recovery indicators. Infrared laser light therapy applied in the third group resulted in positive effects: reduction of oedema, reduction of pain and improvement of blood circulation. It also stimulated metabolism, improved the supply of nutrients to the tissues and accelerated fracture healing. Most local signs of injury disappeared after 4-5 sessions of physiotherapy to complement the main treatment. It is important to note that the formation of connective tissue callus in patients of the third group on the day was faster than in patients of the first group.Parameters of microbiological examination on the 30th day of therapy are shown in Table 7.Table 7. Dynamics of microflora in patients of all studied groups on day 30 of treatment (M±σ)
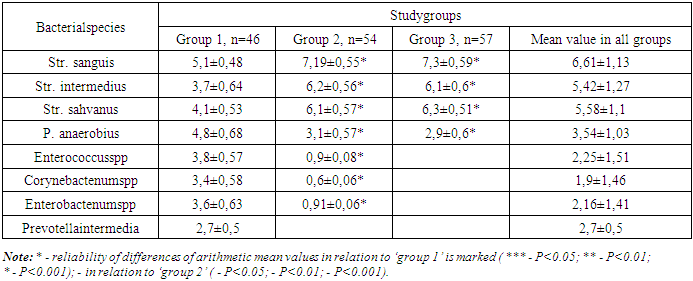 |
| |
|
From the table it can be observed that the mean value of Str. Sanguis increased in group 2 and 3 by the 30th day of treatment and decreased to 5.1±0.21 in group 1, Str. intermedius increased to 6.2±0.22 in group 2, 6.1±0.24 in group 3 by the 30th day, and in group 1 it remained at the same level as on day 14 of therapy. Enterococcus spp, Corynebactenumspp, Enterobactenumspp, Prevotella intermedia were not detected in group 2 and 3 on day 30 after placement of the constructs and initiation of antibacterial and anti-inflammatory therapy, while in group 1, where traditional therapy was used, the values were: Enterococcus spp - 3. 8±0.19, Corynebactenumspp - 3.4±0.20, Enterobactenumspp - 3.6±0.20 and Prevotella intermedia - 2.7±0.21.As for IL-6 and IL-10, these indices also came to normal in the 3rd group of patients, and in the second and first groups we got comparatively the same result. The comparative difference in results is shown in Figure 5.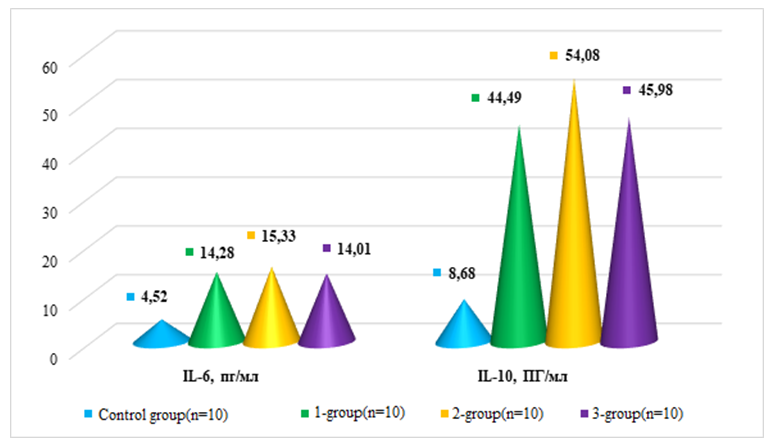 | Figure 5. Comparative indicators of IL-6 and IL-10 parameters in patients with mandible fractures, pg/ml |
Based on the data of the table, we see a significant improvement of the indicators after the therapy in all treatment groups. In the first group of subjects the average value of IL-6 was 12,54±0,82, before treatment - 14,28±1,77, IL-10 before treatment - 44,49±4,37, and after treatment decreased to 28,99±2,24, in the second group the indicators of IL-6 before treatment - 15, 33±1.88, after treatment - 11.46±1.17, and IL-10 - 54.08±6.22 before treatment and 29.1±2.29 respectively after therapy, in the third group IL-6 before treatment - 11.01±0.98 and 8.27±0.97 after, IL-10 - 35.98±2.49 and 25.04±1.47 respectively.The comparative analysis showed that the complex treatment including intermaxillary fixation with cortical screws provides faster and better healing in comparison with traditional methods. The efficacy of the applied complex treatment in the main group in terms of bone consolidation time 20.2% faster than in the comparison group has been reliably proved. This confirms the effectiveness of this approach in the treatment of mandibular fractures, especially in cases of severe injuries.
References
| [1] | Artyushkevich A.S. Errors and complications in the treatment of mandibular fractures. Modern Dentistry. 2016. № 4. С. 40-41. |
| [2] | Vorobyev A.A. et al. Modern methods of mandibular osteosynthesis (analytical review). Bulletin of VolgGMU. 2017. Vop. 2. С. 8-14. |
| [3] | Guluk A.G., Tashchyan A.E., Guluk L.N. Prevention of consolidation complications in mandibular fractures in patients with structural and metabolic changes in bone tissue. ‘Visnikstomatologii’, No. 2, 2012. С. 65 - 71. |
| [4] | Eliseeva E.V., Konev S.S., Spevak E.M. Modern methods of treatment of fractures of the lower jaw. Actual questions of clinical stomatology: collection of materials of the 52nd All-Russian scientific and practical stomatological conference, dedicated to the 110th anniversary of M. M. Slutskaya and the 70th anniversary of the foundation of the department of maxillofacial surgery in the Stavropol region. April 5-7. Stavropol, 2017. P. 176–179. |
| [5] | Levenets A.A., Gorbach N.A., Fokas N.N. Maxillofacial trauma as a social, economic and medical problem. Siberian medical review. 2013. No. 2. P. 13–18. |
| [6] | Moskalyev E. Integrated approach to rehabilitation of patients with mandible fractures and arterial hypertension. Dissertation for the degree of candidate of medical sciences. Russia. 2024. |
| [7] | Pulatova Sh.K. Analysis of a retrospective study of medical documentation of patients with mandible fractures. Integrative dentistry and maxillofacial surgery. Uzbekistan. Tashkent. Volume 3. Issue 2 (7). 2024. P. 152-157. |
| [8] | Pulatova Sh.K. Treatment tactics for victims with fractures of the lower jaw. Justification for the choice of the method of intermaxillary immobilization // Tibbiyotdayangikun. Scientific, abstract, spiritual and educational journal. Uzbekistan. Tashkent. 6 (68). 2024. P. 234-240. |
| [9] | Rakhimov Z.K., Kabanova A.A., Kabanova S.A. Microbiological evaluation of the effectiveness of infrared radiation in the complex treatment of patients with mandible fractures. Bulletin of VSMU. 2022. Vol. 21, No. 5. P. 102–108. |
| [10] | Rakhimov Z.K., Kabanova A.A., Kabanova S.A. Influence of treatment tactics for patients with mandible fractures on oral resistance indicators. Bulletin of Vitebsk State University. 2023, Issue 22, No. 3. P. 97–102. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML