Tarayan Vladimir Sergeyevich
Republican Perinatal Center, Uzbekistan
Correspondence to: Tarayan Vladimir Sergeyevich, Republican Perinatal Center, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
This article investigates cortisol levels—a key stress hormone—in pregnant women with severe preeclampsia undergoing cesarean section under spinal anesthesia (SA). The study compares the effectiveness of SA with the use of dexmedetomidine, morphine hydrochloride, and without any adjuvant. It was found that spinal anesthesia with dexmedetomidine led to a faster and more significant reduction in cortisol levels, improved postoperative pain control, and fewer side effects. The findings suggest that dexmedetomidine is an effective and safe adjuvant for spinal anesthesia in patients with severe preeclampsia.
Keywords:
Spinal anesthesia, Severe preeclampsia, Cortisol, Dexmedetomidine, Morphine hydrochloride, Cesarean section, Pain management, Adjuvants, Hormonal changes during pregnancy, Stress hormone
Cite this paper: Tarayan Vladimir Sergeyevich, Study of Cortisol Levels During Spinal Anesthesia in Pregnant Women with Severe Preeclampsia, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 940-942. doi: 10.5923/j.ajmms.20251504.19.
1. Introduction
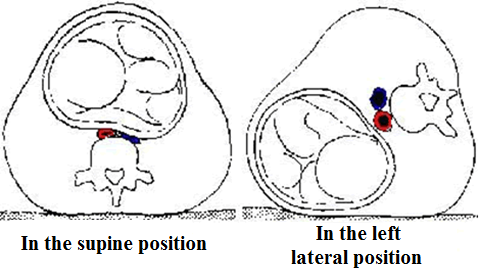
Severe preeclampsia (SP) is a manifestation of preeclampsia (PE) according to the classification of hypertensive conditions during pregnancy, refers to the main and most formidable complications, develops mainly after the 20th week of pregnancy and is characterized by high blood pressure (above 140 and/or 90 mm Hg), proteinuria and massive edema. [1]Preeclampsia occurs in 2 to 8% of all pregnancies, is one of the most important causes of maternal and perinatal morbidity and mortality, and shows no tendency to decrease. [2]In the Republic of Uzbekistan over the past 20 years, maternal mortality (MM) from preeclampsia has annually entered the top 3 obstetric causes of MM. [3] According to international studies, MM from complications of PE is 12 times more common than with other pregnancy complications if the development of TE occurs before 28 weeks of pregnancy. The main method of treating PE is delivery, in most cases the method of delivery is cesarean section. [4]In modern obstetric anesthesiology, a clear concept has been developed regarding the use of spinal anesthesia during cesarean section. This is the "gold standard" of anesthesiology in obstetrics. [7] When performing spinal anesthesia, an adjuvant is added to the local anesthetic solution to prolong postoperative analgesia. [5]In obstetric anesthesiology, opioids such as morphine hydrochloride, fentanyl, and promedol are used as adjuvants. A special group of drugs used as adjuvants are alpha-2-adrenoreceptor agonists. A new drug in this group, which is presented in Uzbekistan, is dexmedetomidine. [6] According to literature, the use of dexmedetomidine in obstetric anesthesiology has already been carried out for 8 years, but the experience of using it as an adjuvant in spinal anesthesia during cesarean section in Uzbekistan during pathological pregnancy, according to literature data, is at the stage of study.The Republican Perinatal Center has begun work on studying the effect of dexmedetomidine as an adjuvant during cesarean section in pregnant women with severe preeclampsia. The study group included women aged 20-38 years, who underwent elective (73%) and emergency (27%) surgery. Indications for surgery were severe preeclampsia as an underlying disease, as well as against the background of diabetes mellitus, kidney and liver disease, and chronic arterial hypertension (CAH).During cesarean section, laparotomy was performed using the Joel-Cohen method. All patients underwent standard examination and consultation with specialized specialists before the operation. Depending on the severity of the patient's condition, the anesthesia risks were set at 2-3 degrees according to ASA, with premedication as indicated. Use of atropine in case of a tendency to bradycardia, antihistamine drug - diphenhydramine.Spinal anesthesia to provide anesthesia assistance during cesarean section was performed using the standard technique: under local infiltration anesthesia in the lateral or sitting position, lumbar puncture was performed at the level of L3 - L4, with aG 26 atraumatic "Pencil-point" needle, a 0.5% bupivacaine solution - 0.2 mg / kg, no more than 15 mg with the addition of adjuvant dexmedetomidine 10 mcg was administered intrathecally. The adjuvant was added using a syringe for insulin administration (100 EU).Dexmedetomidine 1 ml was drawn into an insulin syringe, added to a local anesthetic 10 U, which corresponded to 10 mcg of dexmedetomidine. After the introduction of local anesthetic + adjuvant, the patient was placed on her back with a left uterine position of 15° until the fetus was extracted.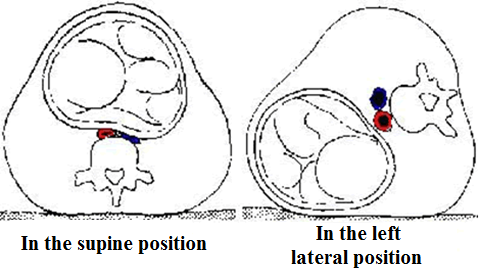 | Figure 1. The figure shows how the gravid uterus compresses the inferior vena cava (blue) and abdominal aorta (red) in the supine position, while this compression is relieved in the left lateral position |
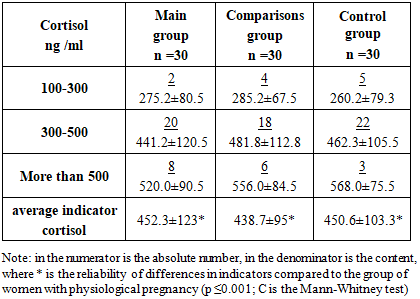
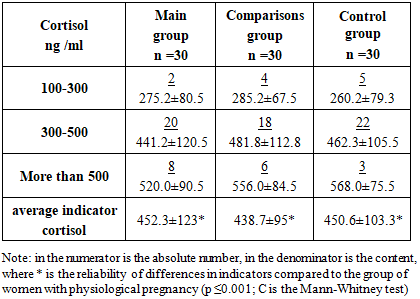
Preoperative replenishment of the BCC was not performed. Intraoperative replenishment of the BCC was performed with balanced crystalloid solutions in a volume of no more than 20 ml/kg. The duration of the operation was 35-55 minutes depending on the complexity of the access. By the end of the operation, paracetamol 1000 mg was administered intravenously as a component of multimodal anesthesia, then 1000 mg intravenously every 6 hours, no more than 4 grams per day.For laboratory confirmation of the effect of the adjuvant use on the quality of spinal anesthesia, an analysis of the study of patients for the stress hormone cortisol was conducted at several stages. The study included 90 pregnant women aged 20 to 38 years who were admitted to the Russian Orthodox Church for treatment with a complication of pregnancy in the form of hypertensive disorders such as severe preeclampsia in 2023-2024. According to the gestational age, pregnant women with severe preeclampsia in all groups were examined from 28 to 39 weeks, with a gestational age of 28-32 weeks - 18 (20%), with a gestational age of 32-35 weeks - 58 (64%) and with a gestational age of 36-39 weeks - 14 (15%) women. There were 38 primiparous women (42%), and multiparous women in the amount of 52 (58%).All pregnant women were divided into 3 groups:Group I – 30 pregnant women (33%) with severe preeclampsia who underwent cesarean section and received SMA with adjuvant dexmedetomidine at a dosage of 10 mcg.Group II – 30 pregnant women (33%) with severe preeclampsia during cesarean section; SMA with morphine hydrochloride adjuvant at a dosage of 100 mcg was used.Group III – 30 pregnant women (33%) with severe preeclampsia during cesarean section, SMA without adjuvant was used. During anesthesia, patients were not sedated, since sedation leads to inadequate patient reactions to the quality of anesthesia and pain syndrome. Patients who for some reason were sedated during surgery were excluded from the study groups.Before anesthesia, the cortisol index, according to literature data and our own data obtained during the study, exceeded the physiological pregnancy in pregnant women with preeclampsia by 2.8 times. For further study of cortisol in the blood, it was carried out at the main stages of anesthesia and at the painful stages of the cesarean section, at the 10th minute of the operation, 2 hours after the end of the operation, when the effect of the local anesthetic has completely ended.Table 1. Cortisol levels in pregnant women before anesthesia
 |
| |
|
It has been established that high levels of cortisol, corresponding to severe preeclampsia, are found in 100% of pregnant women, which indicates high tension of the sympathetic-adrenal system, confirming the correctness of the choice of indicator for assessing the use of a new pain relief technique.After the SMA with and without adjuvants using the standard technique, the following stress hormone indices were obtained. In the 1st main group with dexmedetomidine, cortisol indices began to decrease by the 15th minute after the SMA and amounted to 320.8±70.6 ng/ml, which corresponds to a 30% decrease from the index before the onset of anesthesia. After 2 hours in the postoperative period and the complete end of the local anesthetic effect, the cortisol index achieved a significant decrease to an average of 145.5±45.8 ng/ml, which is approximately 3 times lower than the level in the preoperative period. This index indicates a calm state of the sympathetic-adrenal system, complete blockade of pain receptors from the surgical site due to the blockade of alpha-2-adrenoreceptors, and a decrease in the excitability of brain structures; in this case, we received brain protection due to the central action of dexmedetomidine.In the 2nd comparison group, morphine hydrochloride was used as an adjuvant in the SMA procedure at a dosage of 100 mcg. When analyzing blood taken 10 minutes after the start of the operation, cortisol levels tended to decrease comparable to the decrease in cortisol when using dexmedetomidine, which in numerical terms was 350.8 ± 65.2 ng / ml. The difference between the use of dexmedetomidine and morphine was 15%, which indicates a better blockade of pain receptors by dexmedetomidine due to a faster onset of central action. After 2 hours in the postoperative period, the cortisol level reached 195.1 ± 45.3 ng / ml, which exceeds the comparable indicator when using dexmedetomidine by more than 20%. This indicator shows increased tension of the sympathetic-adrenal system, due to the side effects of central morphine, manifested by uncontrollable nausea, vomiting and itching of the skin.In the 3rd control group, the SMA technique was performed without the use of adjuvants. Analysis of blood plasma samples taken 10 minutes after the start of the operation showed a high level of cortisol comparable to the cortisol levels when using morphine as an adjuvant. The indicator varied at the level of 205 ± 45.2 ng / ml, which exceeds the indicator when using dexmedetomidine by more than 25%. This analysis showed a high level of tension of the sympathetic-adrenal system, and a decrease in cortisol levels only due to the effect of local anesthetic. Unlike the 1st main and 2nd comparison groups, the cortisol indicator taken after 2 hours exceeded the level of these groups by more than 40%, despite the use of multimodal analgesia as pain relief in the postoperative period.Summarizing the obtained results on the use of dexmedetomidine as an adjuvant in SMA in patients with severe preeclampsia, it can be concluded that the use of the new SMA technique in cesarean section has the best analgesia profile than when using morphine or without an adjuvant. The quality of pain relief in the postoperative period, stable indicators of postoperative nausea and vomiting also play a major role.The conducted studies on the use of dexmedetomidine as an adjuvant to a local anesthetic in spinal anesthesia to provide anesthetic assistance during cesarean section have shown an excellent analgesia profile in the intra- and postoperative period. This is significantly different from the use of opioids as adjuvants in spinal anesthesia during cesarean section. The duration of pain relief is completely comparable to the use of narcotic analgesics (morphine hydrochloride) in dosages of 100-150 mcg.
2. Conclusions
The use of dexmedetomidine as an adjuvant in cesarean section leads to a decrease in intraoperative tremors, nausea, vomiting, which improved the rehabilitation of patients after surgery. The analysis showed excellent results in postoperative pain relief, which are comparable to the use of opioids, but unlike the use of opioids, there are significantly fewer side effects that significantly reduce the quality of anesthesia after cesarean section. Side effects from the use of opioids during cesarean section force anesthesiologists to abandon their use for postoperative pain relief, switching to the use of non-steroidal drugs that do not provide such quality of pain relief, which is necessary for early rehabilitation of the woman in labor, active participation in the breastfeeding and safe motherhood program. It is also worth noting that dexmedetomidine does not belong to the group of accounting drugs from the group of narcotics and psychotropics, its use is possible in clinics of any level. All this leads to further research and development of optimal dosages and methods for the use of adjuvants in the practice of obstetric anesthesiologists.
References
| [1] | Saha D, Ghosh S, Bhattacharyya S, et al. Comparison of hemodynamic response and vasopressor requirement following spinal anaesthesia between normotensive and severe preeclamptic women undergoing caesarean section: A prospective study. J Obstet Anaesth Crit Care. 2013; 3: 23-26. DOI: 10.4103/2249-4472.114286. |
| [2] | Vosoughian M. et al. The effect of spinal and general anesthesia on cytokine serum levels following cesarean section in preeclampsia // Journal of Cellular & Molecular Anesthesia. – 2018. – Т. 3. – №. 3. – С. 89-97. |
| [3] | Bao Z, Zhou C, Wang X, Zhu Y. Intravenous dexmedetomidine during spinal anaesthesia for caesarean section: a meta-analysis of randomized trials. J Int Med Res. 2017; 45(3): 924–932. doi:10.1177/0300060517708945. |
| [4] | Bi YH, Cui XG, Zhang RQ, Song CY, Zhang YZ. Low dose of dexmedetomidine as an adjuvant to bupivacaine in cesarean surgery provides better intraoperative somato-visceral sensory block characteristics and postoperative analgesia. Oncotarget. 2017; 8(38): 63587–63595. doi:10.18632/oncotarget.18864. |
| [5] | Yu G, Jin S, Chen J, Yao W, Song X. The effects of novel -adrenoreceptor agonist dexmedetomidine on shivering in patients underwent caesarean section. Biosci Rep. 2019; 39(2): BSR20181847. doi:10.1042/BSR20181847. |
| [6] | Qi X, Chen D, Li G, et al. Comparison of intrathecal dexmedetomidine with morphine as adjuvants in cesarean sections.Biol Pharm Bull. 2016; 39(9): 1455–1460. doi:10.1248/bpb.b16-00145. |
| [7] | Xia F, Chang X, Zhang Y, Wang L, Xiao F. The effect of intrathecal dexmedetomidine on the dose requirement of hyperbaric bupivacaine in spinal anaesthesia for caesarean section: a prospective, doubleblinded, randomized study. BMC Anesthesiol. 2018; 18(1): 74. doi:10.1186/s12871-018-0540-6. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML