Toshev Furkat Nishonovich1, Irismetov Murodjon Ergashevich2
1Head of Department of Traumatology and Orthopedics, Bukhara Regional Multi-Network Medical Center, Bukhara State Medical Institute, Bukhara, Uzbekistan
2Director of the Republican Center for Specialized Traumatology and Orthopedic Scientific and Practical Medicine, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Knee osteoarthritis is a bone and joint disease characterized by degenerative-dystrophic changes and inflammatory processes, and is one of the leading causes of disability. This article analyzes the possibilities of conservative treatment of knee osteoarthritis using autologous platelet mass (ATM). In a study involving 114 patients, patients treated with ATM showed a decrease in pain syndrome, improved joint function, and a decrease in morphological changes. The effectiveness of ATM was assessed using MRI and functional tests. The results of the study confirm the effectiveness of autologous platelet mass in the treatment of knee osteoarthritis.
Keywords:
Osteoarthrosis of the knee joint, Autoplatelet mass, Plasma therapy, Joint tissue, Inflammation, Regeneration, Clinical analysis
Cite this paper: Toshev Furkat Nishonovich, Irismetov Murodjon Ergashevich, Conservative Treatment of Knee Joint Osteoarthritis Using Autothrombotic Mass and Its Clinical Analysis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 934-939. doi: 10.5923/j.ajmms.20251504.18.
1. Introduction
Inflammation is a universal pathological process that underlies the clinical manifestations of osteoarthritis. The important role of inflammation in the pathogenesis of osteoarthritis of the knee joint is confirmed by many factors: the presence of hyperplasia and mononuclear cell infiltration in the synovial membrane of the joint, which is no different from rheumatoid arthritis [1], increased expression of oncoproteins and transcription factors NF-kB, control of the synthesis of "pro-inflammatory" mediators, the relationship between the steady-state concentration of CRP and OA, the effectiveness of intra-articular administration of glucocorticoids and other "anti-arthrosis" drugs (for example, diacerein), the superiority of nonsteroidal anti-inflammatory drugs (diclofenac) over paracetamol [2].Knee osteoarthritis (OA) is a chronic degenerative-dystrophic disease characterized by the degradation of joint tissues, a decrease in the hyaluronan-chondroitin complex, and increased inflammatory processes [3]. According to the World Health Organization, osteoarthritis is an age-related disease and one of the main causes of disability among the population (WHO, 2021).The use of autologous platelet concentrate (APC) as a conservative treatment for knee OA has received particular attention in recent years. APC, or platelet-rich plasma (PRP), has the potential to regenerate tissues, reduce inflammation, and stimulate angiogenesis by utilizing the body's own biological resources [4].Several studies have shown that ATM increases the metabolic activity of chondrocytes in knee osteoarthritis, promotes hyaline cartilage regeneration, and reduces pain [5]. ATM has also been reported to reduce inflammation and improve synovial fluid quality due to the presence of bioactive factors (PDGF, TGF- β, VEGF) [6].Therefore, it is suggested that the use of ATM in the treatment of osteoarthritis may be more effective than conventional therapies, and further research is needed in this regard [7].Research Objective: This study aimed to evaluate the effectiveness of conservative treatment of knee osteoarthritis using autologous platelet mass (ATM). The study compared the results of using ATM with traditional treatment methods and analyzed clinical and functional changes.
2. Research Materials and Methods
114 patients were examined and divided into two groups. The main group (n=70) received ATM therapy in addition to conservative therapy. The control group (n=44) was limited to standard conservative treatment methods. Basically, the patients under control complained of pain in the joint, pain radiating to the knee joint, shin and shin area, and limited mobility. The pain syndrome was always associated with physical activity and usually appeared within a few seconds or minutes after the start of movement. The intensity of the pain syndrome can be very diverse, from episodic pain to constant pain syndrome during the entire period of load on the joint. In some cases, the pain syndrome can persist for several minutes or hours after the end of the stress. Most often, patients complain when starting to move after a long rest or sleep. In particular, this complaint is also characteristic of patients with rheumatoid arthritis or gout. Morning joint stiffness lasts up to 30 minutes. The addition of an inflammatory process in the joint prolongs this time. One of the important aspects of making a diagnosis and subsequently choosing the right treatment tactics is the identification and comprehensive analysis of all possible risk factors.
3. Results of the Study
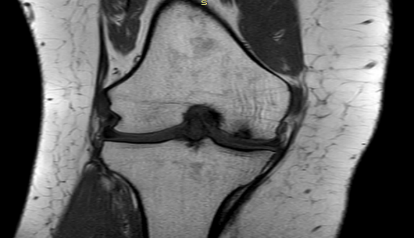
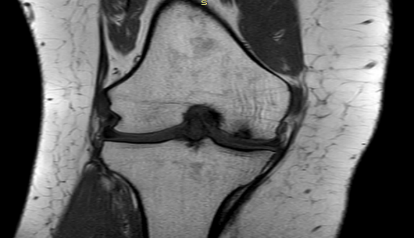
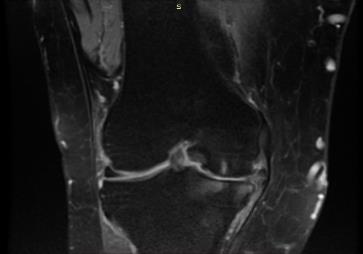
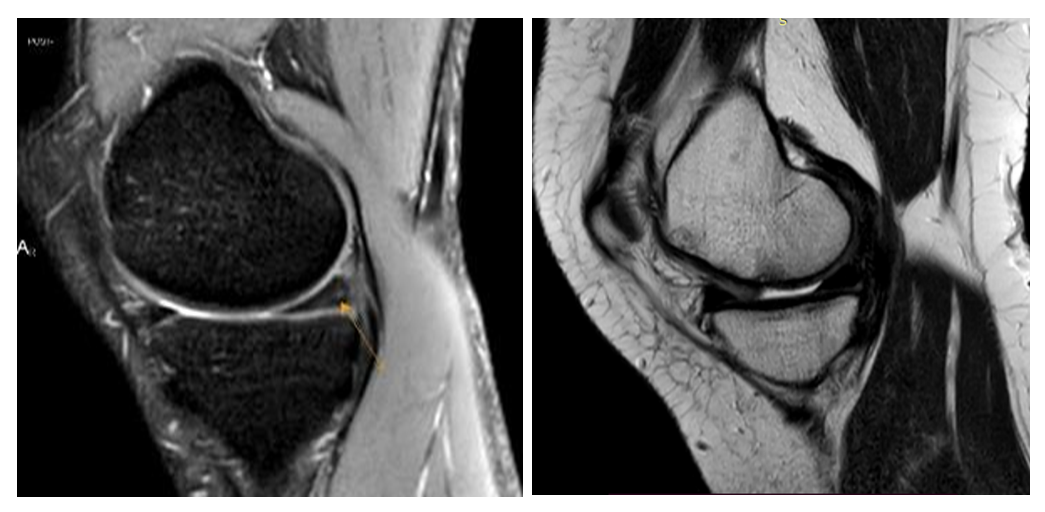
Among the patients with osteoarthritis of the knee joint (OAK) under observation, 14 (12%) had a mild degree of the disease. Of these patients, 4 (3.5%) patients aged 25 to 45 years, 6 (5%) patients aged 46 to 60 years, and 4 (3.5%) patients aged 61 to 75 years had clinical stage I osteoarthritis of the knee joint.The height of the knee joint is unevenly reduced on average, more in the medial parts of the joint, and there are degenerative changes in its structure.Of the patients under observation, 14 (12%) had clinical grade I knee osteoarthritis before treatment, and MRI revealed a moderate uneven decrease in the height of the knee joint in the medial parts of the joint, indicating the presence of degenerative changes (Fig. 1).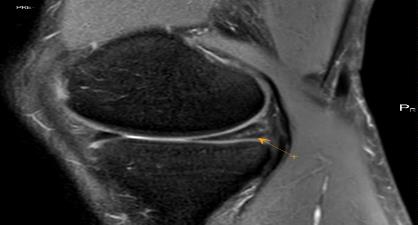 | Figure 1. Patient R.R. 42 years old. MRT-examination of the left knee joint (before treatment) |
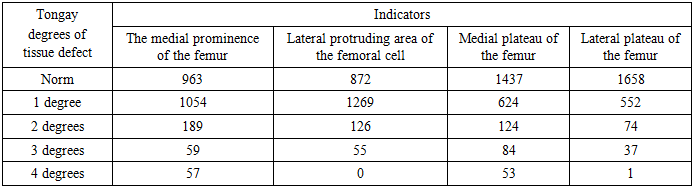
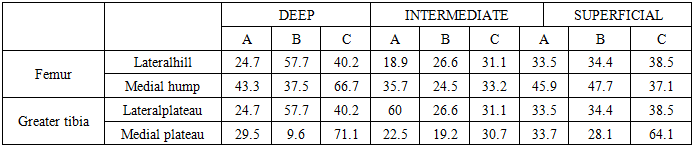
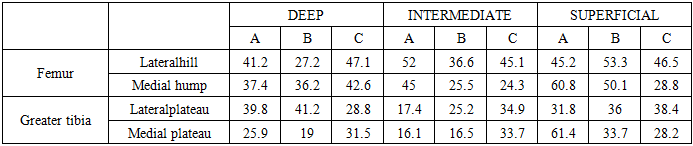
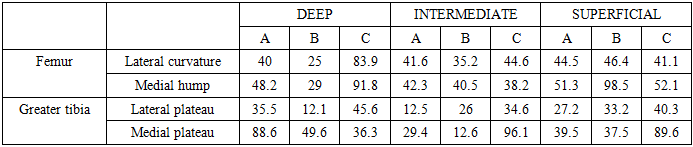
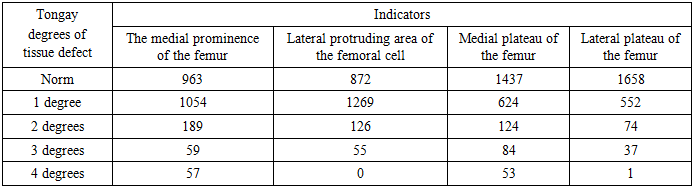
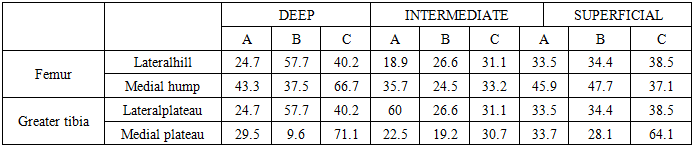
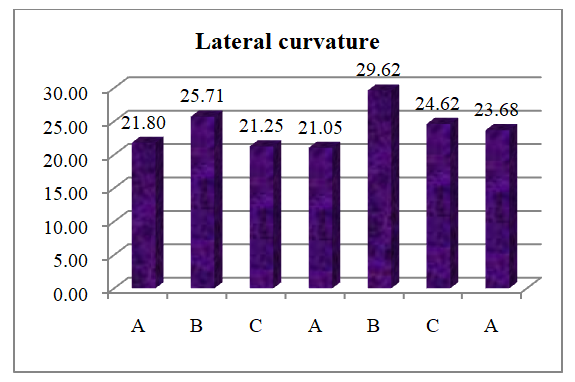
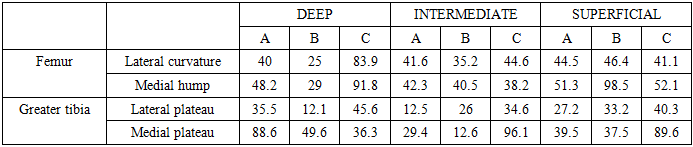
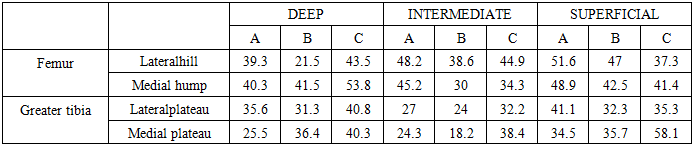
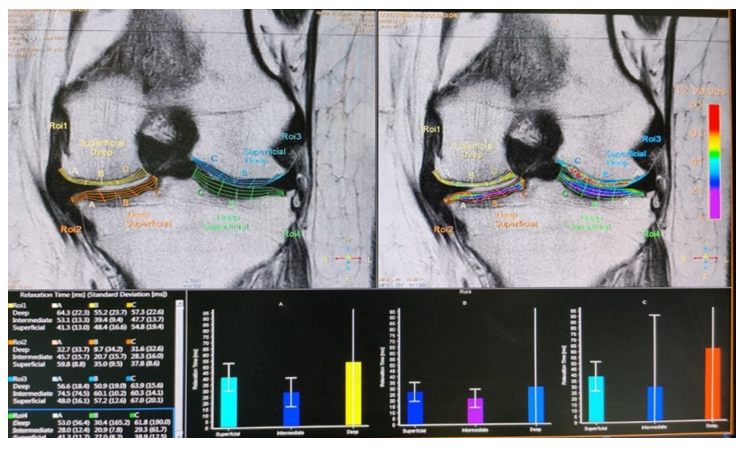
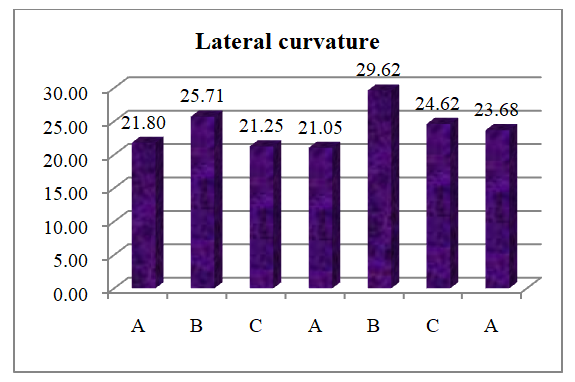
In patients with knee osteoarthritis, the knee cartilage tissues were studied using T2 cal and processing with a special MR Cartilage Assessment program. 36 parameters were obtained from each knee joint: knee zones A, B, C, and each of them was divided into 3 layers - these are superficial, middle and deep layers and lateral and medial tubercles of the femur and plateaus of the greater tibia, a total of 9288 parameters were studied (Table 1).Table 1. Studying the cartilage tissues of patients' knee joints using T2 cal and processing with a special program MR Cartilage Assessment
 |
| |
|
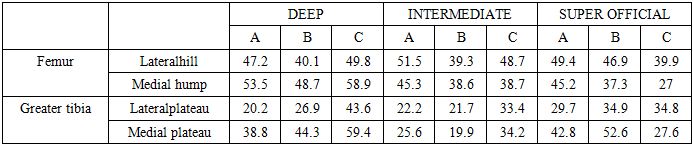
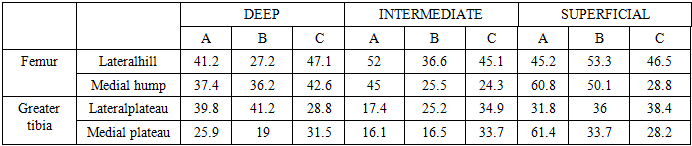
1 allows us to draw the following conclusions: Grade 1 articular cartilage degeneration is more widespread, with increased fluid accumulation, and more pronounced changes in the articular cartilage of the femur compared with the greater femur.Thus, T2 calwith the help of MPTDiagnostics is a very promising method for early detection and monitoring of structural changes characteristic of bone tissues.In order to evaluate the effectiveness of MRI diagnostics in the diagnosis of articular cartilage lesions in relation to T2 time, as well as in the diagnosis of systemic changes in the cartilage, normal and increased T2 values were compared. An increase in the T2 time of the cartilage tissues indicated an expansion of the intercellular space due to edema or chondrocyte death. In 14 (12%) patients with grade I osteoarthritis of the knee jointThe knee joint cartilage was assessed. 36 measurements were taken from each knee joint (the medial femoral condyles are divided into A, B, and C layers, each of which is divided into 3 layers - superficial, middle, and deep layers, and the lateral femoral condyles are also divided into the medial and lateral plateaus of the tibia), a total of 9288 parameters were studied to determine the degree of degeneration of the cartilage.In 14 (12%) patients with grade I knee osteoarthritis, quantitative evaluation of the knee joint cartilage revealed a predominance of grade 1 degeneration (increased hydration) in MRI data based on the results of a color map of the knee joint cartilage (Table 2).Table 2. MRI data based on the results of color mapping of knee joint tissue (before treatment)
 |
| |
|
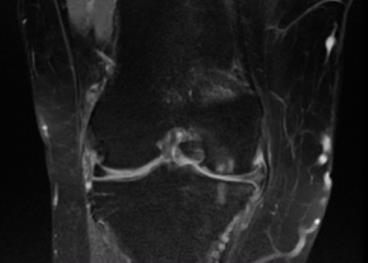
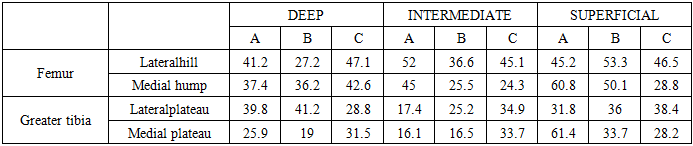
According to the results of the study, 6 months after treatment (after the use of autoplatelet mass), when MRI was repeated dynamically using the sT2Cal TSE-coronal coronal mode, a decrease in degenerative changes in the tissues of the knee joint was detected, based on the recording of the mapping time (T2) indicator in milliseconds (ms). 14 (12%) of the patients under control had clinical grade I osteoarthritis of the knee joint after treatment, and the height of the knee joint was preserved on MRI. Degenerative changesit was found that it decreased (Fig. 2).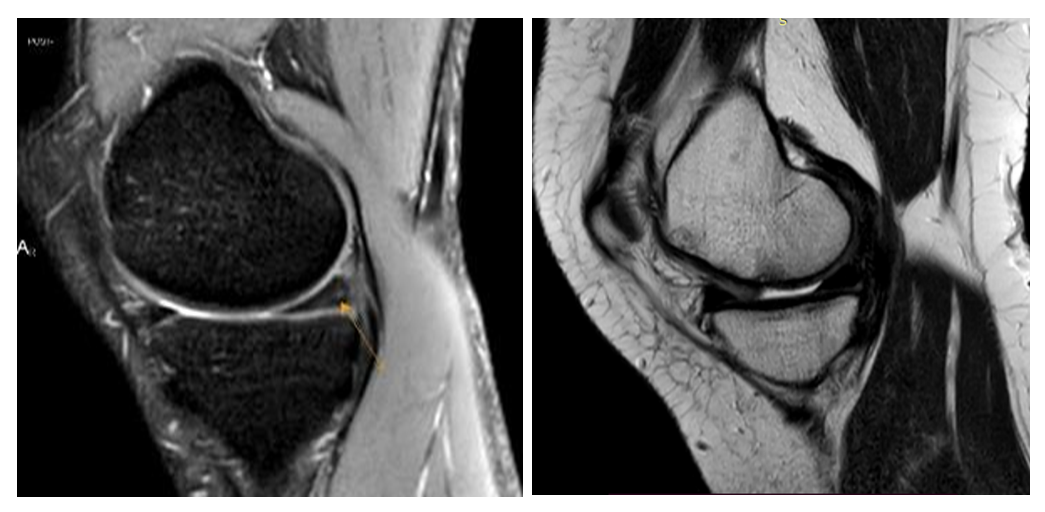 | Figure 2. Patient R.R. 42 years old. MRT examination of the left knee joint (after treatment). The height of the knee joint is preserved |
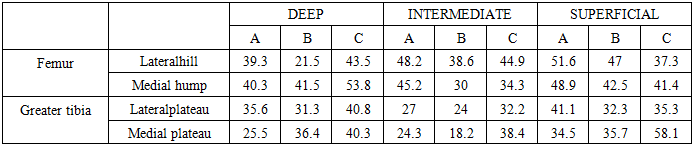
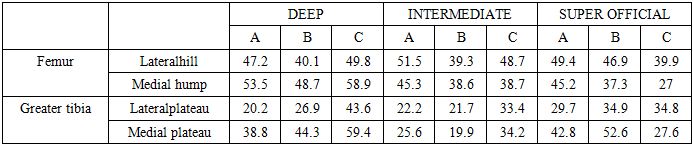
Based on the results of the color map of the knee joint tissue, the reduction of the degenerative process of the 1st degree was detected in the MRI data (Table 3).Table 3. MRI data based on the results of color mapping of knee joint tissue (after treatment)
 |
| |
|
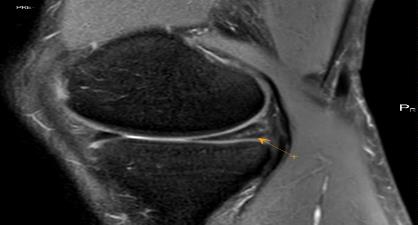
In patients who received standard treatment, MRI results did not show any significant changes, which indicates that there were no effective changes in their condition. During the MRI, degenerative changes in the tissues of the knee joint remained. The lack of improvement in this process indicates the complexity of the patients' condition and the ineffectiveness of the standard treatment methods given to them. This situation, which indicates the ineffectiveness of standard treatment methods, reinforces the idea of the need for the use of new, effective treatment methods in clinical practice. These results encourage doctors and researchers to expand the use of new, successful treatment methods, such as the use of autologous platelet mass.Knee Injury And Osteoarthritis Outcome Score (Knee Injury And Osteoarthritis Outcome Score) in Grade 1 Osteoarthritis of the Knee.The KOOS scale consists of 5 sections, with a total of 42 questions, allowing to assess the anatomical and functional characteristics of the condition of the knee joints. According to the KOOS scale questionnaire, the average total score in patients with grade 1 osteoarthritis of the knee joint before treatment was 64.1 to 73.5, which is considered good.Of the patients with osteoarthritis of the knee joint (OAK) under observation, 61 (53.0%) had a moderate degree of disease. Of these patients, 24 (21%) aged 25 to 45 years, 29 (25%) aged 46 to 60 years, and 8 (7%) aged 61 to 75 years had clinical stage II osteoarthritis of the knee joint.Of the patients under observation, 61 (53.0%) had clinical grade II knee osteoarthritis after treatment, and the knee joint height was preserved on MRI. Degenerative changeswas found to be present (Fig. 3).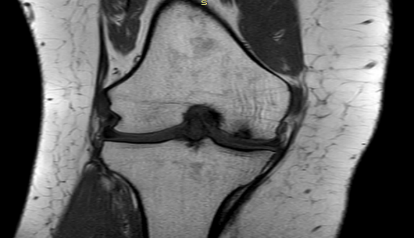 | Figure 3. Patient Sh.A., 51 years old. MRI scan of the left knee joint (before treatment). The height of the knee joint is significantly reduced. Degenerative changes are visible. Arthrosis of the knee joint, grade II |
Table 4. MRI data based on the results of color mapping of knee joint tissue (before treatment)
 |
| |
|
MRI data based on the results of color mapping of the knee joint tissues in 14 (12%) patients with grade I knee osteoarthritis revealed a decrease in the degenerative process to grade 1 (Table 5).Table 5. MRI data (after treatment) based on the results of color mapping of knee joint tissue
 |
| |
|
According to the results of the studies, 6 months after treatment (after the use of Autoplatelet Mass), a decrease in degenerative changes in the tissues of the knee joint was detected when MRI was repeated dynamically using the sT2Cal TSE-coronal coronal mode, based on recording the mapping time (T2) indicator in milliseconds (ms).After treatment (after the use of autoplatelet mass) according to the KOOS scale questionnaire, good results were achieved in grade 1 osteoarthritis of the knee joint, with average total scores ranging from 74.5 to 83.5.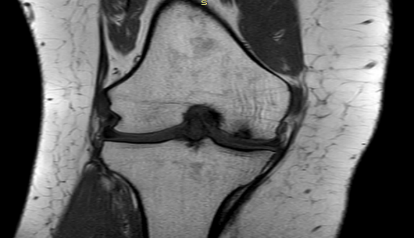 | Figure 4. Patient Sh.A., 51 years old. MRI scan of the left knee joint (before treatment). The height of the knee joint is significantly reduced. Degenerative changes are visible. Arthrosis of the knee joint, grade II |
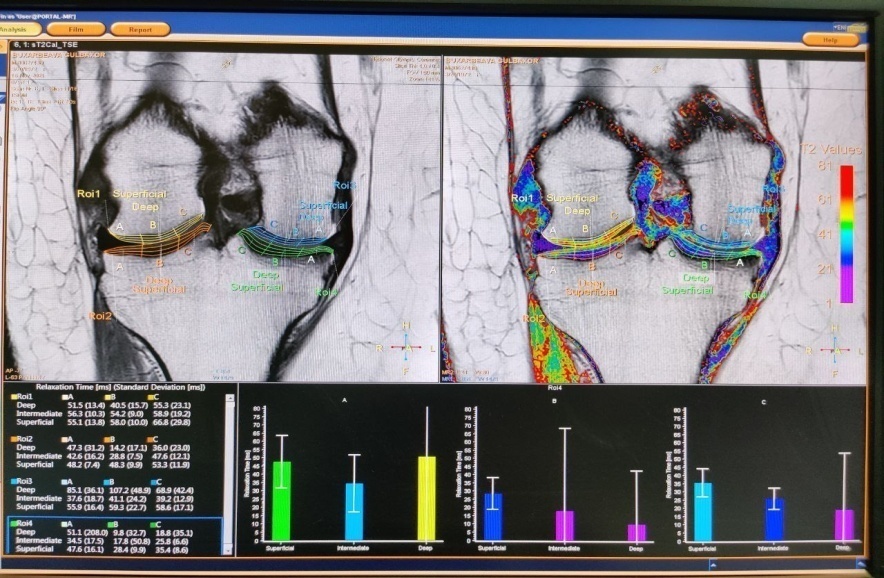
As a result of the use of autoplatelet mass, the remaining patients showed high treatment efficiency, a clear reduction of degenerative changes in the knee joint tissues and an improvement of the clinical condition, which confirms the effectiveness of this method.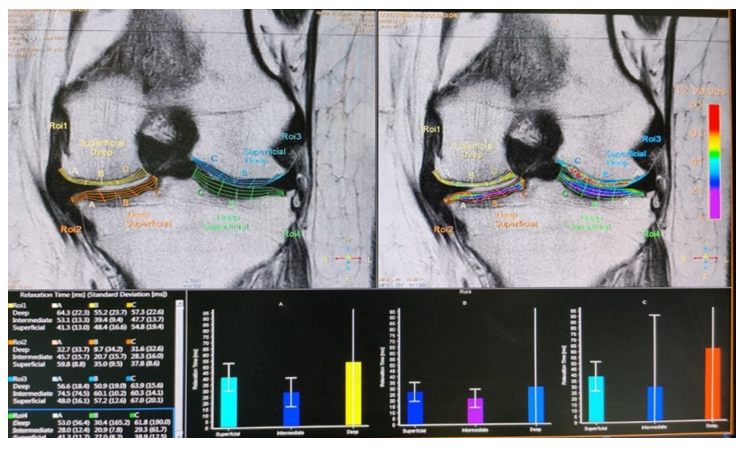 | Figure 5. Patient R.R. 50 years old. Left knee joint MRT-examination knee joint tissue color mapping software. (before treatment) |
According to the results of the conducted studies, the presence of degenerative changes in the articular cartilage tissues was detected in the MRI data based on the results of the color map of the knee joint cartilage tissues, based on the recording of the mapping time (T2) indicator in milliseconds (ms) when performing MRI using the sT2Cal TSE-coronal coronal mode before treatment.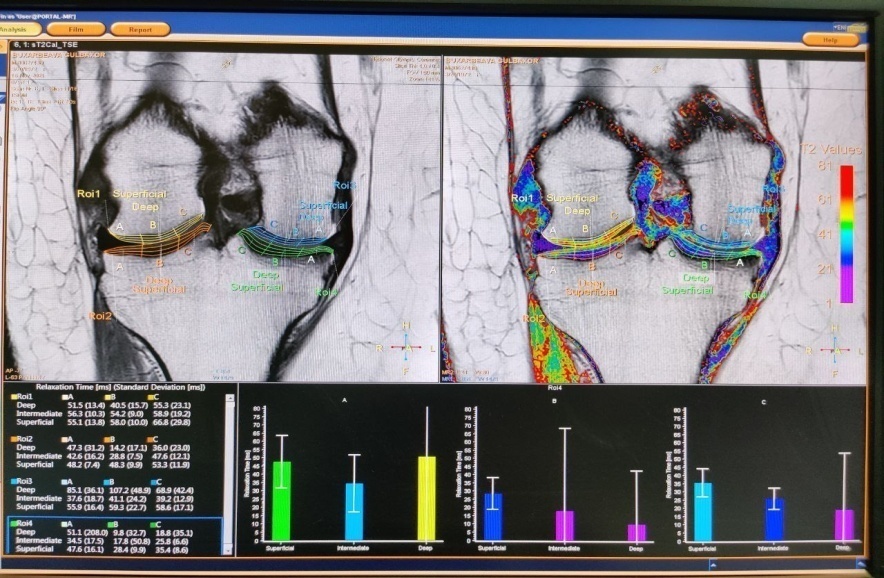 | Figure 6. Patient R.R. 50 years old. Left knee joint MRT-examination knee joint tissue color mapping software. (after treatment) |
Of the patients with osteoarthritis of the knee joint (OAK) under observation, 39 (35.0%) had a moderate degree of disease. Of these patients, 17 (15%) aged 25 to 45 years, 16 (14%) aged 46 to 60 years, and 6 (5.2%) aged 61 to 75 years had clinical stage III osteoarthritis of the knee joint.Of the patients under observation, 39 (35%) had clinical grade III knee osteoarthritis before treatment, and MRI revealed a moderate uneven decrease in the height of the knee cap in the medial parts of the joint, indicating the presence of degenerative changes (Fig. 7).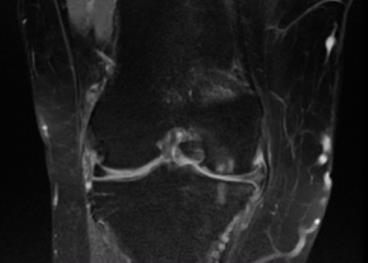 | Figure 7. Patient K.U., 52 years old. MRI scan of the right knee joint (before treatment). The height of the knee joint is significantly reduced. Degenerative changes are clearly visible. Knee joint arthrosis, grade III |
 | Figure 8 |
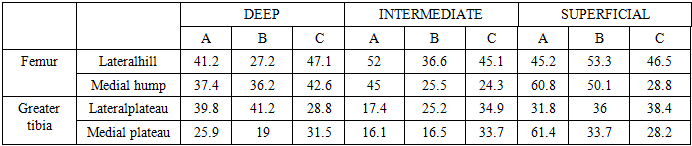
MRI data based on the results of a color map of the knee joint cartilage tissues in patients revealed a predominance of grade III degeneration (increased hydration) (Table 6).Table 6. MRI data based on the results of color mapping of knee joint tissue (before treatment)
 |
| |
|
According to the results of the studies, the presence of pronounced degenerative changes in the articular cartilage tissues was detected in the MRI data based on the results of the color map of the knee joint cartilage tissues, based on the recording of the mapping time (T2) indicator in milliseconds (ms) during MRI performed using the sT2Cal TSE-coronal coronal mode before treatment.Of the patients under observation, 39 (35%) had clinical grade III knee osteoarthritis after treatment, and the knee joint height was preserved on MRI. Degenerative changesit was determined that it decreased (Fig. 9).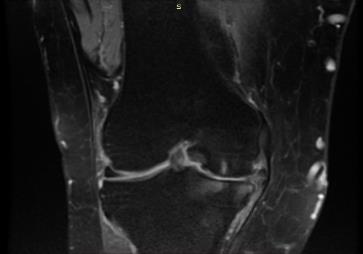 | Figure 9. Patient K.U., 52 years old. MRI scan of the right knee joint (after treatment). The height of the knee joint is significantly reduced. Degenerative changes have decreased. Knee joint arthrosis, grade III |
In 39 (35.0%) patients with grade III knee osteoarthritis, MRI data based on the results of color mapping of the knee joint cartilage revealed a decrease in grade III degeneration (decreased hydration) (Table 7).Table 7. MRI data based on the results of color mapping of knee joint tissue (after treatment)
 |
| |
|
According to the results of the studies, after treatment, a decrease in degenerative changes in the articular cartilage was detected in the MRI data based on the results of the color map of the knee cartilage tissues, based on the recording of the mapping time (T2) indicator in milliseconds (ms) when performing MRI using the sT2Cal TSE-coronal coronal mode.
4. Conclusions
The results of the study showed that the use of autologous platelet mass (ATM) is highly effective in the treatment of osteoarthritis of the knee joint. Patients who received ATM experienced a decrease in pain, improved joint function, and a decrease in morphological changes. MRI analyses showed an improvement in the condition of the articular cartilage in the ATM group. The study suggests that ATM therapy can be used as an effective and innovative method for the treatment of osteoarthritis.
References
| [1] | World Health Organization (WHO). (2021). Musculoskeletal health: Osteoarthritis. Retrieved from www.who.int. |
| [2] | Sánchez M., Fiz N., Azofra J., Usabiaga J., AdurizRecalde E., García Gutierrez A., & Anitua E. (2017). A randomized clinical trial evaluating plasma rich in growth factors (PRGF) versus hyaluronic acid in the short-term treatment of knee osteoarthritis. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 33(7), 1179-1187. |
| [3] | Filardo G., Di Matteo B., Cohn E., Merli G., Marcacci M. (2019). Platelet-rich plasma in osteoarthritis: where do we stand? Current Reviews in Musculoskeletal Medicine, 12(1), 5-13. |
| [4] | Anitua E., Sánchez M., Orive G., Andía I. (2020). The role of platelet-rich plasma in tissue regeneration: review of the literature and future directions. Regenerative Medicine, 15(6), 1965-1985. |
| [5] | Vaquerizo V., Plasencia MA, Arribas I., Seijas R., Padilla S., Orive G., Anitua E. (2018). Comparison of intra-articular injections of plasma rich in growth factors (PRGF- Endoret) versus Durolane hyaluronic acid in the treatment of knee osteoarthritis: a randomized controlled trial. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 34(3), 773-784. |
| [6] | Nishonovich TF, Ergashovich IM Analytical Indicators Of Complex Treatment Methods For Arthrosis Of The Knee Joint // Journal of Advanced Zoology. - 2024. - T. 45. – no. 1. |
| [7] | Turaeva FA Methods of application of autothrombotic mass in periodontic diseases // Academicia: An International Multidisciplinary Research Journal. - Kurukshetra, India. - 2020. - T. 10. – no. 5. - S. 1814-1817. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML