-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 926-929
doi:10.5923/j.ajmms.20251504.16
Received: Mar. 9, 2025; Accepted: Mar. 28, 2025; Published: Apr. 6, 2025

Characteristics of Corneal Topography in the Risk of Primary Angle Closure Glaucoma
Kasimova Munira Sadikjanovna1, Kalankhodjaev Botir Abdunabievich2, Tursunova Feruza Alisherqizi3, Bilalova Saida Sabirovna4
1DSc, Professor, Center for Professional Qualification Development of Medical Workers, Tashkent, Uzbekistan
2PhD, CRYSTAL Clinic, Tashkent, Uzbekistan
3Basic Doctoral Student, Center for Professional Qualification Development of Medical Workers, Tashkent, Uzbekistan
4Ophthalmologist, CRYSTAL Clinic, Tashkent, Uzbekistan
Correspondence to: Kasimova Munira Sadikjanovna, DSc, Professor, Center for Professional Qualification Development of Medical Workers, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Glaucoma is one of the major problem of ophthalmology, leading to irreversible vision loss and affecting 15-25% of the population over 40 years old. Objective: To assess the topographic features of the cornea in the progression of primary angle-closure glaucoma. Methods: The study involved 45 patients (54 eyes), divided into three groups. The first group consisted of 16 patients (8 eyes) diagnosed with primary angle-closure glaucoma (PACG) I A. The second group consisted of 13 patients (26 eyes) diagnosed with primary closure of the anterior chamber angle. The third group consisted of 12 patients (23 eyes) with mild hypermetropia. Results: The study revealed a direct correlation between keratotopographic indicators and the width of the anterior chamber angle, as well as the risk of anterior chamber angle closure with an increase in intraocular pressure (IOP). Higher peripheral corneal thicknesses corresponded in eyes with anterior chamber angle closure and increased IOP. A direct correlation was also found: patients with a wider anterior chamber angle had lower peripheral corneal thickness. Conclusions: The results show a higher risk of anterior chamber angle closure with increased IOP in patients with thicker peripheral corneal profiles. Patients with lower keratotopographic values in the peripheral zones of the cornea have a lower tendency toward angle closure and increased IOP.
Keywords: Glaucoma, Keratotopography, Cornea, Anterior chamber, Lens
Cite this paper: Kasimova Munira Sadikjanovna, Kalankhodjaev Botir Abdunabievich, Tursunova Feruza Alisherqizi, Bilalova Saida Sabirovna, Characteristics of Corneal Topography in the Risk of Primary Angle Closure Glaucoma, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 926-929. doi: 10.5923/j.ajmms.20251504.16.
1. Introduction
- Glaucoma is a chronic and progressive optic neuropathy that resultsin a characteristic optic nerve headappearance and retinal nerve fiber layer, which in turn leads to the progressive death of retinal ganglion cells and the development of typical visual field defects.The World Health Organization (WHO) has established that 105 million people worldwide suffer from glaucoma, and 5 million people are completely blind as a result of this disease [1,2]. The prevalence of glaucoma is 1.5-2% among individuals over 40 years old, and even higher among those over 60. Glaucoma is the second most frequent cause of irreversible blindness after diabetic retinopathy [4,5].In the multicenter international randomized controlled study EAGLE, initial treatment with transparent lens removal proved to be more effective compared to laser peripheral iridotomy in combination with local medication for participants with primary angle closure and primary angle-closure glaucoma. Despite the difficulties in quantitatively assessing changes reported by patients, improvements in overall health, vision, and glaucoma-related disability were recorded, even in the absence of cataracts in patients [3].Many authors have studied the relationship between the lens and the development of primary angle-closure glaucoma, but the significance of corneal parameters in the risk of developing angle-closure glaucoma has been insufficiently explored. Further research may confirm the potential of using corneal parameters as a biological marker for monitoring patients with primary angle-closure glaucoma.Study Objective: To evaluate the topographic features of the cornea during the progression of primary angle-closure glaucoma.
2. Material and Methods
- The study included 45 patients (54 eyes), divided into three groups. The first group consisted of 16 patients (8 eyes) diagnosed with primary angle-closure glaucoma (PACG) I A. The second group consisted of 13 patients (26 eyes) diagnosed with primary closure of the anterior chamber angle. The third group consisted of 12 patients (23 eyes) with mild hypermetropia. The patients’ ages ranged from 40 to 55 years (mean age 48.1±3.6 years).A full set of standard and specific diagnostic tests was performed at the CRYSTAL clinic. Patients underwent the following ophthalmological examinations: visual acuity measurement, tonometry, biomicroscopy, keratotopography (Oculus Pentacam AXL, Germany), non-contact endothelial microscopy (EM-4000 microscope, TOMEY, Japan), gonioscopy, fundoscopy with Goldman lens (Ocular Instruments, USA), threshold computerized perimetry (with PSD and MD indices evaluation) (TOMEY), optical coherence tomography (OCT) using the REVO NX OPTOPOL (Poland).
3. Results and Discussion
- With the development of modern ophthalmology, new etiopathogenetic features of the anterior segment of the eye are emerging in the development of PACG. The morphological structure of the cornea also plays a significant role in the development of PACG. According to the results of the examinations, all subgroups had similarly short eye dimensions, with an average of 22.3±0.2 mm, anterior chamber depth of 2.40±0.1 mm, and lens thickness of 4.8±0.12 mm. Central corneal thickness measurements varied within the average range in all study groups, with a mean of 548.5±1 µm. The keratotopography data differed among the three groups. In Group I, the keratotopography values were 715±6.9 µm (7.3% higher compared to Group III), in Group II, it was 685±5.3 µm (3.3% higher compared to Group III), and in Group III, it was 663±5.1 µm. The keratometric values of patients in Group I were lower (by 6.1%), indicating a flatter corneal profile. In contrast, eyes with a steeper corneal profile and higher keratometry values were noted in Groups II and III.According to gonioscopy data, the average angle width by Schaffer in patients from the first group was 8.2°, in the second group it was 14.4°, and in the third group, the angle width was the highest, at 32.8°.The conducted study revealed a direct relationship between keratotopographic indicators and the width of the anterior chamber angle: lower keratotopography values at the periphery and increased thickness of the peripheral corneal zone corresponded to the pattern observed in the eyes of patients with anterior chamber angle closure and uncompensated intraocular pressure (IOP). A direct correlation was established for patients with a wider anterior chamber angle, where peripheral corneal keratotopography values were lower. An indirect correlation was also found between increased thickness of the peripheral corneal zone and a narrower anterior chamber angle (Fig. 1).
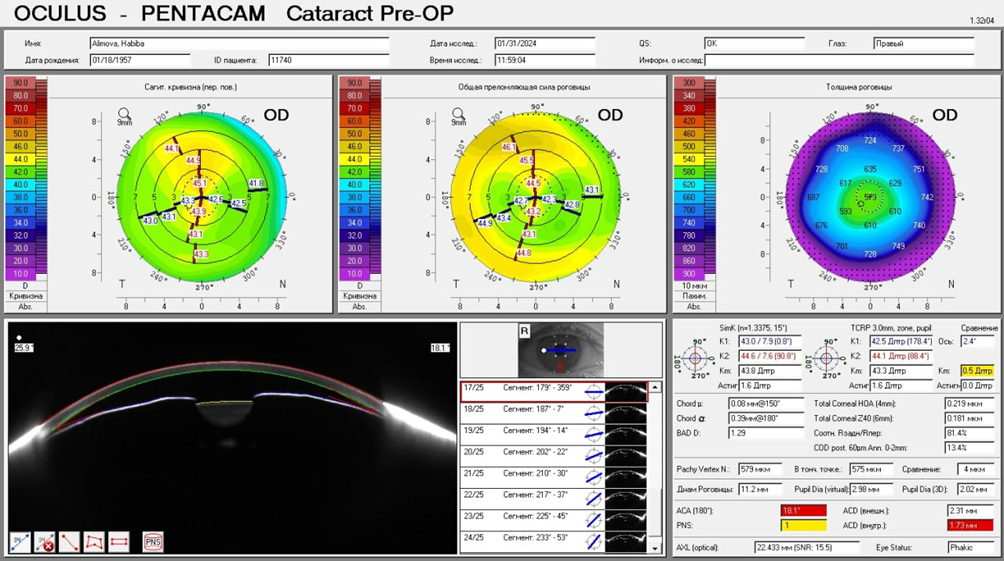 | Figure 1. Example of keratotopography from Research Group I |
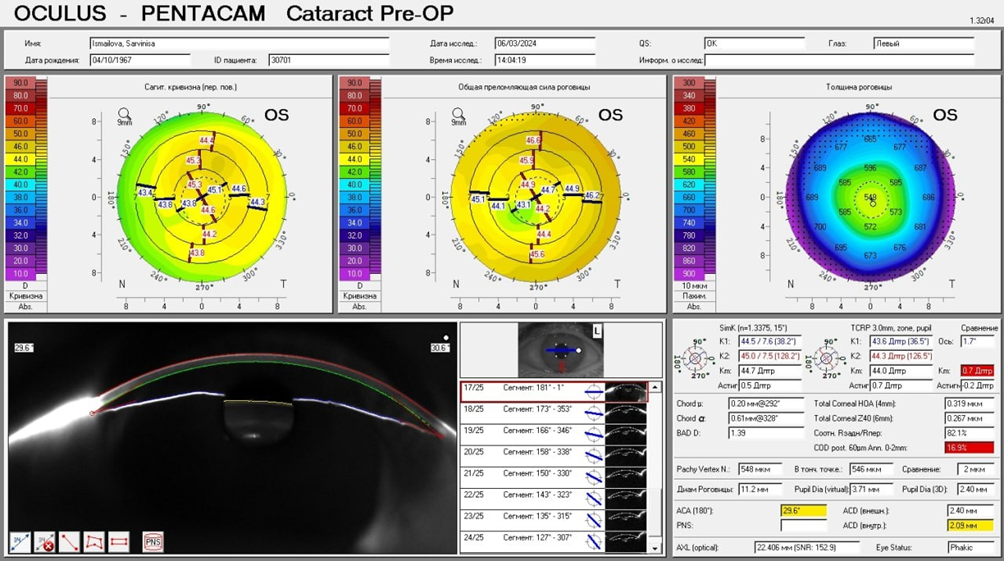 | Figure 2. Example of keratotopography from Research Group II |
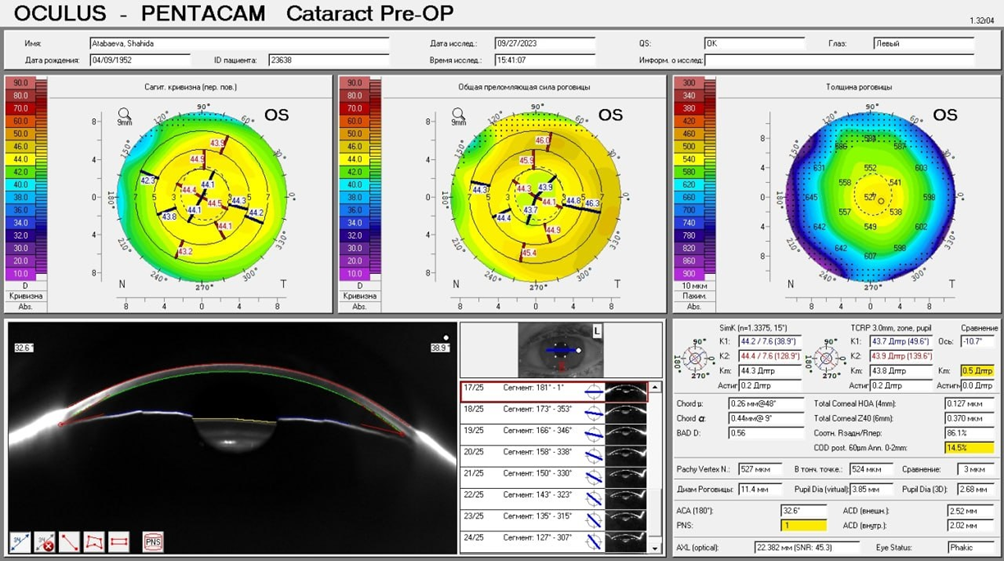 | Figure 3. Example of keratotopography from Research Group III |
4. Conclusions
- 1. High risk of Anterior Chamber Angle Closure: A higher risk of anterior chamber angle closure is observed in eyes with a thickened peripheral corneal zone (thickness greater than 685 µm). This is confirmed by the identified correlation between increased keratotopography values at the periphery and angle closure, which is an important factor contributing to the increase in intraocular pressure (IOP). Such anatomical features of the cornea may serve as markers of the risk of primary angle closure and the development of primary angle-closure glaucoma, highlighting the importance of considering them in the diagnosis and prognosis of the disease.Conversely, low keratotopography values on the periphery of the cornea (less than 685 µm) are associated with the least tendency for anterior chamber angle closure. This indicates that corneas with lower thickness in the peripheral region may reduce the likelihood of angle closure, thereby decreasing the risk of increased IOP.2. Significance of Keratotopographic Studies for Individual Risk Assessment: The results emphasize the importance of keratotopographic studies for the individual assessment of glaucoma risk. The findings support the hypothesis that corneal parameters, such as peripheral zone thickness and keratotopography, can be used as biomarkers for evaluating the risk of developing primary angle-closure glaucoma. This opens up possibilities for further clinical research aimed at optimizing methods for early diagnosis and monitoring of patients at risk.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML