-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 918-920
doi:10.5923/j.ajmms.20251504.14
Received: Mar. 3, 2025; Accepted: Mar. 28, 2025; Published: Apr. 6, 2025

Comparative Analysis of Metastatic Colorectal Cancer
Islamov Khurshid Jamshidovich
Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology, Tashkent, Uzbekistan
Correspondence to: Islamov Khurshid Jamshidovich, Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology, Tashkent, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study was performed on the basis of the coloproctology department of the Republican Medical Specialized Scientific and Practical Center of Oncology and Radiology in Tashkent. The retrospective group included data on 129 patients with colorectal cancer of stage II-IV of the disease who received surgical treatment in the department of Coloproctology of the Republican Medical Specialized Scientific and Practical Center of Oncology and Radiology. The conducted study allows us to conclude that for patients suffering from both locally advanced and metastic colon cancer and rectosigmoid junction and rectal cancer, depending on the predictors studied, there were no subgroups of death risk (and corresponding criteria) for long-term treatment outcomes.
Keywords: Colorectal cancer, Metastasis, Treatment, Long-term results
Cite this paper: Islamov Khurshid Jamshidovich, Comparative Analysis of Metastatic Colorectal Cancer, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 918-920. doi: 10.5923/j.ajmms.20251504.14.
1. Introduction
- In 2020, about 1.9 million people fell ill with colorectal cancer (CRC), and about 900,000 died, making it the second most fatal cancer after lung cancer [4]. The highest incidence in the world is observed in North America, Europe and Oceania, but the incidence is also increasing in countries with economies in transition, such as Russia, China and Brazil [1], which makes the disease an indicator of socio-economic development. CRC affects men more than women. With a global incidence of 23.4 per 100,000 male and 16.2 per 100,000 female population. CRC is a rare disease at a young age (under 40 years of age), most cases occur in the age group of 70 years and older [3]. However, there are reports of an increase in the incidence in younger age groups and that young people are diagnosed with later tumors, which indicates a real increase in the incidence, and not just a consequence of an earlier diagnosis [2,6].Inflammatory bowel diseases (IBD), that is, Crohn's disease and ulcerative colitis, increase the risk of developing CRC. Patients with IBD are under colonoscopic supervision, and the mortality rate from CRC in patients with IBD is decreasing.The International Agency for Research on Cancer and the American Institute for Cancer Research published the report "Diet, Nutrition, Physical Activity, and Colorectal Cancer in 2018," in which they reviewed published studies on lifestyle factors and CRC. They claim that the consumption of red and processed meat increases the risk of colorectal cancer, the same can be said about taking two or more servings of alcohol per day. In addition, obesity, as well as higher height, increase the risk of CRC [7]. Also, cigarette smoking increases the risk of colorectal cancer, moreover, it has been proven that the risk of CRC associated with smoking is for the rectum than for the colon [5].
2. Materials and Methods
- This study was performed on the basis of the coloproctology department of the Republican Medical Specialized Scientific and Practical Center of Oncology and Radiology in Tashkent.The study included data on 129 patients with stage II-IV colorectal cancer who received surgical treatment at the Department of Coloproctology of the Republican Medical Specialized Scientific and Practical Center of Oncology and Radiology (RMSSPCORR). The study did not include patients with primary multiple synchronous/metachronous malignancies, patients who received surgical treatment for colorectal malignancy in other medical institutions of the Republic of Uzbekistan.The diagnosis was established on the basis of complaints, medical history, physical examination, morphological examination of tumor material, data from instrumental and laboratory examination methods. The patients received adjuvant/neoadjuvant treatment in accordance with the current algorithms for the diagnosis and treatment of colorectal cancer patients approved by the Ministry of Health of the Republic of Uzbekistan. The research materials were: peripheral blood of patients, paraffin blocks of tumor tissue, freshly frozen tumor and normal colon tissues, isolated circulating tumor cells.The IBM SPSS Statistics 23 (StatSoft, USA) and MedCalc 19.3.0 (MedCalc Software, USA) programs were used to process the primary research materials.
3. Results
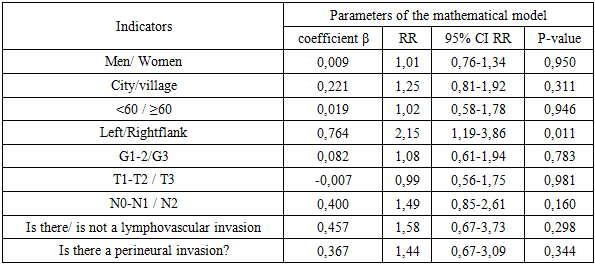
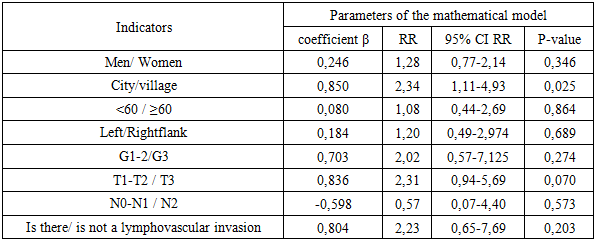
- 51.9% of the patients included in the study are men, 48.1% are women; more than 80% are urban residents.More than 90% of patients are aged 40 years and older, the least number of patients (2 patients) are aged 80 years and older. In more than half of the patients (60.5%), the malignant neoplasm had a degree of differentiation of 3, the size of the primary focus (according to the TNM classification) T3 was detected in 59.7% of patients, T4 in 36.4%, and primary lesion of regional lymph nodes was detected in 78.3% of patients. Primary distant liver metastases were detected in 58.1%, liver and other organs – in 14.7%, in other organs and dissemination - in 27.1%.The largest number of CRC patients included in the study were patients with primary colon lesions – 74 patients (57.4%), rectal tumors – 36 patients (27.9%) – in second place in terms of frequency, and rectosigmoid tumors – 19 patients (14.7%) – in third place.Metastatic colon and rectosigmoid junction cancer was detected in 93 patients: 38 men (40.9%) and 55 women (59.1%). The share of urban residents was 82.8% (77 patients), rural residents – 17.2% (16 patients). The average age of the patients was 58.4±11.8 years, the median was 60 years. This pathology was noted in 8 patients under the age of 40 years, among patients aged 80 years and older, the disease was detected in 2 (2.2%).The first degree of differentiation was identified in 8 patients (8.6%), 2 in 28 (30.1%), 3 in 57 (61.3%). According to the size of the primary focus (category T), more than half of the tumors (51.6%) are classified as T3 (48 patients), 45.2% (42 patients) as T4, and only 3.2% (3 patients) as T2.Lymphovascular invasion was detected in 80 patients (86.0%), perineural invasion – in 79.6% (74 patients).Distant liver metastases were detected in patients (53.8%), in the liver and other organs – in 12 (12.9%), dissemination and metastases in other organs – in 31 (33.3%) patients.The main method of treatment of metastatic colon cancer and rectosigmoid junction remains the surgical stage based on the RSMNPCOR.Single-stage removal of the main lesion and liver metastases was performed in 39 (41.9%) patients: 35 (70.0%) patients with liver metastases and 4 (33.3%) patients with liver and other organ metastases. Combined operations were performed in 7 (7.5%) patients with distant metastases: 1 (2.0%) patient with liver metastases, 3 (25.0%) with liver and other organ metastases, and 3 (9.7%) patients with distant metastases and dissemination.Neoadjuvant therapy (47 patients – 50.5%) using targeted drugs allowed surgical treatment of distant metastases in 31 patients (65.9%).The analysis of treatment results was based on the calculation of overall survival (OS) (1-year, 3-year and 5-year).The analysis of overall survival revealed significant (p=0.008) differences in survival rates of patients with metastatic colon cancer and rectosigmoid junction depending on the side of the lesion. Thus, the 5-year OS in the case of damage to the left flank was 42.7±7.4%, the right - 15.4± 9.2%. Five-year survival was not achieved among patients with grade 1 differentiation and without metastatic lesion of regional lymph nodes (N0) due to the small number of patients with these characteristics.When conducting a one-factor Cox regression analysis, all potential predictors that may influence treatment outcomes were included (Table 1).
|
|
4. Conclusions
- Long-term treatment results of patients with metastatic colon cancer and rectosigmoid junction were statistically significantly better among patients with left flank lesions (42.7±7.4%) compared with patients with right flank lesions (15.4±9.2%), p=0.008. Among patients with metastatic rectal cancer, the median of urban residents It was 40.0 months, among rural areas – 70.0 months, p=0.013.It was found that the risk of death from is higher among patients with metastic colon and rectosigmoid junction lesions on the left flank than on the right (HR=2.15, 95% CI 1.19-3.86, p=0.011), among patients with metastatic rectal cancer living in the mountains is higher than living in rural areas (HR=2.34 (95% CI 1.11-4.93), p=0.025). The conducted study allows us to conclude that for patients suffering from both locally advanced and metastic colon cancer and rectosigmoid junction and rectal cancer, depending on the predictors studied, there were no subgroups of death risk (and corresponding criteria) for long-term treatment outcomes. This statement does not mean that there are no such subgroups of patients, it means that if there are such subgroups, then it is not possible to distinguish these subgroups based on existing indicators determined before choosing treatment tactics.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML