-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 915-917
doi:10.5923/j.ajmms.20251504.13
Received: Mar. 2, 2025; Accepted: Mar. 27, 2025; Published: Apr. 6, 2025

Nearest Results of Surgical Treatment of Obesity in Type 2 Diabetes with Traditional Approaches to Surgical Treatment
Abdullajanov B. R., Botirov A. K., Madvaliev B. B., Botirov J. A.
Andijan State Medical Institute, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The authors report that in cases of morbid obesity (MO), understanding the mechanisms of type 2 diabetes (T2D) development or its absence will contribute to the development of preventive measures. Proximal Roux-en-Y Gastric Bypass (PRYGB) and Mini-Gastric Bypass (Mini-GB) surgeries in the treatment of obesity, including morbid obesity, improve the short-term outcomes of bariatric surgical interventions. The authors conclude that further refinement of PRYGB and Mini-GB techniques will contribute to the continued improvement of outcomes in this patient population, necessitating further research.
Keywords: Obesity, Morbid Obesity (MO), Body Mass Index (BMI), Type 2 Diabetes Mellitus (T2DM), Bariatric Surgical Interventions, Sleeve Gastrectomy (SG), Mini-Gastric Bypass (Mini-GB) Surgery
Cite this paper: Abdullajanov B. R., Botirov A. K., Madvaliev B. B., Botirov J. A., Nearest Results of Surgical Treatment of Obesity in Type 2 Diabetes with Traditional Approaches to Surgical Treatment, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 915-917. doi: 10.5923/j.ajmms.20251504.13.
1. Introduction
- According to experts from the International Diabetes Federation, by 2045, the prevalence of diabetes is expected to reach 629 million people. Type 2 diabetes mellitus (hereinafter T2DM) leads to complications such as renal failure in 40–55% of cases, cardiovascular diseases in 50–60%, and is often a cause of lower limb amputations [4]. Obesity has reached epidemic proportions among non-communicable diseases in recent decades: in 2016, 39% of adults worldwide were classified as overweight or obese [5]. In the member countries of the Organisation for Economic Co-operation and Development (OECD), 54% of the population has an excessive BMI, including 19% suffering from morbid obesity (hereinafter MO). There is a strong causal relationship between obesity and T2DM [6,7]. Understanding the mechanisms of T2DM development or its absence in MO cases will contribute to the development of preventive measures, which served as the basis for this study.
2. Materials and Methods
- This study is based on the results of a retrospective and prospective analysis of patients with morbid obesity (MO) and type 2 diabetes mellitus (T2DM) who underwent surgical treatment between 2023 and 2024 at the private clinic "Sehat" in Andijan and the Third Surgical Department of the Clinic of Andijan State Medical Institute. The study included 159 patients with obesity, including cases of MO with T2DM. According to the study’s objectives, the patients were conditionally divided into two groups:• Comparison group (2023) – 57 patients (35.8%) who underwent a retrospective analysis of surgical treatment outcomes following traditional approaches.• Main group (2024) – 102 patients (64.2%) who were prospectively studied for surgical treatment outcomes using a differentiated approach to bariatric interventions.It is important to note that during the examination, diagnosis, preoperative preparation, selection of bariatric surgical methods, and postoperative management of patients with obesity and T2DM, all procedures were carried out in accordance with the latest universally recognized clinical guidelines [2], which have been adopted and approved by the Ministry of Health of our Republic.
3. Results and Discussion
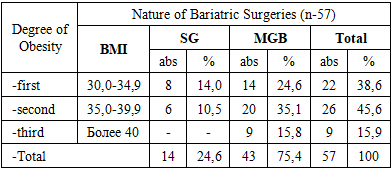
- According to the study’s objectives, the comparison group (2023) consisted of 67 patients (42.1%), who underwent a retrospective analysis of surgical treatment outcomes for MO with T2DM following traditional approaches.The distribution of patients was carried out according to the International Age Classification of the WHO [1].• Among the 57 patients with MO and T2DM in the comparison group, 18 patients (31.6%) belonged to the 19–44 age category, including 8 men (14.0%) and 10 women (17.5%).• The 45–59 age category included 39 patients (68.4%), representing individuals of the most economically active age, which holds significant medical and economic importance. Among them, 20 men (35.1%) and 19 women (33.3%) were recorded.The retrospective analysis showed that in the comparison group, the ratio of men to women with MO and T2DM was 1:1.Among the 57 patients with MO and T2DM in the comparison group: 22 cases (38.6%) had first-degree obesity (BMI: 30.0–34.9), including 13 men (22.8%) and 9 women (15.8%); 26 cases (45.6%) had second-degree obesity (BMI: 35.0–39.9), including 12 men (21.0%) and 14 women (24.6%).The degree of obesity and duration of T2DM play a crucial role in determining surgical tactics for the studied patients.For first-degree obesity (22 patients, 38.6% in the comparison group): T2DM duration ≤2 years – 7 cases (12.3%), 2–5 years – 12 cases (21.1%), 6–10 years – 1 case (1.7%), >10 years – 2 cases (3.5%).For second-degree obesity (26 patients, 45.6% in the comparison group): T2DM duration ≤2 years – 4 cases (7.0%), 2–5 years – 10 cases (17.5%), 6–10 years – 9 cases (15.8%), >10 years – 3 cases (5.3%).For third-degree obesity (morbid obesity, MO) (9 patients, 15.9% in the comparison group): T2DM duration ≤2 years – 1 case (1.8%), 2–5 years – 1 case (1.8%), 6–10 years – 4 cases (7.0%), >10 years – 3 cases (5.3%).Comorbid therapeutic pathologies were observed in 10 cases (17.5%) with first-degree obesity, 13 cases (22.8%) with second-degree obesity, 9 cases (15.8%) with third-degree (morbid) obesity.A retrospective analysis of bariatric surgery outcomes revealed a significant impact of comorbid pathologies on surgical treatment results.In the comparison group, among patients with obesity and T2DM, the types of performed surgical interventions are presented in Table 1.
|
4. Conclusions
- Thus, in morbid obesity, understanding the mechanisms underlying the development of type 2 diabetes—or its absence—will contribute to the development of preventive measures. SG and MGB procedures in obesity surgery, including for morbid obesity, improve short-term outcomes of bariatric interventions. However, further refinement of SG and MGB techniques will lead to even better outcomes for this patient cohort.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML