Abdullajanov B. R., Boltaev A. A., Botirov J. A.
Andijan State Medical Institute, Republic of Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The aim of the research: To improve treatment outcomes for patients with various forms of varicose vein disease by incorporating endovenous laser obliteration (EVLO) into comprehensive treatment. Materials and Methods: This scientific research is based on the results of research conducted on 267 patients with varicose veins of the lower extremities who underwent surgery at the Angiomed Clinic in Davlatabad District, Namangan Region, from 2020 to 2023. All patients were divided into three groups. The first group included 104 (38.9%) patients who underwent traditional phlebectomy. The second group consisted of 107 (40.1%) patients who underwent EVLO combined with miniphlebectomy of the great saphenous vein simultaneously. The third (main) group comprised 56 (20.9%) patients who underwent EVLO followed by sclerotherapy or miniphlebectomy after three months. Results: A comparative analysis of the short-term outcomes of surgical treatment in the studied patient groups showed that phlebectomy complications were observed in 17 (6.4%) patients overall, including 11 (10.6%) cases in the first group, 5 (4.7%) cases in the second group, and 1 (1.9%) case in the third group. This represents a reduction of 8.7%. Complications of EVLO were identified in a total of 34 (12.7%) patients, including 29 (27.1%) cases in the second group and 5 (8.9%) cases in the third group, showing a reduction of 18.2%. Determined complications of EVLO were identified in a total of 28 (10.5%) patients, including 14 (13.1%) cases in the second group and 4 (7.2%) cases in the third group, showing a reduction of 5.9%. Stochastic complications of EVLO were identified in a total of 12 (4.5%) patients, including 11 (10.3%) cases in the second group and 1 (1.8%) case in the third group, showing a reduction of 5.5%. Complications of EVLO associated with the fiber optic were identified in a total of 18 (6.7%) patients, including 16 (14.9%) cases in the second group and 2 (3.6%) cases in the third group, showing a reduction of 11.3%. Minor complications were identified in a total of 115 (43.1%) patients, including 67 (64.4%) cases in the first group, 39 (36.5%) cases in the second group, and 9 (16.1%) cases in the third group, showing a reduction of 48.3%. Major complications were identified in a total of 6 (2.3%) patients, including 4 (3.8%) cases in the first group, 2 (1.8%) cases in the second group, and no major complications in the third group, showing a 100% improvement. General complications were identified in a total of 53 (19.8%) patients, including 28 (26.9%) cases in the first group, 18 (16.8%) cases in the second group, and 7 (12.5%) cases in the third group, showing an improvement of 14.4%. Conclusion. Summarizing the results, it should be noted that in the long-term follow-up period, when evaluating the total scores, no statistically significant differences were found among patients who underwent different interventions. The effectiveness of a particular treatment option for chronic venous disease of the lower extremities (CVDLE) should be confirmed by clinical and instrumental diagnostic methods, as well as data on the frequency of complications and recurrences. The results of the study provide valuable additional information that can improve the interaction between doctors and patients to achieve better treatment outcomes.
Keywords:
Surgery, Varicose veins, Lower limb veins, Treatment
Cite this paper: Abdullajanov B. R., Boltaev A. A., Botirov J. A., Comparative Evaluation of Treatment Methods for Patients with Varicose Veins of the Lower Extremities, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 907-914. doi: 10.5923/j.ajmms.20251504.12.
1. Introduction
Chronic venous diseases include varicose disease (primary varicose vein dilation), post-thrombotic disease, reticular varicose veins and telangiectasia, venous malformations, and functional venous insufficiency.Some international studies indicate that chronic venous insufficiency (CVI) is most commonly observed in 60–75% of the population and in more than 80% of elderly patients [4,13,17]. Complications of CVI are detected in 42% of patients, with lower limb edema occurring in 10%, skin changes in 37%, trophic ulcers of the lower extremities in 11%, and open ulcers in 3% of cases [7,15,19,21].The treatment of the disease should be comprehensive and include lifestyle modifications, elastic compression, and both conservative and surgical treatment methods [1,8,11,18,20]. In cases where various pathogenic factors, the severity of varicose dilation of the saphenous veins, and complications of the primary disease are present, conservative therapy alone cannot eliminate the symptoms. As a result, specialists opt for a specific type of surgical intervention.Phlebectomy, considered a classical and radical surgical treatment for varicose veins, has undergone significant modifications. Only those saphenous veins where the pathological process is irreversible and resistant to conservative treatment are removed [2,5,9,12,19,22].Most specialists support treating varicose vein patients in outpatient and polyclinic settings, a trend largely facilitated by the development of minimally invasive surgery. One of the most promising minimally invasive techniques is endovenous laser ablation (EVLA) [3,6,10,14,16].Globally, research on the morphological and functional aspects of disease development, progression, pathogenesis, and treatment selection remains highly relevant. This study represents the outcome of research aimed at addressing these issues.The aim of the research was to improve treatment outcomes for patients with various forms of varicose vein disease by incorporating endovenous laser ablation (EVLA) into comprehensive treatment.
2. Materials and Methods
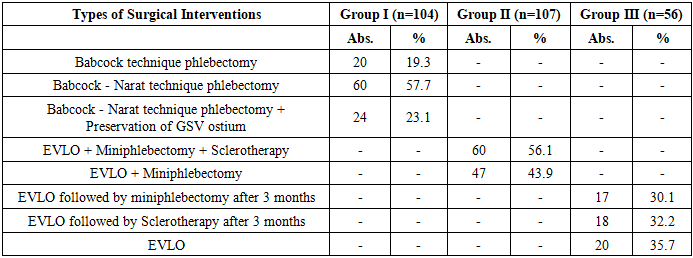
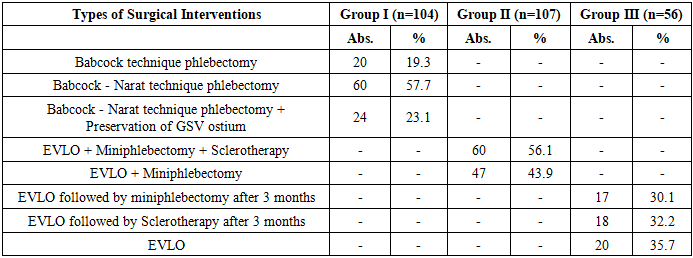
This scientific research is based on the results of an investigation involving 267 patients with varicose vein disease of the lower extremities who underwent surgery at the Angiomed Clinic in Davlatabad District, Namangan Region, between 2020 and 2023.All patients were divided into three groups. The first group consisted of 104 patients (38.9%) who underwent traditional phlebectomy. The second group included 107 patients (40.1%) who underwent EVLA combined with miniphlebectomy of the great saphenous vein simultaneously. The third (main) group consisted of 56 patients (20.9%) who underwent EVLA, followed by sclerotherapy or miniphlebectomy after three months.The type of surgical intervention plays a significant role in treatment outcomes. The different types of surgical procedures performed are presented in Table 1.Table 1. Types of Surgical Interventions
 |
| |
|
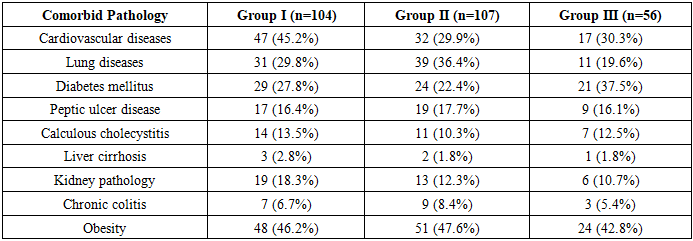
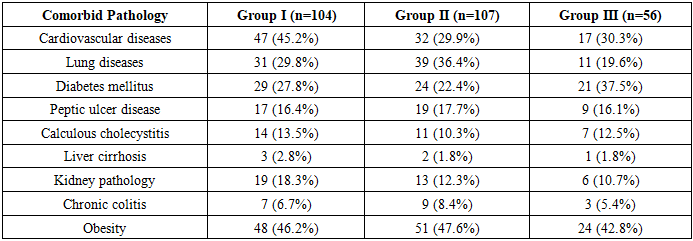
Among the 104 patients in the first group, phlebectomy using the Babcock method was performed in 20 cases (19.3%), the Babcock-Narat method was used in 60 cases (57.7%), and in 24 cases (23.1%), surgery was conducted using the Babcock-Narat method along with SSV ostium ligation.Among the 107 patients in the second group, surgery was performed using the EVLO + miniphlebectomy + sclerotherapy method in 60 cases (56.1%), while EVLO + miniphlebectomy was carried out in 47 cases (43.9%).Among the 56 patients in the third group, surgical interventions were performed using the EVLO method followed by miniphlebectomy after 3 months in 17 cases (30.1%), EVLO followed by sclerotherapy after 3 months in 18 cases (32.2%), and EVLO alone in 20 cases (35.7%).The analysis of anamnesis data in the compared groups revealed that among 122 patients with varicose disease, the duration of the disease was up to 1 year in 6 patients from the control group and 7 from the main group; 1–3 years in 11 patients from the control group and 14 from the main group; and more than 3 years in 41 patients from the control group and 43 from the main group.Among all patients with CVI lasting more than 3 years, 142 (53.2%) were hospitalized, while 77 (28.8%) with a disease duration of 1–3 years and 48 (17.9%) with a disease duration of up to 1 year were hospitalized.The presence of comorbidities plays an important role in ensuring a positive treatment outcome.In this regard, an analysis of comorbid pathologies in this category of patients was conducted, as presented in Table 2. The most common comorbid diseases were cardiovascular diseases, which were identified in 47 (45.2%) patients of the first group, 32 (29.9%) patients of the second group, and 17 (30.3%) patients of the third (main) group.Table 2. Nature of comorbid pathology in the compared groups
 |
| |
|
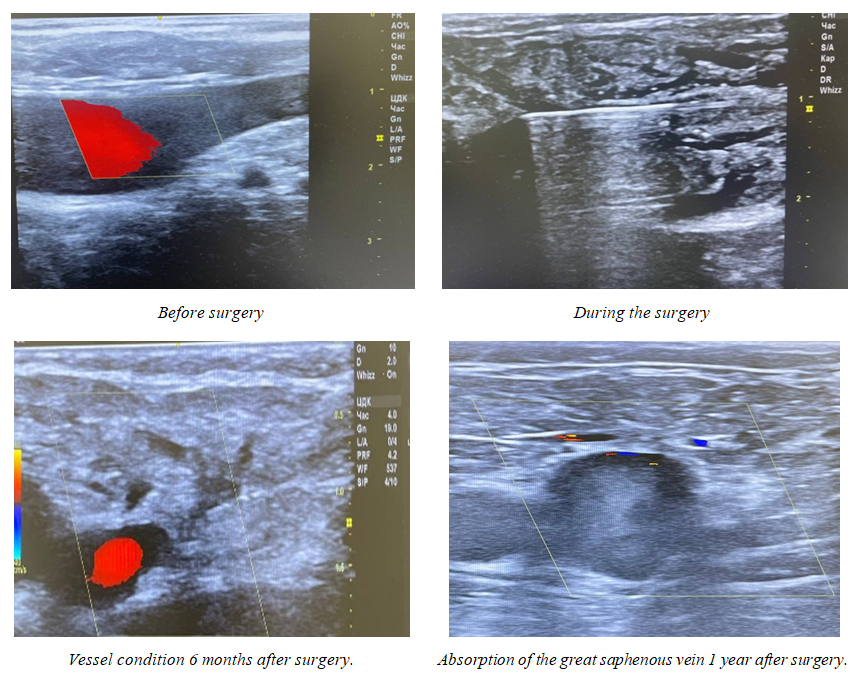
Among other pathologies in the compared groups, lung diseases were the most frequently encountered, diagnosed in 31 (29.8%) patients of the first group, 39 (36.4%) patients of the second group, and 11 (19.6%) patients of the third group. Diabetes mellitus was detected in 29 (27.8%) patients of the first group, 24 (22.4%) patients of the second group, and 21 (37.5%) patients of the third group.Among the specific symptoms of chronic venous insufficiency (CVNI), particular attention was paid to the presence of pain, trophic ulcers, heaviness in the legs, burning sensation, and others. The frequency of symptoms is presented in Figure 1.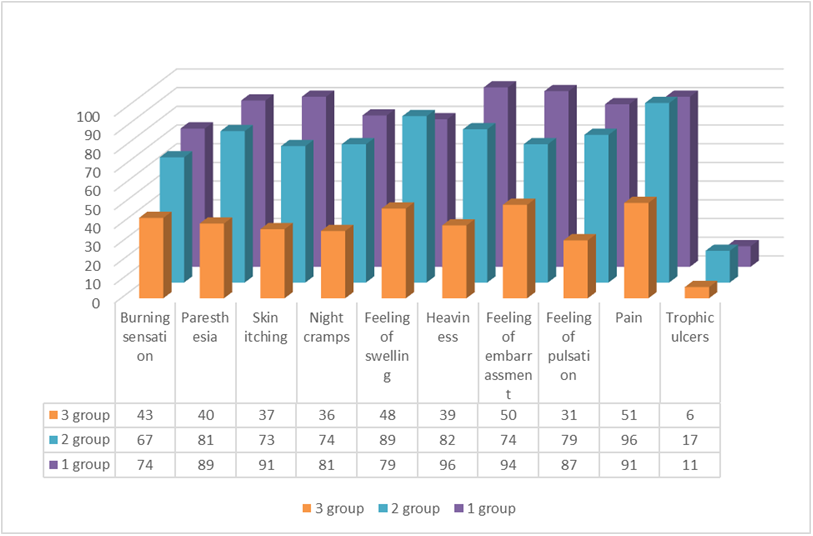 | Figure 1. Specific Symptoms of CVI |
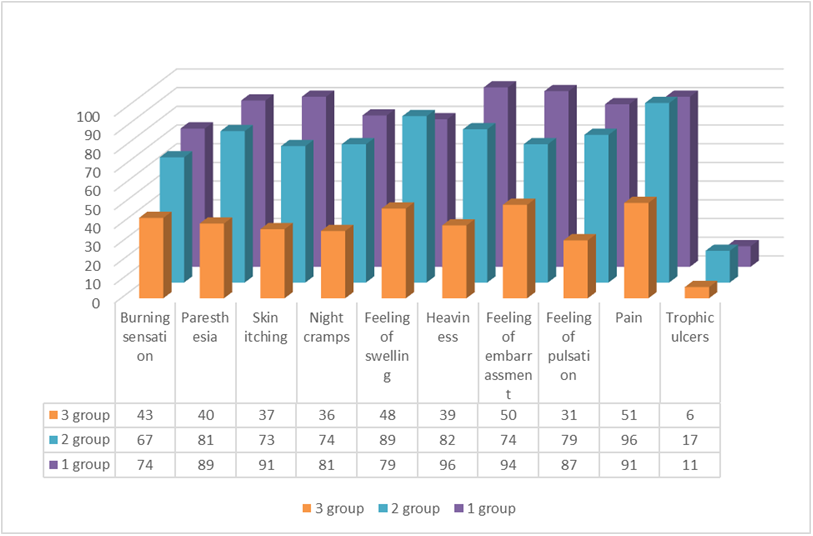
As seen in Figure 1, the percentage distribution of specific symptoms was approximately equal across all groups, indicating a similar clinical course of the disease in all three patient groups.The therapeutic measures for CVI were aimed at preventing the spread of thrombosis to deep veins, rapidly alleviating pain symptoms, and preventing complications. The order and methods for addressing these issues were determined by the localization and extent of the pathological process.In the first observation group (n=104), cases were considered where single-stage phlebectomy was performed. After hospitalization, all patients underwent preoperative conservative therapy before proceeding to traditional phlebectomy.In the second group (n=107), after diagnosis verification and preoperative preparation, patients underwent Endovenous Laser Obliteration (EVLO) + Mini-Phlebectomy of the great saphenous vein simultaneously.EVLO Procedure Technique: Skin marking was performed under ultrasound guidance immediately before the intervention. First, the lower boundary of reflux along the great saphenous vein was determined.A mark was placed at the site of a large tributary’s inflow. The second mark was placed 3–4 cm distal to the first, indicating the puncture site of the vein. Then, along the great saphenous vein, all tributary inflow points were marked. This was done to ensure a prolonged laser exposure at these sites during EVLO to seal the tributary openings.Next, all varicose tributaries were marked, regardless of the method of removal (Figure 2).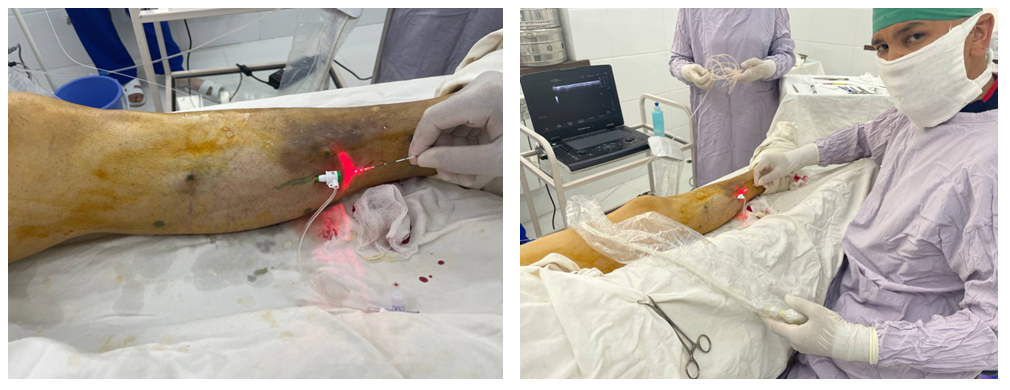 | Figure 2. EVLO Procedure Process |
Next, the positioning of the working part of the laser fiber is performed, followed by the creation of tumescent anesthesia. Then, endovenous laser obliteration (EVLO) is carried out, and compression hosiery is applied. After completing EVLO, the procedure moves on to the stages of miniphlebectomy.The third (main) group consisted of 56 patients who underwent EVLO, followed by deferred sclerotherapy or miniphlebectomy three months later. Surgical treatment was performed exclusively in a planned manner.Indications for Postponing Miniphlebectomy or Sclerotherapy After EVLO:• Presence of other comorbidities that do not prevent surgery.• A large number of varicose veins.• Detection of abnormalities in laboratory test results.• Diffuse positioning of the great saphenous vein, its bifurcation (multiple branches), and various anatomical variations.• Presence of valve insufficiency in both the great and small saphenous veins, along with a significant number of varicose veins.The patient was assigned a two-stage procedure: EVLO in the first stage, followed by miniphlebectomy or sclerotherapy in the second stage after three months. In some cases, indications for miniphlebectomy and sclerotherapy were not determined, and no further treatment was provided.The patient returns for a follow-up visit the day after the procedure. An examination is conducted using Doppler ultrasound.Control check-ups are scheduled 12 days and one month after the procedure, during which patients receive necessary recommendations regarding self-care, prevention of complications, and disease recurrence.Based on the above findings, a treatment strategy was developed by dividing the patients in the main group into three subgroups according to the results of a follow-up examination after three months.In the first case: The patient's complaints are heard during a physical examination, and a follow-up Doppler study is conducted. If no varicose vein enlargement is detected during the examination and no changes in the veins are found in the Doppler study, no further intervention is performed. The patient is given the necessary recommendations and discharged home.In the second case: Patients undergoing a follow-up examination are objectively assessed, their complaints are heard, and a Doppler study is performed. If varicose vein enlargement is detected through general and local examination, as well as Doppler imaging, sclerotherapy is performed for small veins with a diameter of 3–4 mm. If the diameter exceeds 4–5 mm, miniphlebectomy is performed.Contraindications to sclerotherapy include:• Pregnancy and lactation• Allergy (to the administered drug)• Severe atherosclerosis• Current or past thrombosis and thrombophlebitis• Heart defects• Presence of local infectious or inflammatory processesPre-sclerotherapy requirements:• Avoid using creams and ointments on the day of the procedure• Refrain from smoking and alcohol consumption for 2 days• Eat a light meal 1.5–2 hours before the procedure• Take a hygienic shower before the procedurePatients are allowed to walk and go home 25–30 minutes after the procedure.In the third case: The patient comes for a follow-up examination, their complaints are assessed objectively, their general and local condition is evaluated, and a Doppler study is performed. After diagnosing, if the vein diameter exceeds 4–5 mm, a miniphlebectomy is recommended using the method described above.
3. Results
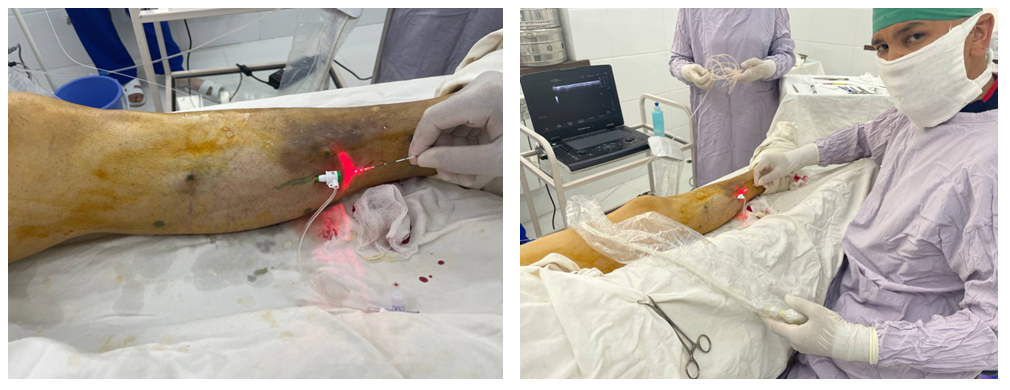
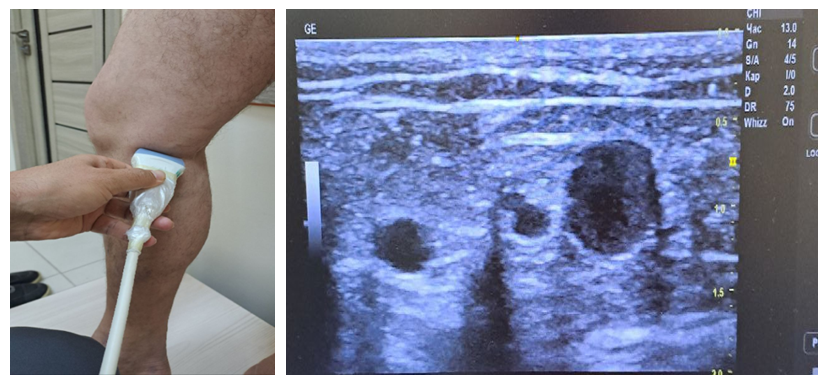
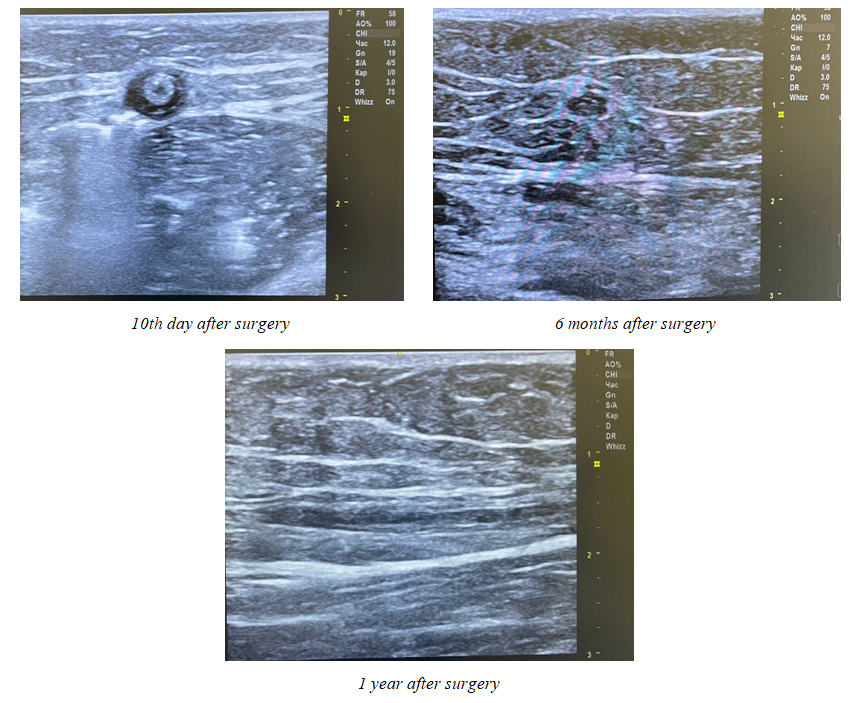
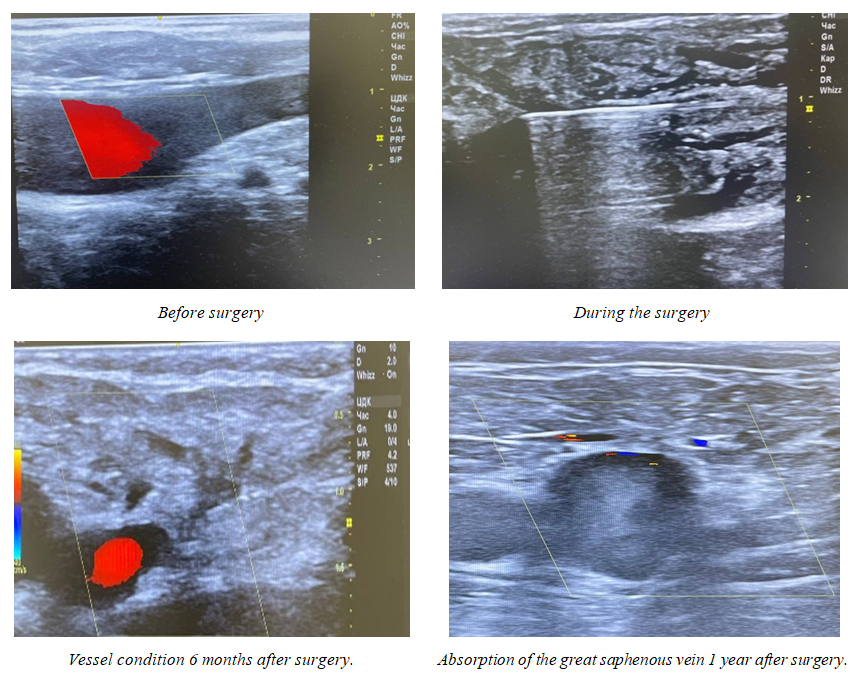
The immediate results of surgical treatment are of great importance for all categories of surgical patients. Complications after phlebectomy were observed in 17 patients. Among them, complications were detected in:• 11 patients (10.6%) from the first group• 5 patients (4.7%) from the second group after EVLO + miniphlebectomy• 1 patient (1.9%) from the third group after delayed miniphlebectomyIt should be noted that the primary complication was damage to the cutaneous sensory nerves.Complications related to EVLO were identified in 34 patients, accounting for 12.7% of the total number of patients (267). Among them, complications were observed in: 29 patients (27.1%) from the second group; 5 patients (8.9%) from the third group.It should be noted that the most frequent complication (in 30 patients) was pain in the operated limb. Additionally, short-term low-grade fever was observed in 21 patients.A comparative analysis of the short-term outcomes of surgical treatment in the studied groups showed that phlebectomy complications were detected in 17 patients (6.4%) overall, distributed as follows: 11 patients (10.6%) in the first group; 5 patients (4.7%) in the second group; 1 patient (1.9%) in the third group. This represents a reduction of 8.7%.EVLO-related complications were identified in 34 patients (12.7%) overall: 29 cases (27.1%) in the second group; 5 cases (8.9%) in the third group. This represents a reduction of 18.2%.Determined EVLO-related complications were observed in 28 patients (10.5%) overall: 14 cases (13.1%) in the second group; 4 cases (7.2%) in the third group. This represents a reduction of 5.9%.Stochastic complications of EVLO were identified in a total of 12 (4.5%) patients, including 11 (10.3%) cases in the second group and 1 (1.8%) case in the third group. Reduction by 5.5%. Complications of EVLO related to the optical fiber were detected in a total of 18 (6.7%) patients, including 16 (14.9%) cases in the second group and 2 (3.6%) cases in the third group. Reduction by 11.3%. Minor complications were observed in a total of 115 (43.1%) patients, including 67 (64.4%) cases in the first group, 39 (36.5%) cases in the second group, and 9 (16.1%) cases in the third group. Reduction by 48.3%. Major complications were identified in a total of 6 (2.3%) patients, including 4 (3.8%) cases in the first group, 2 (1.8%) cases in the second group, and no major complications in the third group. Improvement by 100%. General complications were observed in a total of 53 (19.8%) patients, including 28 (26.9%) cases in the first group, 18 (16.8%) cases in the second group, and 7 (12.5%) cases in the third group. Improvement by 14.4%.Among the studied patients, follow-up examinations at 3 months were conducted for 87 (83.6%) patients in the first group, 92 (85.9%) patients in the second group, and 49 (87.5%) patients in the third group. At 6 months, examinations were performed for 83 (79.8%) patients in the first group, 86 (80.1%) patients in the second group, and 41 (73.2%) patients in the third group.At 1 year, follow-up was conducted for 67 (64.4%) patients in the first group, 71 (66.4%) patients in the second group, and 36 (64.3%) patients in the third group. After more than 3 years, examinations were completed for 54 (51.9%) patients in the first group, 71 (66.4%) patients in the second group, and 29 (51.8%) patients in the third group.In the first group, control ultrasound duplex scanning and MSCT examinations performed between 6 months and 1 year postoperatively showed a significantly higher incidence of reflux in the thigh region in 28 (26.9%) patients compared to 17 (15.8%) patients in the second group and 2 (3.6%) patients in the third group (p <0.05).An example of instrumental examination data for patients in the first group is shown in Figure 3, for the second group in Figure 4, and for the third group in Figure 5.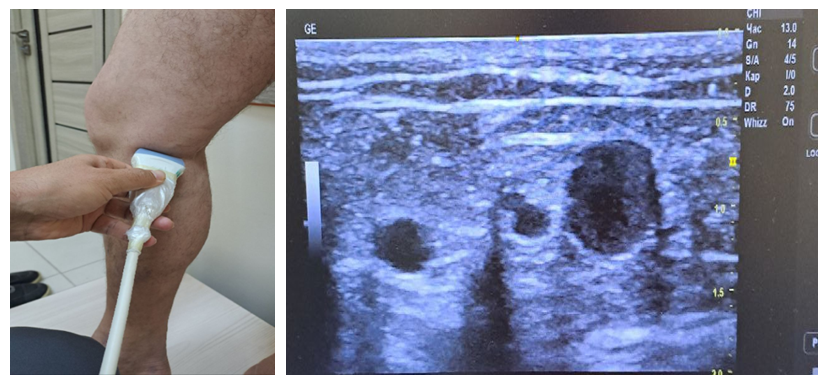 | Figure 3. Ultrasound examination of first-group patients at 6 months postoperatively |
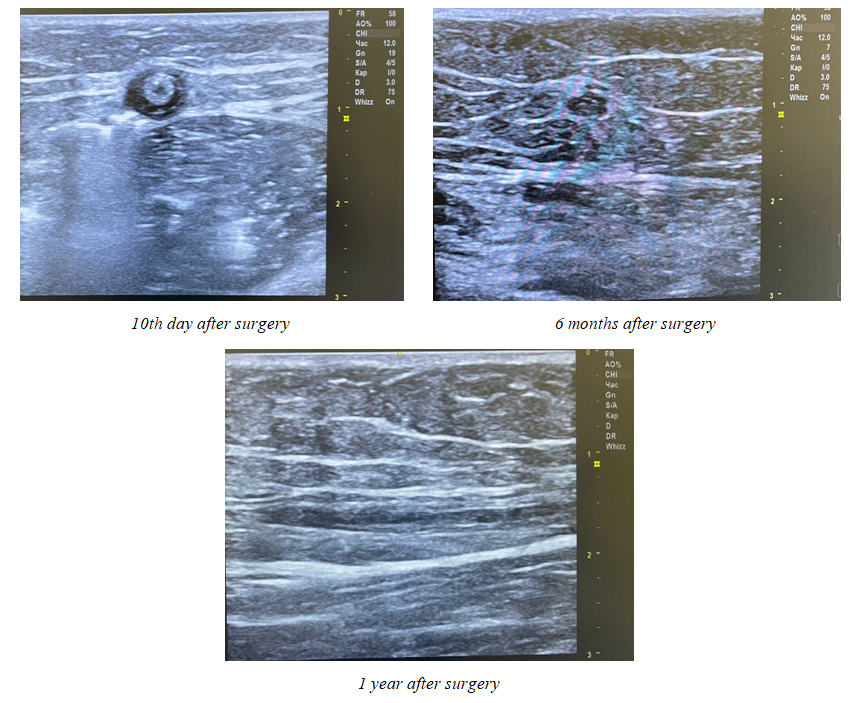 | Figure 4. Ultrasound examination of patients in the second group at 10 days, 6 months, and 1 year after surgery |
 | Figure 5. Ultrasound examination of patients in the third group before surgery, during surgery, and at 6 months and 1 year after surgery |
The treatment outcomes between 6 months and 1 year postoperatively correlated with the incidence of clinical recurrence of varicose veins: in the first group, recurrence was observed in 16 (15.4%) cases, in the second group in 7 (6.5%) cases, while no recurrences of varicose veins were recorded in the third group.Among the 54 patients in the first group, at more than 3 years post-surgery, reflux in the thigh was detected in 3 (5.5%) cases, reflux in the lower leg in 4 (7.4%) cases, and recurrence of varicose disease in 2 (3.7%) cases. Among the 62 patients in the second group, at more than 3 years post-surgery, reflux in the thigh was detected in 3 (4.8%) cases, reflux in the lower leg in 2 (3.2%) cases, and recurrence of varicose disease in 1 (1.6%) case. Meanwhile, among the 29 patients in the third group, at more than 3 years post-surgery, reflux in the thigh was detected in 1 (3.4%) case. It should be noted that in the third group, at more than 3 years post-surgery, no cases of reflux in the lower leg or recurrence of varicose disease were detected.Summarizing the results, it should be stated that in the long-term follow-up period, when assessing the total scores, no statistically significant differences were found among patients who underwent different interventions. The effectiveness of a particular treatment approach for chronic venous disease should be confirmed by clinical and instrumental diagnostic methods, as well as data on the frequency of complications and recurrences. The study results provide valuable additional information that can enhance physician-patient interaction to achieve better treatment outcomes.
References
| [1] | Babajanov A.S., Tukhtaev Zh.K., Toirov A.S., et al. Comparison of the effectiveness of endovenous laser coagulation and traditional combined phlebectomy. Science and World. 2017. Vol. 1. No. 5. pp. 85-87. ISSN: 2308-4804. |
| [2] | Volkov A.S., Dibirov M.D., Shimanko A.I., et al. Comparison of the results of endovenous laser and radiofrequency obliteration of the great saphenous vein trunk in the comprehensive treatment of patients with varicose veins of the lower extremities. Phlebology. 2020. Vol. 14, No. 2. pp. 91-98. |
| [3] | Gavrilenko A.V., Vakhratyan P.E., Arakelyan A.G. Endovenous methods for treating varicose veins of the lower extremities: A literature review. Laser Medicine. 2022; 26(2): 31-36. https://doi.org/10.37895/2071-8004-2022-26-2-31-36. |
| [4] | Kamaev A.A., Bulatov V.L., Vakhratyan P.E., et al. Varicose veins. Phlebology. 2022. Vol. 16, No. 1. pp. 41-108. |
| [5] | Lobastov K.V. Implementation of the eASVAL principle: The impact of endovenous laser obliteration of the perforating vein and/or sclerotherapy of varicose tributaries on the course of varicose disease in the great saphenous vein system. Phlebology. 2019. Vol. 13, No. 2. pp. 98-111. |
| [6] | Mikhailov I.P., Kozlovsky B.V., Arustamyan V.A. Surgical treatment of varicose veins of the lower extremities. N.V. Sklifosovsky Journal of Emergency Medical Care. 2023; 12(3): 471-480. https://doi.org/10.23934/2223-9022-2023-12-3-471-480. |
| [7] | Pryadko S.I. Immediate and long-term results of various surgical treatment methods for patients with acute varicothrombophlebitis. Annals of Surgery. 2019. Vol. 24, No. 2. pp. 115-120. |
| [8] | Tazhiev S.Z. Optimization of treatment methods for patients with chronic venous insufficiency of the lower extremities. PhD dissertation in medical sciences. 2023. p. 120. |
| [9] | Al Shakarchi J, Wall M, Newman J. The role of compression after endovenous ablation of varicose veins. J Vasc Surg Venous Lymphat Disord. 2018 Jul; 6(4): 546-550. |
| [10] | Bissacco, D, Stegher, S, Calliari, FM. Saphenous vein ablation with a new cyanoacrylate glue device: a systematic review on 1000 cases. Minim Invasive Ther Allied Technol. 2019; 28(1): 6-14. https://doi.org/10.1080/13645706.2018.1464029. |
| [11] | Chen S, Zeng Q, Fu Q, Li F, Zhang M, Zhao Y. Transilluminated powered phlebectomy in the treatment of large area venous leg ulcers: A case-control study with 3 years follow-up. Microcirculation. 2019 Apr; 26(3): e12523. |
| [12] | Farah M.H. A systematic review supporting the Society for Vascular Surgery, the American Venous Forum, and the American Vein and Lymphatic Society guidelines on the management of varicose veins // J. Vasc. surgery. Venous Lymphat. Disord. - 2022. - Vol. 10, № 5. - P. 1155-1171. |
| [13] | Gibson K, Minjarez R, Gunderson K, Ferris B. Need for adjunctive procedures following cyanoacrylate closure of incompetent great, small and accessory saphenous veins without the use of postprocedure compression: Three-month data from a postmarket evaluation of the VenaSeal System (the WAVES Study). Phlebology. 2019; 34(4): 231-237. https://doi.org/10.1177/ 0268355518801641. |
| [14] | Karsten H. Endovenous minimally invasive procedures for treatment of varicose veins: The gentle and effective alternative to high ligation and stripping operations. Hautarzt. 2020; https://doi.org/):12-19. DOI:10.1007/s00105-019-04520-2. |
| [15] | Larsson S.C., Burgess S. Appraising the causal role of smoking in multiple diseases: A systematic review and meta-analysis of Mendelian randomization studies. EBioMedicine. 2022 Aug; 82: 104154. |
| [16] | Lurie F, Lal BK, Antignani PL. Compression therapy after invasive treatment of superficial veins of the lower extremities: Clinical practice guidelines of the American Venous Forum, Society for Vascular Surgery, American College of Phlebology, Society for Vascular Medicine, and International Union of Phlebology. J Vasc Surg Venous Lymphat Disord. 2019 Jan; 7(1): 17-28. |
| [17] | Maeseneer M. G. De Editor’s Choice - European Society for Vascular Surgery (ESVS) 2022 Clinical Practice Guidelines on the Management of Chronic Venous Disease of the Lower Limbs // Eur. J. Vasc. Endovasc. Surg. - 2022. - Vol. 63, № 2. - P. 184-267. |
| [18] | Pompilio G. Systematic literature review and network Meta-analysis of sulodexide and other drugs in chronic venous disease // Phlebology. - 2021. - Vol. 36, № 9. - P. 695-709. |
| [19] | Shadrina A.S, Elgaeva E.E, Stanaway I.B. Mendelian randomization analysis of plasma levels of CD209 and MICB proteins and the risk of varicose veins of lower extremities. PLoS One. 2022; 17(5): e0268725. |
| [20] | Yetkin E, Kutlu Karadag M, Ileri M. Venous leg symptoms, ecchymosis, and coldness in patients with peripheral varicose vein: A multicenter assessment and validation study (VEIN-VIOLET study). Vascular. 2021 Oct; 29(5): 767-775. |
| [21] | Yuan S., Bruzelius M., Damrauer S.M. Cardiometabolic, Lifestyle, and Nutritional Factors in Relation to Varicose Veins: A Mendelian Randomization Study. J Am Heart Assoc. 2021 Nov 02; 10(21): e022286. |
| [22] | Zalewski DP, Ruszel KP, Stępniewski A. miRNA Regulatory Networks Associated with Peripheral Vascular Diseases. J Clin Med. 2022 Jun 16; 11(12). |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML