-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 810-816
doi:10.5923/j.ajmms.20251503.67
Received: Feb. 23, 2025; Accepted: Mar. 15, 2025; Published: Mar. 22, 2025

The Detailed Analysis of the Mechanisms Resulting to Lethal Outcome in Patients with Severe Traumatic Brain Injury
A. L. Rosstalnaya1, 2, H. H. Dadaev2, A. U. Takhirov2
1Center for the Development of Professional Qualification of Medical Workers, Tashkent, Uzbekistan
2Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

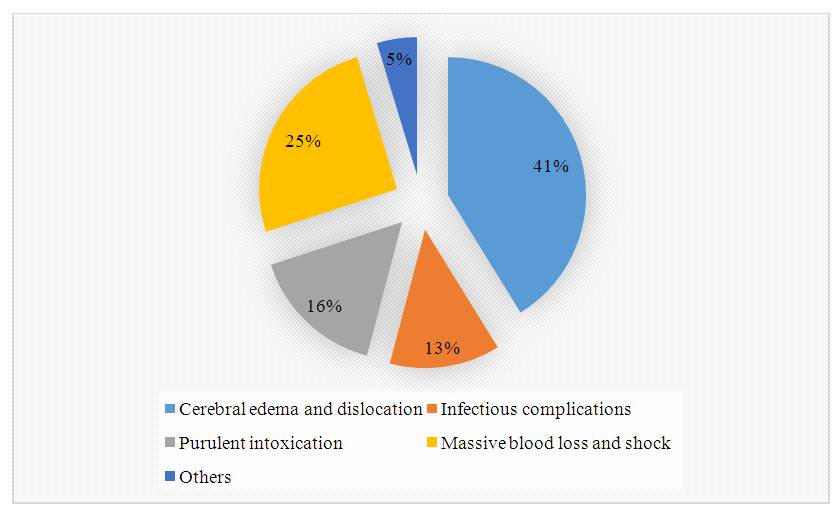
The aim of the study was to conduct a detailed analysis of the mechanisms leading to lethality in patients with severe traumatic brain injury, as well as to study the clinical epidemiology and identify the main causes of hospital mortality at different stages of experiencing severe traumatic brain injury. A detailed analysis of the main causes of fatal outcomes in victims with severe traumatic brain injury who were admitted to the neurosurgical ICU of the Republican Research Center of Emergency Medicine for the period from 2023 to 2024 was performed in this article. The total number of admitted patients was 948: 699 (74%) of them were diagnosed with severe traumatic brain injury. The overall mortality differed by years and was 15.25% and 16.67%, respectively. Ninety-two patients out of 699 victims with traumatic brain injury died at various time after receiving the injury. There were 74 (80.4%) males and 26 (19.6%) females among the deceased. The mean age was 42.3±12.5 years. In 41.2% of patients the main cause of death was cerebral edema and dislocation, in 25.3% - massive blood loss and shock (traumatic and/or hemorrhagic), in 15.9% - purulent-septic complications. Sepsis and septicemia were the main cause of death in 18.5% of the patients, and the average duration of hospital stay was 28.4±16.5 days. Almost half of the patients had a combination of two or more complications. A statistically significant relationship between the severity of trauma, the development of infectious complications, the main causes of death, on the one hand, and the terms of fatal outcomes, on the other hand, was revealed.
Keywords: Severe traumatic brain injury, Combined severe traumatic brain injury, Mortality, Main causes of death, Timing of death
Cite this paper: A. L. Rosstalnaya, H. H. Dadaev, A. U. Takhirov, The Detailed Analysis of the Mechanisms Resulting to Lethal Outcome in Patients with Severe Traumatic Brain Injury, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 810-816. doi: 10.5923/j.ajmms.20251503.67.
Article Outline
1. Introduction
- The injury epidemic has become one of the major medical and social problems in industrialized countries, requiring huge financial expenditures for its solution [1,2]. Traumatism ranks the 3rd and the 4th after cardiovascular diseases, stroke, respiratory diseases, and infectious diseases in the mortality structure of the population of economically developed and developing countries [3,4]. Modern scientific and practical achievements of medicine have allowed to slightly reduce lethality in combined severe traumatic brain injuries (CSTBI). However, traumatic brain injury and its consequences occupy one of the leading places in the structure of neurological morbidity, and this problem, despite the great attention that is constantly paid to it, is still topical [5]. According to the World Health Organization, the incidence of severe traumatic brain injury (STBI) is increasing by 2.2% per year, with an increasing incidence of more severe types of injury [3,6,7]. Speaking about the mechanism of traumatic brain injury, in 40-50% of cases the cause is road traffic accidents (RTAs), in 17% of cases the injury occurs as a result of fights or attacks, and in about 13% the cause is catatrauma. In most cases, STBI is associated with other injuries, often with chest trauma (30-40% of all CSTBI cases). In 3-8% of STBI there are concomitant cervical spine injuries [1,8]. The high incidence of illness and mortality caused by traumatic brain injury, especially among young and able-bodied citizens, takes this pathology beyond the scope of a purely medical problem and elevates it to the level of one of the most important social issue [5,9].According to the data of the Institute of Health under the Ministry of Health of the Republic of Uzbekistan, severe traumatic brain injury occupies one of the leading places in the structure of lethality, making from 10 to 50% of all traumatic injuries. Mortality in TBI is 5-10%, and in STBI it can reach 41-85%. In the combined STBI group, mortality varies from 25 to 75% according to scientific and practical literature, while overall mortality in combined STBI averages 32%. [1,10,11]. Road traffic accidents (RTAs) play a leading role among the main causes of CSTBI: from 50 to 60% of all victims are participants in RTAs. Catatrauma also contributes to the increasing number of CSTBI victims. Catatrauma also contributes to the increasing number of CSTBI victims. They together account for 85-90% of all CSTBI victims. Train and household injuries account for 10-15%.Severe traumatic brain injury is a complex diagnosis that combines multiple pathologic conditions, including diffuse axonal injury, localized contusion foci, and hematomas located in the epi- and subdural spaces. Numerous scientific and practical studies have focused on identifying the causes of adverse outcomes and risk factors contributing to mortality [1,12,13]. After the initial injury caused by the traumatic agent, various pathophysiologic mechanisms come into play, leading to the development of secondary organic lesions. These secondary damaging factors aggravate the condition in more than half of STBI patients. Posttraumatic hypotension observed in the early posttraumatic period significantly worsens the prognosis of the disease, provoking the development of chronic intracranial hypertension. Chronic intracranial hypertension is an extremely dangerous and destructive factor, causing up to 70% of deaths and increasing disability [14]. In patients with STBI, mortality is dramatically increased with simultaneous hypoxia and hypercapnia. At the same time, pathogenetic factors are not simply added up (for example: hypoxia and hypotension), but mutually enhance each other due to the commonality of individual pathogenetic mechanisms. As a result, an aggravating effect is created, leading to an even more unfavorable development of each of the coexisting processes. As a consequence, the course of trauma in victims of this group is more severe, with a greater risk of infectious complications and characterized by high mortality, especially in patients with CSTBI, where the number of adverse and fatal outcomes can exceed 80% [2,3,7,15].Despite the successes achieved in recent decades, mortality in the group of STBI victims, according to various authors, remains high and reaches 70% [5,8,16]. Reducing mortality is a socially significant problem, as these are mostly patients of working age. In spite of this, we are still often unable to prevent fatal outcomes or serious lesions even in patients who are not initially considered severe. All this forces us to carefully analyze the reasons that led to the tragic outcome in order to prevent their repetition in the future. The aim of the study was to conduct a detailed analysis of the mechanisms leading to lethality in patients with severe traumatic brain injury, as well as to study the clinical epidemiology and identify the main causes of hospital mortality at different stages of experiencing severe traumatic brain injury.
2. Material and Methods
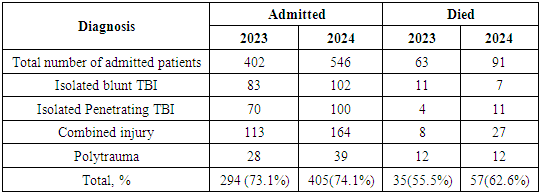
- We conducted a retrospective analysis of 92 case histories and the results of forensic medical examination of patients who died with severe traumatic brain injury and were treated in the neurosurgical ICU of the Republican Research Center of Emergency Medicine for the period from 2023 to 2024. The total number of admitted patients was 948: 699 (74%) of them were diagnosed with severe traumatic brain injury. The overall mortality differed by years and was 15.25% and 16.67%, respectively. Ninety-two patients out of 699 victims with traumatic brain injury died at various time after receiving the injury. Ninety-two patients out of 699 victims with traumatic brain injury died at various time after receiving the injury. There were 74 (80.4%) males and 26 (19.6%) females among the deceased. The mean age was 42.3±12.5 years. The age of the patients varied as follows: 14.9% of patients were from 17 to 20 years old, between 21 to 40 years old - 38.9%, between 41 to 50 years old - 35.9%, and over 50 years old there were 10.2%. TBI was associated with RTAs in 62.7% of the cases, 18.2% of the cases were related to catatrauma, 15.6% of the cases were household in nature, and 3.5% of the cases had an injury under unclear circumstances (Fig. 1).
 | Figure 1. Mechanisms leading to severe traumatic brain injury |
|
3. Results
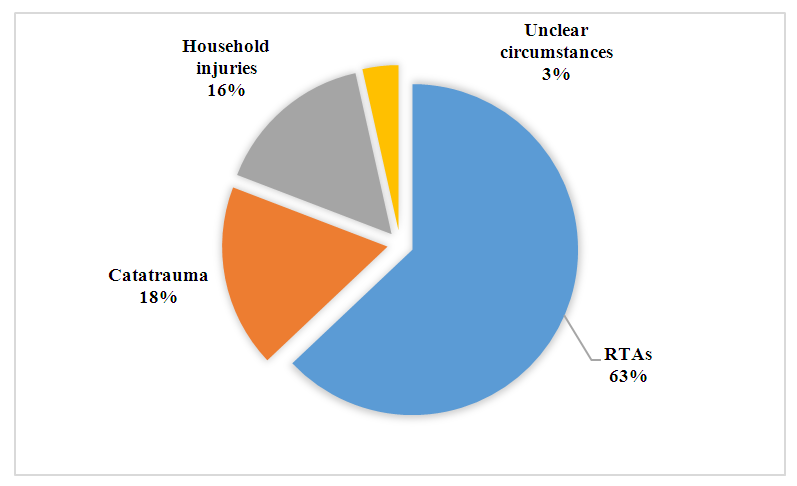
- The structure of STBI in the considered sample of patients was as follows: a combination of head and chest injuries was present in 49 (56.5%) patients, abdominal injury - in 28 (30.4%) cases, musculoskeletal system injury - in 48 (52.17%) ones, facial injury - in 32 (34.7%), combination with spinal injury was revealed in 22 (24%) patients. At the same time, it should be noted that one third of the victims had injuries of three or more anatomical areas of the body. The severity of injuries in patients was evaluated by ISS scale from 33 to 75 points (mean 54.4±12.8 points), and the level of consciousness was assessed by GCS (mean 5.2±2.4 points). In 6 patients compression of brain cisterns was detected at the initial CT scan, in 46 patients - displacement of medial structures more than 5 mm, intracerebral hematomas with the volume from 15 to 120 ml (evacuated surgically).Those who died in the first 24 hours after trauma were patients with very severe injuries and depression of consciousness level to deep coma. The severity of their injuries was estimated at 64.6±13.2 points on the ISS scale, and the level of consciousness according to the GCS was 4.2±1.6 points. No infectious complications were noted. It was noticed that as the severity of injuries decreased, the length of stay in the intensive care unit increased, but at the same time the incidence of infectious complications increased significantly. If by the 3rd day of patient's stay in the intensive care unit pneumonia was developed in 30% of them, then by the 10th day nosocomial pneumonia occurred in 100% of patients. Nineteen (20.6%) patients died in the first day, and 11 (57.9%) of those patients died within the first 7 hours of admission. There were 20 (21.7%) patients who died on days 1 to 3; 28 (30.4%) patients died on days 3 to 10 and 25 (27.2%) patients died on days more than 10. There was a statistically significant correlation between the severity of ISS scale injuries and the timing of death: the Spearman rank correlation coefficient was -0.637 (-0.718; -0.538), p < 0.0001 (Fig. 2).
 | Figure 2. Characteristics of injury severity, level of consciousness and frequency of nosocomial pneumonia development in patients depending on the time of death |
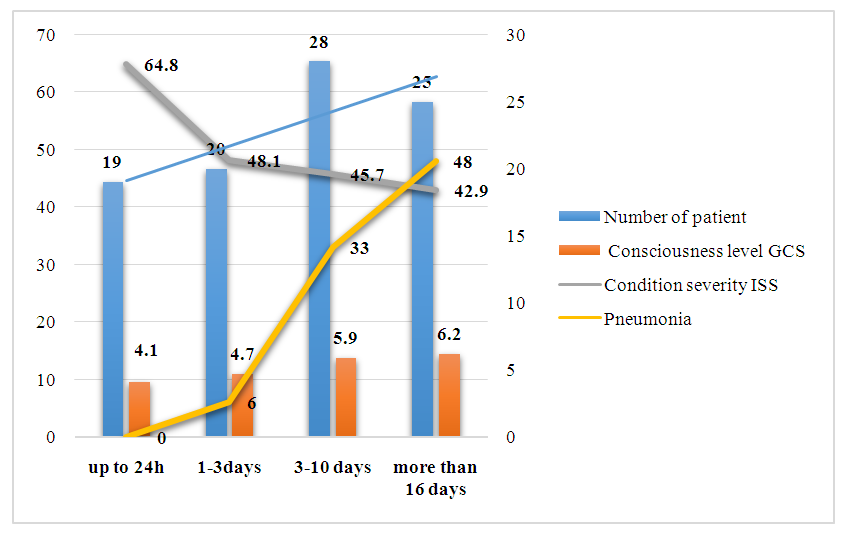
 | Figure 3. Distribution of patients depending on the main causes of death |
|
4. Discussion
- Analysis of the data showed that a greater number of victims die early from blood loss and shock (traumatic, hemorrhagic), but significantly more often fatal outcomes occure as a result of edema and dislocation of the brain, although at a later stage. According to the data, there is a statistically significant relationship between the timing of death depending on its main causes. According to the 5×4 contingency table, Chi-square is 164.007, the number of degrees of freedom is 12, and p <0.0001.Analyzing all groups of patients regardless of the time of admission, we can say that 41.2% of patients had brain edema and dislocation as the main cause of death, 25.3% had massive blood loss and shock (traumatic and/or hemorrhagic), and 15.9% had purulent-septic complications. Sepsis and septicemia were the main cause of death in 18.5% of the patients, and the mean time of the hospital stay was 28.4±16.5 days. Almost half of the patients had a combination of two or more complications. Thus, the retrospective detailed analysis of the case histories of STBI victims, as well as the features of their clinical course and lethality, including the main causes and terms of death, showed that the combination of head and musculoskeletal system trauma prevailed in the overall structure of STBI (79%). This was followed by patients with a combination of head and chest injury (72%); combination of STBI with abdominal injury was noted in 31% and combination with spinal injury was present in 17% of cases. The performed forensic medical studies revealed that the main causes of death in 25.3% of cases were massive blood loss and shock mainly in the first 24 hours, with up to 75% of them dying in the first 6 hours after the injury. It should be noted that two thirds of patients had a combination of injuries of four or more anatomical areas of the body. These victims were extremely severe, one third of whom were brought to the hospital in a state of clinical death, the rest were in agonal and extremely severe condition, and the severity of injuries according to ISS was more than 70 points.
5. Conclusions
- Edema and dislocation of the brain was the largest group of deceased patients, which accounted for 41.2% of the total. More than half of them died within 3 days from increasing edema, ischemia and dislocation of the brain, massive blood loss and shock; in the remaining victims, the severity of STBI was complicated by additional infectious complications. In these patients (12.9% of the total number), against the background of massive blood loss and prolonged shock, as well as prolonged mechanical ventilation, the severity of the injury was complicated by nosocomial pneumonia, which played a leading role in thanatogenesis.
Ethical Approval and Consent to Participate
- The Research Ethics Board of our institution does not require review or approval of case reports. Our research was carried out in accordance with the World Medical Association Code of Ethics (Declaration of Helsinki).
Conflict of Interests
- The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
ACKNOWLEDGEMENTS
- The authors express their gratitude to the management of the multidisciplinary clinic of Republican Research Centre of Emergency Medicine for the material provided for our study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML