-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 798-802
doi:10.5923/j.ajmms.20251503.64
Received: Mar. 1, 2025; Accepted: Mar. 19, 2025; Published: Mar. 22, 2025

The Importance of the Magnetic Resonance Imaging Method in the Diagnosis of Stenosis of the Lumbar Spine Canal
Abduvaxob Ablyazov1, Otabek Ablyazov2, Zarnigor Madumarova1, Shomahmud Turgunov1, Faryoz Kadirov1
1Department of Medical Radiology, Andijan State Medical Institute, Andijan, Uzbekistan
2Department of Medical Radiology, Center for the Development of Professional Qualifications of Medical Workers, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Lumbar spinal canal stenosis (LSS) is a prevalent condition characterized by the narrowing of the spinal canal, leading to nerve compression and neurological impairments. According to the World Health Organization, approximately 90% of the global population experiences lower back pain, with LSS being a major contributing factor. Accurate and early diagnosis is crucial for effective treatment, with magnetic resonance imaging (MRI) emerging as the gold standard due to its ability to visualize soft tissues and pathological changes. Objective: This study evaluates the role of MRI in diagnosing LSS by comparing MRI findings in healthy individuals and patients with degenerative and tumorous spinal conditions. Methods: A total of 55 participants (40 patients with LSS and 15 healthy controls) underwent MRI examination using the Magnetom Open Viva scanner. Key spinal canal parameters, including middle sagittal and frontal diameters at the bony and dural sac borders, were assessed. Statistical analysis was performed using SPSS software, with p-values <0.05 considered statistically significant. Results: The mid-sagittal diameter of the fifth lumbar vertebra was found to be 13.2% larger than that of the first lumbar vertebra in healthy individuals. Among patients with degenerative disease, the L4-L5 and L5-S1 levels exhibited the highest rates of stenosis. MRI effectively identified size reductions in pathological cases, confirming its diagnostic value. Conclusion: MRI is a reliable and non-invasive tool for assessing LSS severity, enabling accurate diagnosis and treatment planning. It offers superior soft tissue visualization compared to traditional radiological methods.
Keywords: Lumbar spine, MRI method, Degenerative and tumor lesions of the spinal canal, Central stenosis
Cite this paper: Abduvaxob Ablyazov, Otabek Ablyazov, Zarnigor Madumarova, Shomahmud Turgunov, Faryoz Kadirov, The Importance of the Magnetic Resonance Imaging Method in the Diagnosis of Stenosis of the Lumbar Spine Canal, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 798-802. doi: 10.5923/j.ajmms.20251503.64.
Article Outline
1. Introduction
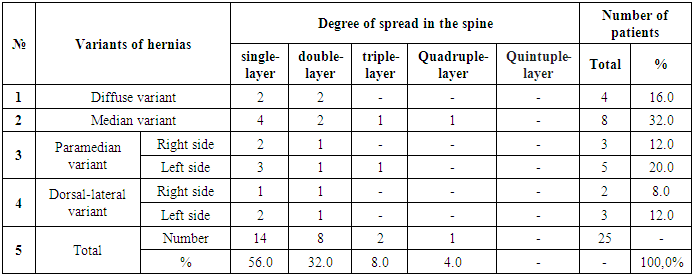
- Lumbar spinal canal stenosis (LSS) is a significant and prevalent condition affecting the spinal column, characterized by the narrowing of the spinal canal, which may result in nerve compression and various neurological symptoms. According to the World Health Organization (WHO), approximately 90% of the global population experiences lower back pain at least once in their lifetime, with LSS being one of the primary contributing factors. [1]The accurate and early diagnosis of LSS is crucial for effective patient management and treatment. Traditional radiological diagnostic methods such as X-ray and computed tomography (CT) scans have been used to assess spinal abnormalities. However, these techniques have limitations in evaluating soft tissue structures, which play a crucial role in LSS pathology. Magnetic resonance imaging (MRI) has emerged as the gold standard for diagnosing LSS due to its superior ability to visualize soft tissues, spinal cord structures, and pathological changes within the spinal canal. [2], [3]Anatomically, the lumbar spine consists of five vertebrae with intervertebral cartilage that contributes to spinal flexibility and shock absorption. The normal sagittal diameter of the lumbar spinal canal ranges from 20-25 mm, while the frontal diameter measures between 26-30 mm. [4] The spinal cord, housed within the spinal canal, extends approximately 44-45 cm in males and 41-42 cm in females, terminating at the conus medullaris and giving rise to the cauda equina. [5]Various factors contribute to the development of LSS, including degenerative changes, herniated discs, and malignant tumors. [6] Karahan and Kuvshinov (2002) classified lumbar stenosis into four main types: (a) central stenosis, (b) central stenosis with lateral stenosis, (c) unilateral lateral stenosis, and (d) mixed stenosis, with central stenosis accounting for up to 52% of cases. [7] A significant cause of stenosis is lumbar disc herniation, commonly occurring at the L4-L5 and L5-S1 levels. [8] Additionally, malignant tumors, either primary or metastatic, can lead to significant narrowing of the spinal canal. [9]This study aims to assess the role of MRI in diagnosing lumbar spinal canal stenosis by comparing MRI findings of healthy individuals with those of patients suffering from degenerative and tumorous spinal conditions. By examining key spinal canal parameters and their variations in pathological conditions, the research seeks to provide a comprehensive understanding of MRI’s effectiveness in identifying and grading the severity of LSS.
2. Materials and Methods
- A total of 55 participants were included in this study, comprising 40 patients with lumbar spinal canal stenosis and 15 healthy individuals as controls. All participants underwent MRI examination using the "Magnetom Open Viva" scanner, installed in the radiology department of the multidisciplinary clinic at the Andijan State Medical Institute. Among the patients, 25 were diagnosed with degenerative spinal changes, while 15 presented with malignant spinal tumors.Key MRI parameters assessed included:• Middle sagittal and frontal diameters of the lumbar spinal canal at the bony border.• Middle sagittal and frontal diameters at the dural sac border.• Vertical diameter measured in a straight projection.Statistical AnalysisStatistical analysis was performed using SPSS software (version 25.0, IBM Corp.). Continuous variables were expressed as means ± standard deviations (SD). The Kolmogorov-Smirnov test was used to assess data normality. Differences between the patient and control groups were analyzed using the independent t-test for normally distributed data and the Mann-Whitney U test for non-normally distributed data. A p-value of <0.05 was considered statistically significant.
3. Results and Discussion
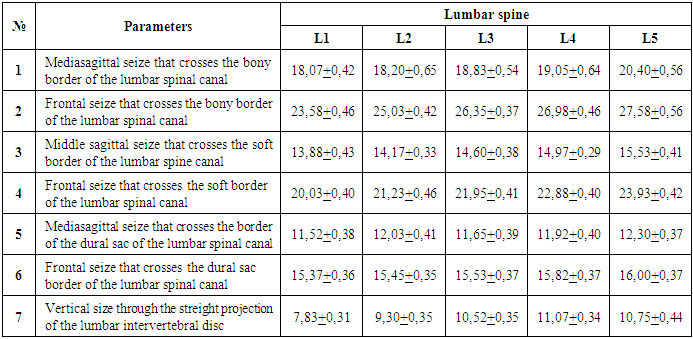
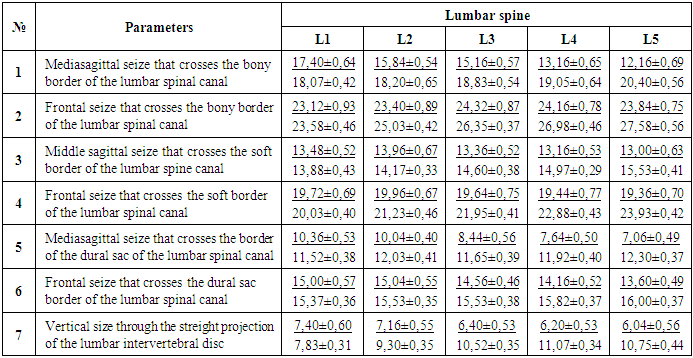
- Using MRI, we analyzed the lumbar spine canal dimensions in 15 healthy individuals to establish baseline parameters (Table 1). The mid-sagittal diameter of the bony border of the fifth lumbar vertebra was found to be 13.2% larger than that of the first lumbar vertebra, while the corresponding soft tissue measurements showed an 11.9% increase. The frontal diameter at the fifth lumbar level was also significantly wider, with bone and soft tissue measurements exceeding those at the first lumbar vertebra by 17.8% and 19.5%, respectively. Additionally, the vertical diameter at the L5-S1 intervertebral level was 27.3% greater than that measured at L1-L2. These findings provide a reference framework for assessing stenosis severity by comparing pathological deviations from these normal values.
|
|
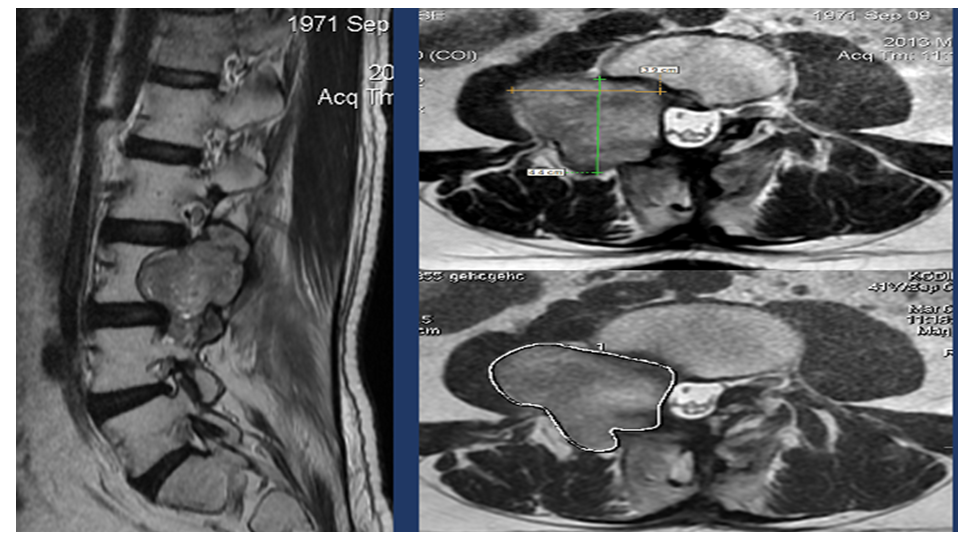 | Figure 1. Patient Kadyrov N. born in 1971. The malignant tumor is located mainly in the out of canal and partially penetrated into the canal. Stenosis in the subcompensatory phase occurred |
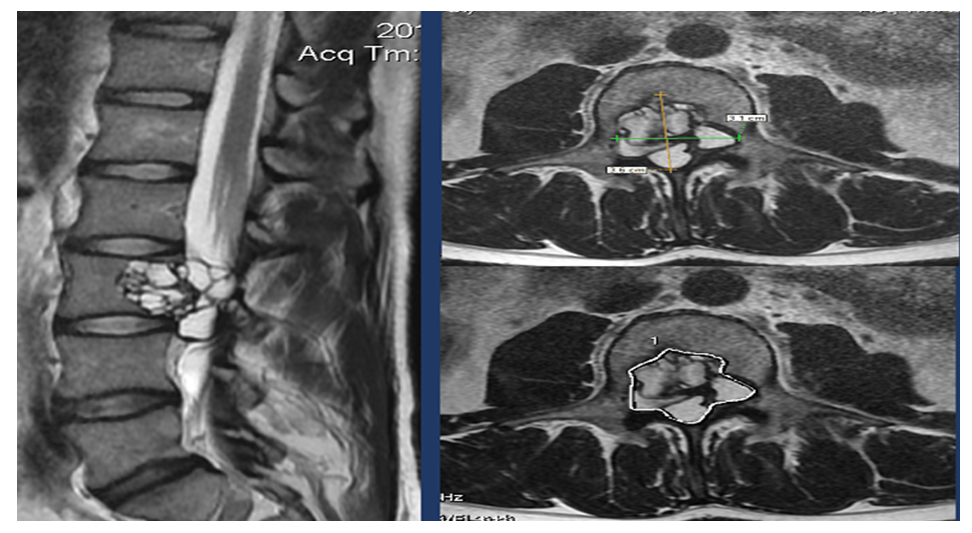 | Figure 2. Patient Novikov. born in 1982. Malignant tumor was located inside the canal, the canal was divided into two parts (blocks). Decompensated stenosis |
4. Conclusions
- The conclusion is that stenosis of the lumbar spine canal occurs as a result of severe degenerative trauma of the spine, in this disease the canal narrows and the spinal cord is pinched. With the help of the MRI method, it is possible to study at a high level the normal and pathological condition of the lumbar spine canal. All pathalogies that cause stenosis of the lumbar spine canal can be detected by the MRI method accurately and without harm to the patient.
ACKNOWLEDGEMENTS
- This study was conducted without any external funding.
Conflicts Interest
- The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
| [1] | World Health Organization. Low back pain: A major global challenge. WHO Bulletin. 2020; 98(3): 120-126. |
| [2] | Modic MT, Ross JS. Lumbar degenerative disc disease. Radiology. 2007; 245(1): 43-61. |
| [3] | Saito J, Ohtori S, Kishida S, et al. Difficulty of diagnosing the origin of lower leg pain in patients with both lumbar spinal stenosis and hip joint osteoarthritis. Spine. 2012; 37(7): 2089-2093. |
| [4] | Gelli RL, Raiser M, et al. Emergency orthopedics: Spine. Moscow: Medicine; 2003. |
| [5] | Zinyakov NT, Zinyakov NN. On the classification and terminology of herniated discs. Manual Therapy. 2007; (3): 22-29. |
| [6] | Saidov KK. Diagnosis of spinal cord tumors in elderly and senile patients. Neurology. Tashkent; 2006: 12-14. |
| [7] | Karahan V, Kuvshinov K. Spinal canal stenosis in the lumbar region: Surgical treatment. Doctor. Moscow. 2002; (4): 25-27. |
| [8] | Conn A, Buenaventura RM, Datta S, et al. Systematic review of caudal epidural injections in the management of chronic low back pain. Pain Physician. 2009; 12: 109-135. |
| [9] | Modic MT, Ross JS. Lumbar degenerative disc disease. Radiology. 2007; 245(1): 43-61. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML