-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 793-797
doi:10.5923/j.ajmms.20251503.63
Received: Feb. 27, 2025; Accepted: Mar. 17, 2025; Published: Mar. 22, 2025

Evaluation of the Quality of Life in Patients with Endocrine Ophthalmopathy
Sarvarkhon Yuldashov1, Erkin Bilalov2, Sayyora Akhmedova3, Akhmadjon Nozimov4
1PhD Student, Department of Human Anatomy, Operative Surgery and Topographic Anatomy, Tashkent Medical Academy, Tashkent, Uzbekistan
2Professor, Head of the Department of Ophthalmology, Tashkent Medical Academy, Tashkent, Uzbekistan
3Professor, Department of Human Anatomy, Operative Surgery and Topographic Anatomy, Tashkent Medical Academy, Tashkent, Uzbekistan
4PhD, Republican Specialized Scientific and Practical Medical Center of Eye Microsurgery, Tashkent, Uzbekistan
Correspondence to: Sarvarkhon Yuldashov, PhD Student, Department of Human Anatomy, Operative Surgery and Topographic Anatomy, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Relevance: Endocrine ophthalmopathy, commonly known as thyroid or Graves' ophthalmopathy, is an autoimmune disorder stemming from thyroid dysfunction. This chronic and progressive condition results in inflammation of the orbital soft tissues, thickening of the extraocular muscles, and the abnormal bulging of the eyes, leading to impaired visual function. Understanding the factors that impact and evaluate the quality of life for patients with this condition is essential. Purpose of the study: The primary aim of this study is to explore the clinical significance of quality of life in individuals suffering from endocrine ophthalmopathy through a specialized questionnaire. Materials and methods: We conducted a comprehensive study involving 72 patients (144 eyes), which included 54 women and 18 men, all diagnosed with endocrine ophthalmopathy. We employed an enhanced version of the Graves' ophthalmopathy quality of life (GO-QOL) survey, specifically developed and adapted to our local context. Results and conclusion: Our findings indicate that patients with severe cases of endocrine ophthalmopathy experience considerable visual impairment, which significantly detracts from their quality of life. The questionnaire not only elucidates the profound effects of this condition on patients' well-being but also serves as a vital measure for assessing the effectiveness of treatment interventions.
Keywords: Endocrine ophthalmopathy, Quality of life, Questionnaire, Disability assessment, Rehabilitation
Cite this paper: Sarvarkhon Yuldashov, Erkin Bilalov, Sayyora Akhmedova, Akhmadjon Nozimov, Evaluation of the Quality of Life in Patients with Endocrine Ophthalmopathy, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 793-797. doi: 10.5923/j.ajmms.20251503.63.
Article Outline
1. Introduction
- Endocrine ophthalmopathy (EO), often referred to as thyroid ophthalmopathy or Graves' ophthalmopathy, is a serious autoimmune disease linked to thyroid dysfunction. This chronic and progressive condition is marked by inflammation of the orbit's soft tissues, thickening of the extraocular muscles (EOM), and the alarming protrusion of the eyeball from the orbital cavity, known as bilateral thyrotoxic exophthalmos. Additionally, it poses risks to vision [1,2,3]. Recent research highlights a troubling trend: the incidence of EO is on the rise, particularly among young adults of working age and those in their reproductive years. This surge can be attributed to a complex interplay of genetic, anatomical, and environmental factors. While many studies have delved into the clinical diagnostic features of EO, there remains a critical gap in understanding how this condition affects patients' quality of life [4,5]. Alarmingly, some research indicates that individuals with EOP experience more significant health challenges and lower quality of life compared to those with other chronic illnesses such as diabetes or coronary heart disease. This situation can act as a substantial psychological stressor, adversely impacting the well-being of patients [6,7]. Moreover, the escalating prevalence of endocrine ophthalmopathy within the adult population is not merely a health concern; it has profound social implications. The potential for partial or complete loss of working capacity due to EO is a matter that demands urgent attention, as it affects not just individuals but also the broader community. Addressing this rising issue should be a priority for healthcare providers and policymakers alike [8,9,10].
2. Research Purpose
- This study aims to assess the clinical significance of the quality of life (QOL) in patients with endocrine ophthalmopathy through a specialized questionnaire administered in the Fergana region.
3. Material and Methods
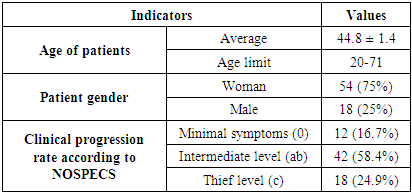
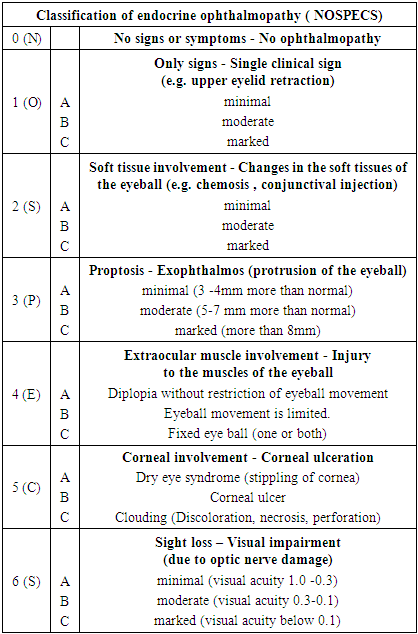
- The research involved 72 patients (n=144 eyes) diagnosed with endocrine ophthalmopathy at the Fergana branch of the Republican Specialized Scientific and Practical Medical Center of Endocrinology, named after Academician Y.Y. Turaqulov. All patients had both eyes affected by EO. The study included 54 women and 18 men, aged between 20 and 71 years, with an average age of 44.8 ± 1.4 years (Table 2) study. The average age of the patients was 44.8 ± 1.4 years (Table 1).
|
|
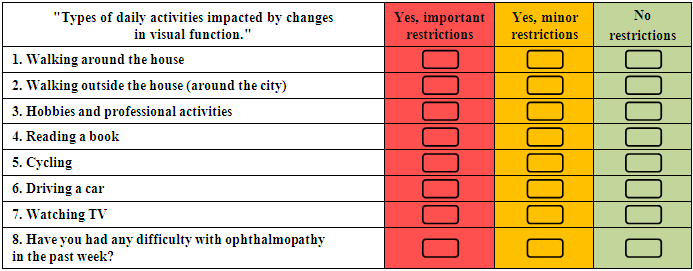
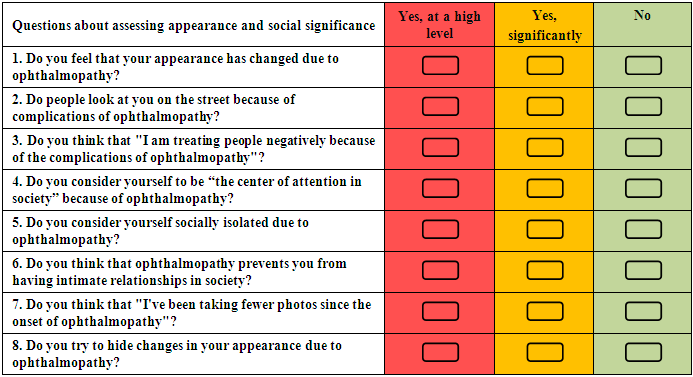
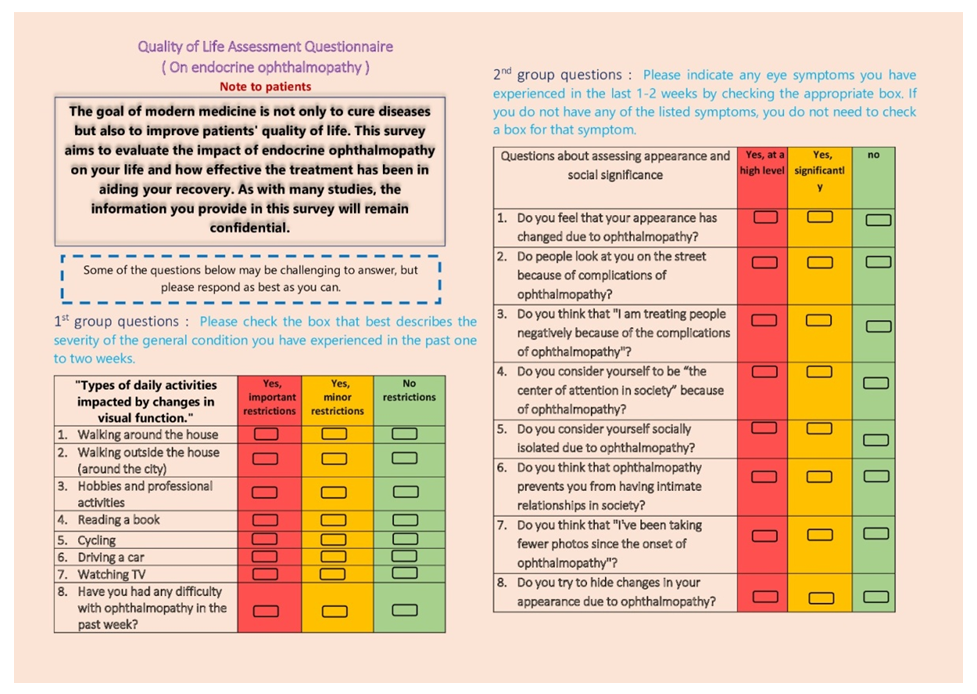 | Figure 1. Quality of life assessment questionnaire for Graves' ophthalmopathy |
4. Result and Discussion
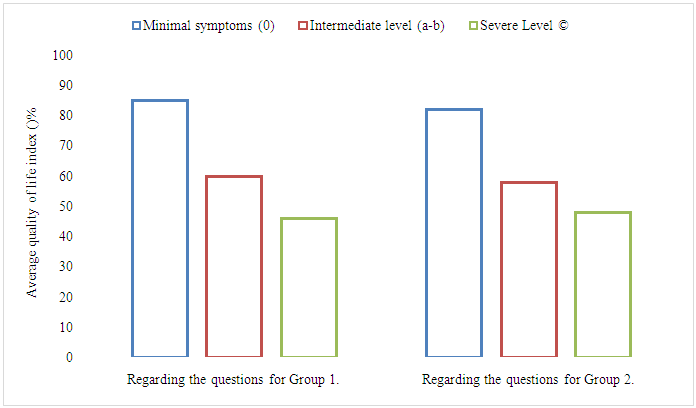
- The questionnaires were distributed to all 72 patients, of whom 68 (94.5%) completed the questionnaires and 4 (5.5%) patients did not want to participate in the survey. The time allotted for completing the questionnaire was 8 minutes and the process was carried out in a simple format, without special training. The questionnaire is designed to assess the impact of visual impairment and changes in the patient's appearance on the background of EOP, as well as the patient's emotional well-being, changes in social activities due to the disease are the subjective component of the questionnaire. In this case, a higher score on the scale indicates a higher level of quality of life. Changes in visual function in severe disease had a greater impact on the patient's quality of life, including daily activities (p=0.0018) and appearance and social significance (p=0.013), compared to patients with minimal disease (Table 3).
|
|
|
5. Conclusions
- The questionnaire used in the clinical study helps to better understand the impact of endocrine ophthalmopathy on the quality of life of patients and is an adequate criterion for assessing the effectiveness of treatment. Also, this type of questionnaire can be recommended for widespread use in clinical practice to improve the management of endocrine ophthalmopathy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML