-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 772-775
doi:10.5923/j.ajmms.20251503.59
Received: Feb. 26, 2025; Accepted: Mar. 15, 2025; Published: Mar. 20, 2025

Clinical and Diagnostic Significance of Inflammatory Biomarkers (IL-6, IL-1Β, IL-10, CRP) and Vitamin D Levels in Chronic Headaches
Dilafruz Bahodirovna Akhmedova
Associate professor, Department of Neurology, Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Dilafruz Bahodirovna Akhmedova, Associate professor, Department of Neurology, Bukhara State Medical Institute, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study aimed to investigate the levels of inflammatory biomarkers - IL-6, IL-1β, IL-10 and C-reactive protein (CRP) in chronic headaches and their clinical significance. Within the framework of the study, patients diagnosed with migraine with and without aura, chronic tension-type headache (CTHT) and migraine were subjected to immunological analysis. The concentrations of biomarkers were measured during the headache attack and in the non-attack period, and the dynamics of their changes were assessed. According to the results, the levels of IL-6, IL-1β and CRP significantly increased during the migraine attack (p<0.001), while in the non-attack period these indicators decreased (p<0.001). It was also noted that the level of the immunoregulator IL-10 was highest in the migraine with aura group, which reflects the activity of mechanisms modulating inflammatory processes. Inflammatory markers were relatively low in the TBI and cluster headache groups, which indicates that inflammatory processes play a secondary role in the pathogenesis of these headache types. It was also found that the level of Vitamin D did not differ significantly by headache type, which indicates that the pathogenetic significance of this vitamin in chronic headaches may be limited. The results obtained confirm the possible role of inflammatory markers in migraine attacks and indicate the need for additional studies to assess the effectiveness of anti-inflammatory therapy in migraine pathogenesis.
Keywords: Chronic headache, Migraine, Chronic tension-type headache, Interleukins, Vitamin D, Immunomodulatory assay
Cite this paper: Dilafruz Bahodirovna Akhmedova, Clinical and Diagnostic Significance of Inflammatory Biomarkers (IL-6, IL-1Β, IL-10, CRP) and Vitamin D Levels in Chronic Headaches, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 772-775. doi: 10.5923/j.ajmms.20251503.59.
Article Outline
1. Introduction
- Aydin et al. (2015) investigated plasma cytokine levels in migraine patients both during attacks and in attack-free periods. The study found that levels of pro-inflammatory cytokines, including TNF-α and IL-6, were significantly higher in migraine patients compared to healthy controls. Additionally, IL-10 levels were elevated during migraine attacks but lower during attack-free periods. These findings suggest that neurogenic inflammation, mediated by cytokines, plays a crucial role in the pathogenesis of migraines [1,9,12,13]. Bo et al. (2009) examined cerebrospinal fluid (CSF) cytokine levels in patients with migraine, tension-type headache (TTH), and cervicogenic headache (CH) compared to healthy individuals. The study found significant differences in the levels of IL-1 receptor antagonist (IL-1ra), transforming growth factor-beta 1 (TGF-β1), and monocyte chemoattractant protein-1 (MCP-1) between headache patients and controls. These findings suggest that cytokine-related neuroinflammation may play a role in the pathophysiology of different headache disorders, with variations in inflammatory responses among migraine, TTH, and CH patients [2]. Djalali et al. (2023) conducted a randomized, double-blind, placebo-controlled trial to investigate the effects of omega-3 fatty acid supplementation on inflammatory biomarkers in migraine patients. The study found that omega-3 supplementation significantly increased the levels of the anti-inflammatory cytokine IL-4 while reducing the levels of the pro-inflammatory cytokine IFN-γ. However, no significant changes were observed in TGF-β and IL-17 levels. These findings suggest that omega-3 fatty acids may have a beneficial impact on inflammation-related immune responses in migraine patients, potentially contributing to migraine management [3]. Hai (2010) investigated the effects of an NF-κB inhibitor on pro-inflammatory cytokine levels (TNF-α and IL-17) in a monocyte cell line cultured with serum from migraine patients. The study found that migraine patient serum significantly increased TNF-α and IL-17 levels in monocytes compared to the control group. However, treatment with the NF-κB inhibitor BAY11-7082 reduced TNF-α levels to near-normal levels, while IL-17 levels showed a partial reduction. These findings suggest that NF-κB activation may play a role in migraine-related neuroinflammation and that targeting NF-κB could be a potential therapeutic approach for migraine management [4,14,15]. Ishizaki et al. (2005) examined plasma levels of transforming growth factor-β1 (TGF-β1) in migraine patients during headache-free periods. The study found that migraine patients had significantly higher levels of TGF-β1 compared to healthy controls. Since TGF-β1 is a multifunctional cytokine involved in inflammatory and immune responses, its elevated levels suggest a potential role in migraine pathophysiology.These findings support the hypothesis that neurogenic inflammation contributes to migraine development, highlighting TGF-β1 as a possible biomarker or therapeutic target [5]. Javanmard et al. (2019) conducted a double-blind, randomized clinical trial to evaluate the effect of enalapril, an angiotensin-converting enzyme inhibitor (ACEI), on pro-inflammatory cytokines in migraine patients. The study found that enalapril significantly reduced serum levels of tumor necrosis factor-alpha (TNF-α) after two months of treatment, while there was no significant change in calcitonin gene-related peptide (CGRP) levels. These results suggest that enalapril may have an anti-inflammatory effect in migraine patients by lowering TNF-α levels, supporting its potential role in migraine management through inflammation modulation [6,10,11]. Khaiboullina et al. (2017) investigated cytokine changes and cerebellar atrophy in a Russian family with familial hemiplegic migraine type 1 (FHM1) caused by the CACNA1A R583Q mutation. The study found that patients with the mutation had significantly elevated levels of pro-inflammatory cytokines IL-6 and IL-18 compared to non-mutation carriers, indicating a strong inflammatory component in FHM1. Additionally, MRI scans revealed cerebellar atrophy in mutation carriers, suggesting a link between neuroinflammation and structural brain changes in migraine. These findings highlight the role of cytokine-mediated neuroinflammation in genetic forms of migraine and its potential impact on brain structure [7]. Lukács et al. (2017) reviewed the role of neurogenic inflammation in migraine pathophysiology and its implications for drug development. The study highlights the trigeminovascular system as a key player in migraine, where the release of pro-inflammatory neuropeptides such as calcitonin gene-related peptide (CGRP), substance P (SP), and vasoactive intestinal peptide (VIP) contributes to pain and vascular dysfunction. The review discusses emerging therapeutic targets, including monoclonal antibodies against CGRP and CGRP receptors, which have shown promising results in clinical trials. Additionally, potential future treatments targeting pituitary adenylate cyclase-activating polypeptide (PACAP) and kynurenic acid (KYNA) analogs are explored.These findings emphasize the importance of inflammation in migraine and the need for novel pharmacological approaches [8]. While standard therapeutic approaches, including triptans and prophylactic treatments, are effective for many patients, they do not provide consistent benefits in all cases. Therefore, a deeper understanding of inflammatory processes associated with migraine and other chronic headaches, identifying relevant biomarkers, and developing new therapeutic strategies based on these findings are crucial.
2. Purpose of the Research
- This study aims to analyze the dynamics of inflammatory biomarkers across different headache types and determine their pathogenetic role. The results may contribute to improving treatment strategies for chronic headaches, evaluating the potential of anti-inflammatory therapies, and developing novel approaches to migraine prevention. Given its implications for both neurology and immunology, this research holds significant scientific and clinical relevance in modern medicine.The purpose of this study is to investigate the dynamics of inflammatory biomarkers in different types of chronic headaches, including interleukin-6 (IL-6), interleukin-1β (IL-1β), interleukin-10 (IL-10), and C-reactive protein (CRP), and to determine their role in the pathogenesis and attack mechanisms of headaches. Additionally, the study seeks to assess the relationship between vitamin D levels and headaches.This research will examine the impact of inflammatory processes on migraine, chronic tension-type headache, and medication-overuse headache (MOH). Changes in biomarker levels during headache attacks and interictal periods will be analyzed to evaluate the potential of anti-inflammatory therapies in chronic headaches. The findings will provide a scientific basis for developing new treatment approaches to enhance therapeutic efficacy and improve headache management.
3. Materials and Methods
- This study included 315 patients diagnosed with chronic headache disorders, who were classified into four clinical groups based on the International Classification of Headache Disorders (ICHD-3):Ø Migraine with aura – 76 patientsØ Migraine without aura – 75 patientsØ Chronic tension-type headache (CTTH) – 117 patientsØ Medication-overuse headache (MOH) – 47 patientsAll patients underwent a comprehensive clinical and neurological examination. Headache characteristics, attack duration and intensity were assessed. Pain intensity was evaluated using the Visual Analog Scale (VAS), while the impact on quality of life was measured using the SF-36 and CPAQ-R questionnaires.For immunological analysis, venous blood samples were collected both during headache attacks and in interictal periods. The levels of inflammatory biomarkers – interleukin-6 (IL-6), interleukin-1β (IL-1β), interleukin-10 (IL-10), and C-reactive protein (CRP) – were determined using the enzyme-linked immunosorbent assay (ELISA). Additionally, vitamin D levels were analyzed in all patients.Statistical analysis was performed using SPSS software. Mean values (M±m) were calculated, and group differences were assessed using the Student's t-test and the Mann-Whitney U-test. Correlations between immunological markers and headache parameters were analyzed using Pearson and Spearman correlation coefficients. The association between inflammatory biomarkers and headache types was evaluated using the Chi-square test (χ²).The primary objective of the study was to determine the role of inflammatory biomarkers in different headache types and assess the potential application of immunological changes in treatment strategies.
4. Results and Discussion
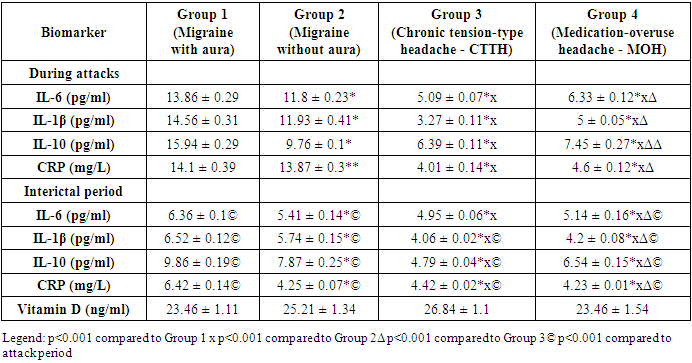
- The study evaluated the changes in inflammatory biomarkers—interleukin-6 (IL-6), interleukin-1β (IL-1β), interleukin-10 (IL-10), and C-reactive protein (CRP)—in different types of chronic headaches and their role in pathogenesis. The results confirmed that inflammatory processes play a significant role in migraine and other chronic headaches.
|
5. Conclusions
- The obtained results confirm the relationship between migraine attacks and inflammatory processes. A significant increase in inflammatory biomarkers was observed in both migraine with aura and migraine without aura groups (p<0.001). The decline in these markers after headache attacks indicates that inflammation has a dynamic nature. In chronic tension-type headache (CTTH) and medication-overuse headache (MOH) groups, inflammatory processes were found to be less active.These findings suggest the need for further investigation into the use of anti-inflammatory therapy and immunomodulatory agents in migraine management. Additionally, broader studies should be conducted to refine therapeutic approaches targeting inflammation and to deepen our understanding of migraine pathophysiology.Significant increase in inflammatory biomarkers during migraine attacks – IL-6, IL-1β, and CRP levels were notably higher in migraine with aura compared to other headache types (χ²=45.547; p=0.000). This confirms the strong link between inflammation and migraine attacks.Reduction of inflammatory markers in the interictal period – The decline in inflammatory indicators after an attack confirms the dynamic nature of inflammation (χ²=30.154; p=0.000). Additionally, lower levels of inflammatory mediators in CTTH and MOH groups suggest that these headache types are not directly associated with inflammation-driven mechanisms.No significant difference in vitamin D levels across headache types – Vitamin D levels did not show a statistically significant correlation with headache pathogenesis (χ²=2.683; p=0.847), suggesting that its role in migraine pathophysiology is limited.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML