Sh. A. Boymuradov, Sh. Kh. Bakieva, B. I. Karimberdiev, J. A. Djuraev
Tashkent Medical Academy, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
This article presents the results of comprehensive treatment for patients with combined injuries of the nose and paranasal sinuses. Combined craniocerebral injuries vary. First aid is provided first, i.e., bleeding from wounds is stopped, the wound is firstly surgically treated and sutured. Simultaneous symptomatic treatment is performed. Respiration, blood pressure, heart and brain activity will be restored. If there is a hematoma of the brain, a craniotomy is first performed to prevent complications, bleeding is stopped, and only then is planned treatment performed. In modern cranial-maxillary surgery, the principles of minimal dissection of bone fragments using small incisions have been replaced by the principles of reconstructive surgery, which involve separating all fracture planes, open repositioning, and rigid internal fixation. Lost bone fragments are often replaced with autografts. The best functional and cosmetic results can be achieved in the acute phase of the injury, as improper healing of the fracture can lead to difficult-to-repair functional, cosmetic defects and inflammatory complications. Using these principles, it is possible to reduce the number of later manifestations of aesthetic and functional consequences of facial trauma.
Keywords:
Paranasal sinuses, Trauma of paranasal sinuses, Mucociliary transport
Cite this paper: Sh. A. Boymuradov, Sh. Kh. Bakieva, B. I. Karimberdiev, J. A. Djuraev, Treatment Results of Various Trauma of Frontal Sinus, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 758-764. doi: 10.5923/j.ajmms.20251503.56.
1. Introduction
The treatment of paranasal sinus injuries in combined injuries is a subject of great debate. There is no algorithm for managing patients with acute kidney injury, therefore there are many questions regarding their conservative treatment, as well as the choice of the optimal surgical approach, the relevance and prevalence of surgical intervention. In addition, various specialists are involved, such as maxillofacial surgeons, neurosurgeons, plastic surgeons and otolaryngologists, and other specialists [4].In the post-traumatic period, specialists immediately provide first aid, there is no question of restoring the integrity of the cavity walls. This is due to the fact that in the acute period of HCC, fractures of the walls of the paranasal sinuses are not always diagnosed, only nasal bleeding is stopped [2].The primary principle for treating chronic kidney disease is the restoration of anatomical integrity of the bones. Combined craniocerebral injuries are diverse. First aid is provided first, i.e., bleeding from wounds is stopped, the wound is firstly surgically treated and sutured. Simultaneous symptomatic treatment is performed. Respiration, blood pressure, heart and brain function will be restored. If there is a hematoma of the brain, a craniotomy is first performed to prevent complications, bleeding is stopped, and only then is scheduled treatment performed. On the first day after the injury, repositioning of the cheekbones is performed, jaw repositioning is performed, and tires are placed, and the facial wound is sutured. Open osteosynthesis of jawbone fragments is sometimes performed [1-5]. In modern cranial-maxillary surgery, the principles of minimal dissection of bone fragments using small incisions have been replaced by the principles of reconstructive surgery, which involve separating all fracture planes, open repositioning, and rigid internal fixation. Lost bone fragments are often replaced with autografts. The best functional and cosmetic results can be achieved in the acute phase of the injury, as improper healing of the fracture can lead to difficult-to-repair functional, cosmetic defects and inflammatory complications. Using these principles, it is possible to reduce the number of aesthetic and functional consequences of facial trauma that manifest later [6-9].Although the treatment of these injuries is significantly more advanced than "tooth joint," combined injuries can leave significant cosmetic and functional defects. A good understanding of the mechanism of injury, the development of fixation methods, will significantly improve treatment outcomes, however, many controversial issues remain, such as: damage to the paranasal sinuses, especially the frontal sinuses, damage to the base of the skull, choice of treatment method, timing and extent of surgical treatment, the nature of complications, and methods of their treatment [10-14].The aim of the study is to improve the effectiveness of treatment outcomes for combined injuries of the paranasal sinuses in patients with combined injuries of the facial skeleton, skull, and other bones.
2. Results
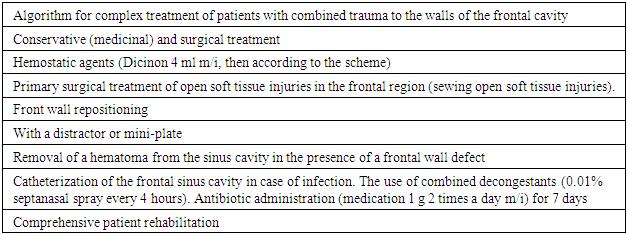
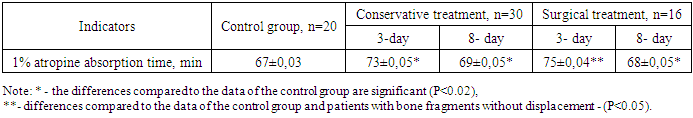
Comprehensive treatment of combined injuries of the lower extremities depended on many factors of combined trauma. These factors include the mechanism of injury, the severity of the patients' general condition, and the degree of brain damage. It is known that combined traumatic brain injury is accompanied by damage to the bones of the facial skeleton, the bones of the brain, internal organs, and the entire skeleton. In such patients, the clinic of brain damage often predominates, therefore, the consciousness of patients ranges from clear to deep coma. Treatment tactics include restoration of respiratory and cardiovascular system function. Therefore, resuscitation care is an important step.First aid includes stopping bleeding and symptomatic treatment. In addition to otolaryngologists, specialized care requires the involvement of a resuscitator, neurosurgeon, maxillofacial surgeon, ophthalmologist, traumatologist, and other specialists.Often, specialized otolaryngological care for this category of patients is delayed, i.e., after the general condition of the patients improves and the first aid is performed after the bleeding is stopped. Symptoms of sinusitis often appear in patients, therefore consultation with an otolaryngologist for this category of patients should be conducted within the first 24 hours after the injury.The combined injury of the paranasal sinuses is accompanied by a violation of the integrity of the paranasal sinuses mucosa, hemorrhages into the sinus cavity, and hematoma, with subsequent infection of the blood clots, leading to the development of sinusitis. To date, there is no algorithm for providing step-by-step care to patients with combined injuries of the lower extremities. The development of an algorithm for providing assistance to patients with combined injuries of the paranasal sinuses is crucial for the prevention of secondary sinusitis.Often, specialized otolaryngological care for this category of patients is delayed, i.e., after the general condition of the patients improves and the first aid is performed after the bleeding is stopped. Symptoms of sinusitis often appear in patients, therefore consultation with an otolaryngologist for this category of patients should be conducted within the first 24 hours after the injury.The combined injury of the paranasal sinuses is accompanied by a violation of the integrity of the paranasal sinuses mucosa, hemorrhages into the sinus cavity, and hematoma, with subsequent infection of the blood clots, leading to the development of sinusitis. To date, there is no algorithm for providing step-by-step care to patients with combined injuries of the lower extremities. The development of an algorithm for providing assistance to patients with combined injuries of the paranasal sinuses is crucial for the prevention of secondary sinusitis.The symptoms of the combined wound of the peripheral nervous system manifested differently. All 100% (n=142) of patients reported headaches, general weakness, and pain in the facial region, 93% (n=132) of patients reported dizziness and nausea, 39.4% (n=56) reported nosebleeds due to fractures of the nasal bones, 26% (n=37) reported subcutaneous emphysema due to fractures of the nasopharyngeal-orbital complex, 22.5% (n=32) reported diplopia due to fractures of the walls of the orbital cavity and displacement of its fragments. The complex treatment included symptomatic, antibacterial, anti-inflammatory, desensitizing, and surgical treatment methods. Reposition of the nasal bones was performed on 39.4% (n=56) of the examined patients, who were repositioned within 3 days of admission to the hospital. In 11.3% (n=16) of patients, the anterior wall of the frontal sinus was repositioned using a titanium distractor proposed by Sh.A. Boymurodov (2014).Cheekbone repositioning was performed by maxillofacial surgeons in 2.8% (n=4), while nasopharyngeal-orbital complex repositioning was performed in 10.6% (n=15) of patients. In 15.5% (n=22) of patients, the lower orbital wall was reconstructed using a titanium implant, while in 9.8% (n=14) of patients, the lower orbital wall was repositioned by endothelium. Sinusotomy of the upper jaw was performed in 10.6% of patients (n=15) with the aim of removing the hematoma and repositioning the sinus walls. We have developed a mobile application for comprehensive treatment of combined facial bone injuries.Comprehensive treatment of patients with combined frontal wall trauma (n=46).Of the 46 patients, 58.6% (n=27) reported facial soft tissue involvement, with subcutaneous hematoma and soft tissue edema frequently observed, who were prescribed cold compresses, hemostatic, desensitizing, and anti-inflammatory therapy to prevent the development of hematomas during medical care. Open soft tissue injuries with bone fragment displacement were identified in 19.5% of patients (n=9). During hospitalization, these patients underwent primary surgical treatment of their wounds. To do this, the soft tissue wound was anesthetized with a 0.5% lidocaine solution, then cleaned of the dirty mass, foreign bodies were removed, after which the wound was cleaned with antiseptics, 3% hydrogen peroxide, 0.1% chlorhexidine, the soft tissues around the wound were rubbed with a betadine solution, in the final stage, the muscular-subcutaneous layer was sutured layer by layer with Vicryl No. 5, and the skin was sutured with a synthetic suture material - proline The wound was rearranged daily, the sutures were removed on days 7-8.Closed craniocerebral trauma was recorded in 95.6% (n=44), while open craniocerebral trauma was recorded in 4.4% (n=2). Brain concussion was observed in 38 patients, hematoma and stroke in 6 patients. Four of them were admitted unconscious. The remaining patients exhibited symptoms of concussion. All patients were admitted to the intensive care unit through the emergency department, where they received first aid, which included stopping bleeding, primary surgical treatment of the wound, restoration of respiratory and cardiovascular function.We have developed an algorithm for comprehensive treatment of combined trauma to the anterior wall of the frontal cavity (Table 1).Table 1. Algorithm for comprehensive treatment of combined frontal wall trauma
 |
| |
|
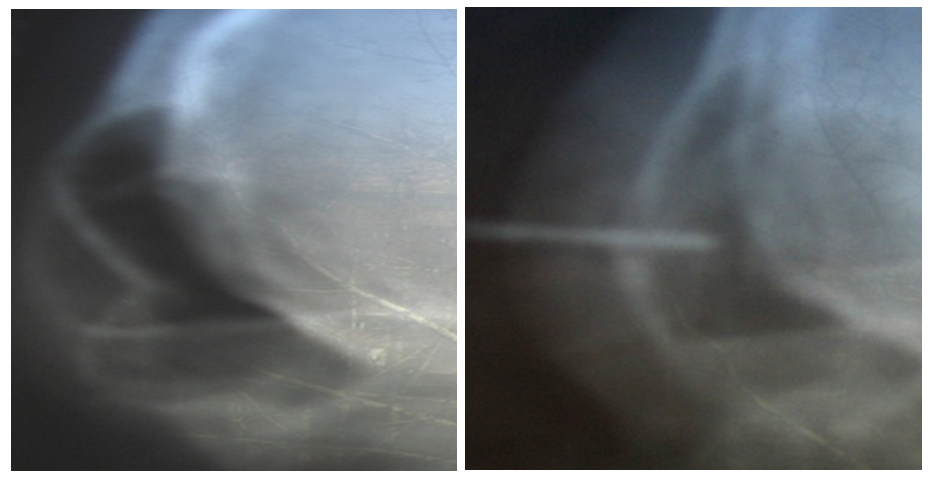
All 16 patients underwent bone fragment repositioning and osteosynthesis within 3 days. In 95.6% of patients (n=44), MSCT revealed the presence of blood in the sinuses, while only 1 patient showed the presence of serous fluid in the sinuses.Of the 16 operated patients, 12 underwent anterior wall repositioning using a distractor. The surgical procedure included the repositioning of bone fragments of the anterior wall of the frontal sinus using a titanium distractor, proposed by Sh.A. Boymurodov (2014). The operation process was as follows. Clinical example 1: Under general anesthesia, a horizontal incision was made along the arch of the eyebrow, followed by layer-by-layer separation of soft tissues, subcutaneous adipose tissue, muscles, and periosteum. After that, it was possible to access the fragments of the forehead, which were in a compressed state, using drill No. 1, a hole was opened, into which a distractor with spiral threads was installed (Fig. 1). | Figure 1. Titan distractor installation steps |
After the distractor was rotated and installed, the anterior wall was repositioned manually under visual observation, after which the soft tissue locusts were replaced and sutured layer by layer with Vicryl and Prolen No. 5. The distractor was screwed and removed on the 4th day after surgery, and sutures were removed on the 8th day, with all patients healing the wound with primary drawing (Fig. 2).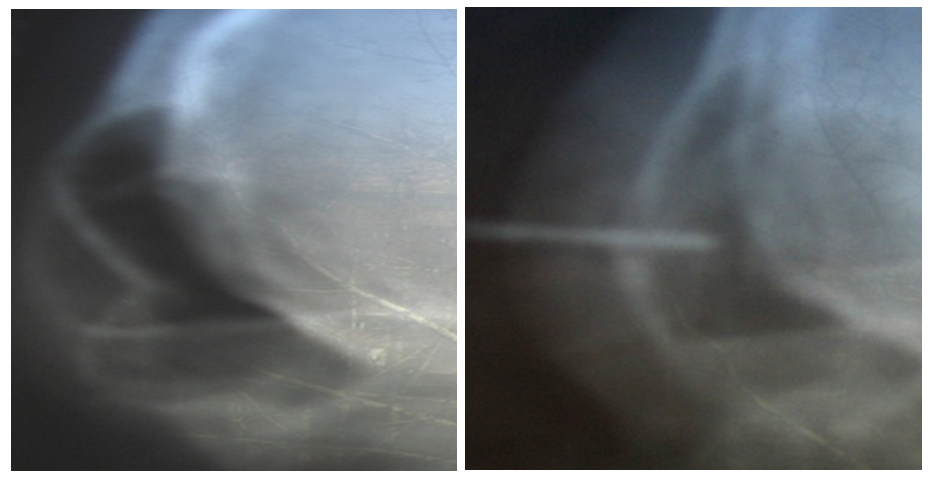 | Figure 2. X-ray image of the displacement of the bone fragment of the anterior wall of the frontal cavity and the implanted titanium distractor |
Four patients were diagnosed with fractures of the frontal bone, in which we restored the anterior wall using mini-plates. For this purpose, the introduction was made as described above, after which mini-plates were installed in the horizontal direction, secured with screws, bone fragments were installed on mini-plates with screws. After that, the wound was sutured. On the 8th day, the threads were removed.Clinical example 2. Patient X.1 was injured in a car accident. He was admitted to the emergency department of the multidisciplinary clinic of the Tashkent Medical Academy. She was diagnosed with a "complex injury: concussion, compression fracture of the frontal wall on the right." Following the clinical and laboratory examination, the patient underwent surgery, under general anesthesia, an incision was made along the arch of the eyebrows, soft tissues were incised, the periosteum was separated, and compression fragments of bone fragments of the anterior wall of the frontal cavity were found (Fig. 3). | Figure 3. Image of the patient with a compression fracture of the anterior wall of the frontal cavity |
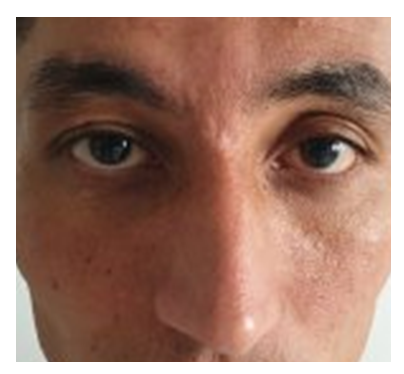
After that, using a screw mounted on a titanium mini-plate (Fig. 4), the place of the pressed slice was changed, and in the final stage, the wound was covered with soft tissue and an aseptic bandage was applied. The wound healed with the first drawing, the thread was removed on the 8th day. As can be seen from the patient's photo, there were no coarse scars after surgery (Fig. 5). | Figure 4. A photograph of the patient. A mini-plate was placed on the anterior wall of the frontal cavity and the wound was sutured |
 | Figure 5. A photograph of the patient after suture removal |
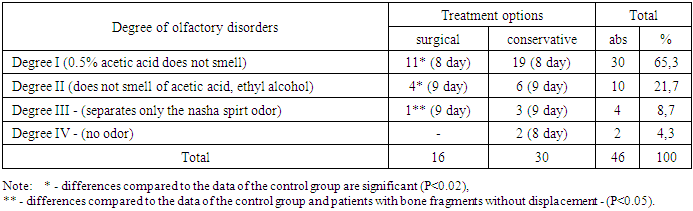
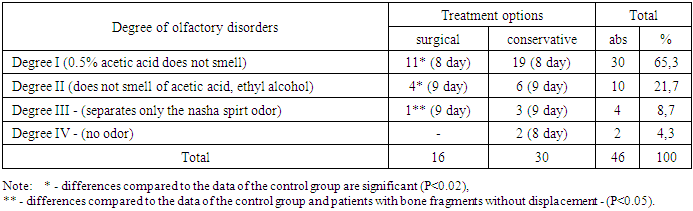
Fractures of the frontal walls without displacement of bone fragments were observed in 65.2% (n=30) of 46 patients with combined frontal wall trauma. All of them exhibited nasal bone fractures and underwent nasal bone repositioning. These patients received conservative treatment.Patients were treated conservatively according to the proposed algorithm.In the postoperative period, narrowing drugs, antibiotics, and anti-inflammatory drugs were prescribed to the nose.Olfactometric parameters were studied in the postoperative period. The study showed that hyposmia was observed in n=11 patients who underwent surgery and n=30 patients who received conservative treatment in the postoperative period. Mild hyposmia was observed in n=4 patients who underwent surgery and n=6 patients who received conservative treatment. A significant degree of hyposmia was observed in n=1 patients who underwent surgery and n=3 patients who received conservative treatment. Anosmia was not observed in the operated patients, but in n=2 patients who received conservative treatment (Table 2).Table 2. The olfactometric parameters of patients treated with anterior sinuses wall injuries were n=46 (100%)
 |
| |
|
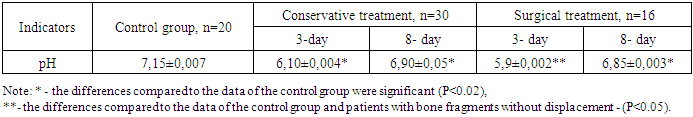
Table 3. Nasal secretion parameters (pH) in n=46 (100%) patients with frontal sinus wall damage on days 3 and 8
 |
| |
|
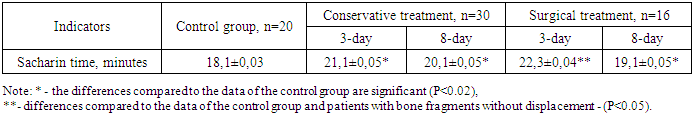
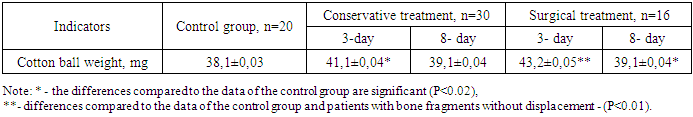
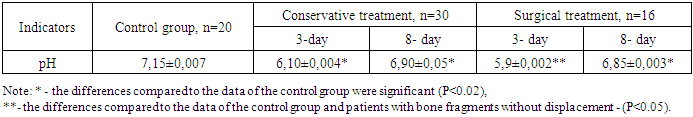
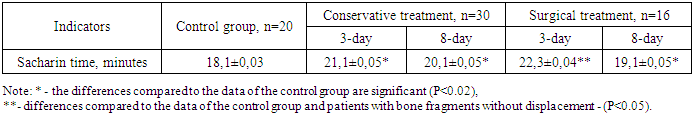
Analysis of the data showed that in operated patients, olfactory disturbances recovered in a short time (8 days), while in patients receiving conservative treatment, this indicator recovered after a long time (P<0.02).Odor disorders are associated with damage to the peripheral olfactory reflex, which are restored after treatment, while anosmia is associated with the central mechanism of damage, i.e., the frontal lobe of the brain.Results of the study of the hydrogen index (pH) of nasal secretion in this group of patients before and after treatment showed that in patients receiving conservative treatment n=30, a shift to an acidic environment was observed before treatment - 6.10±0.004 (P<0.02) and on the 8th day after treatment, this indicator was 6.90±0.05 compared to the control group (control group indicator - 7.15±0.007, n=20), the indicator of n=16 operated patients before treatment was 5.9±0.002 and after treatment - 6.85.Mucociliary clearance data showed that in patients n=30 who received conservative treatment on the 3rd day, saccharine time lasted longer than in patients in the control group (18.1±0.03) (21.1±0.05) (P<0.02), while on the 8th day this indicator decreased to 20.1±0.05; in patients n=16 who received surgical treatment, this time lasted longer than in the control group 22.3±0.04 (P<0.05), and on the 8th day after treatment, this indicator decreased to 19 (Table 4).Table 4. Mucociliary clearance indices on the 3rd and 8th days in 46 (100%) patients with anterior wall trauma, in minutes
 |
| |
|
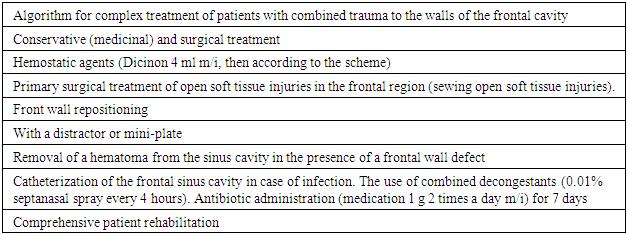
These disorders of mucociliary clearance were associated with damage and swelling of the nasal mucosa, which led to a slowing of mucosal movement. In patients receiving conservative treatment, this indicator decreased on the 8th day, while in patients receiving surgical treatment, this indicator approached the control group.A study of nasal mucosal absorption function showed that in patients receiving conservative treatment, it was longer than the control value on day 3, and closer to normal on day 8. On the 3rd day of surgical treatment, this indicator was 75±0.04 mg, and on the 8th day, this indicator was within the control range (P<0.05) (Table 5).Table 5. Indicators of nasal mucosal absorption function on days 3 and 8 in n=46 (100%) patients treated with anterior wall trauma, min
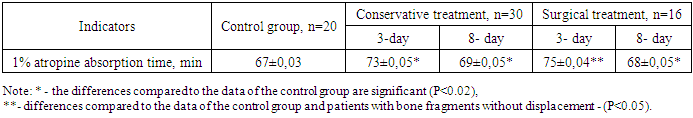 |
| |
|
Results of the study of nasal excretory function showed that in n=30 patients who received conservative treatment, the mass of the balloon on day 3 was 41.1±0.04 mg, meaning it was 3.1±0.04 mg heavier than the control weight (P<0.02), and on day 8 this indicator was closer to the norm 39.1±0.04 mg, while in n=16 patients who received surgical treatment, this indicator was 43.2±0.05 mg on day 3, meaning it was 5.1±0.04 mg heavier than the control (P<0.01).Table 6. Indicators of nasal septal function on days 3 and 8 in patients with anterior wall trauma n=46 (100%), in mg
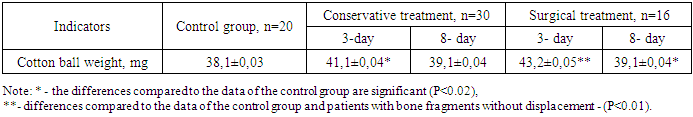 |
| |
|
3. Conclusions
Therefore, it can be concluded that according to the results of the conducted research, it has been established that damage to the frontal sinus is accompanied by a decrease in the volume of the frontal sinus, leading to impaired function. The upper wall is most often damaged (67%). Following complex treatment, the anatomical integrity of the walls and the function of the nasal mucosa are restored.
Limitations and Strengths of the Study
This study provides valuable insights into the treatment of combined trauma involving the frontal sinus, highlighting the importance of timely surgical intervention and comprehensive postoperative care. One of the strengths of this study is its detailed analysis of clinical cases and the use of innovative reconstructive techniques, such as the titanium distractor method, which enhances the accuracy and effectiveness of surgical repositioning. Additionally, the study contributes to the development of an algorithm for the treatment of combined trauma, which can improve clinical decision-making and patient outcomes.However, there are certain limitations to the study. The sample size, while representative, may not be large enough to generalize the findings to a broader population. Additionally, the study focuses on short-term treatment outcomes, and long-term follow-up data are limited. Future studies should consider larger, multi-center trials and extended follow-up periods to evaluate the long-term effectiveness of the proposed treatment methods.
Ethical Considerations
This study was conducted in accordance with the ethical guidelines and principles established by the Declaration of Helsinki. Ethical approval was obtained from the institutional ethics committee of the Tashkent Medical Academy. Written informed consent was obtained from all patients before their inclusion in the study. The anonymity and confidentiality of patient data were strictly maintained throughout the research process. No experimental procedures were performed outside standard clinical practice, and patients received appropriate medical care based on their individual conditions.
ACKNOWLEDGEMENTS
The authors would like to express their sincere gratitude to the medical staff and specialists at the Tashkent Medical Academy for their valuable contributions to the study. Special thanks to the maxillofacial surgeons, neurosurgeons, and otolaryngologists who participated in the clinical management of patients. We also acknowledge the support of the research team and institutional colleagues for their constructive feedback and assistance in data collection and analysis. Finally, we extend our appreciation to the patients who consented to participate in the study, contributing to advancements in the treatment of combined trauma of the frontal sinus.
References
| [1] | Agzamova S. Retrospective analysis of the condition of ophthalmological status in traumas of the scoop-orbital complex // Stomatology. - 2021. - T. 1. - No. 1 (82). - С. 89-92. |
| [2] | Boymuradov Sh. Innovative methods of treatment of combined injuries of the bones of the facial skeleton based on algorithmization of the doctor's activities // Journal of Problems of Biology and Medicine. - 2015. - No. 1 (82). - С. 29-33. |
| [3] | Dorovskyi G.N. Radiation diagnostics of polytrauma: dis. Moscow State Medical Dental Institute named after A.I. Evdokimov. Moscow. 2014, 2014. |
| [4] | Dorovskyi G. N. Comparative analysis of sensitivity and specificity of various methods of radiation diagnostics in polytrauma // Acta Biomedica Scientifica. - 2014. - No. 4 (98). - С. 24-28. |
| [5] | Ilyasov D.M. Treatment tactics for nasal cavity injuries in patients with severe combined head trauma: dis. - Ilyasov Denis Maratovich. 2013.-24c, 2013. |
| [6] | Maday D. Yu., Golovko K. P. Minimally invasive methods in the treatment of severe craniocerebral injuries // Health. Medical ecology. Science. - 2012. - T. 47. - No. 1-2. - С. 41-42. |
| [7] | Z.K. Norboyev et al. Algorithm for diagnosing traumatic injuries and post-traumatic complications in the area of the frontal sinus // Questions of Science and Education. - 2018. - No. 26 (38). - С. 72-74. |
| [8] | Pavlova O.Yu. et al. Radiation diagnosis of facial bone injuries // Russian electronic journal of radiation diagnostics. - 2014. - T. 4. - No. 3. - С. 39-45. |
| [9] | Popova I. E. et al. Modern aspects of diagnosing severe combined trauma using computed tomography // Vestnik meditsinskogo instituta "Reaviz": rehabilitation, doctor and health. - 2021. - No. 3 (51). - С. 28-37. |
| [10] | Saurasova N.A. et al. X-ray diagnostics of traumatic injuries to the maxillofacial region. - 2017. |
| [11] | Samykin A. S. Characteristics of treatment for traumas of the scoop-orbital complex // Universum: Medicine and Pharmacology. - 2014. - No. 3 (4). - С. 4. |
| [12] | Urgunaliyev B. K., Shaiahmetov D. B., Tsoy A. R. Modern approaches to the diagnosis of fractures of the bones of the facial skeleton // Russian dental journal. - 2018. - Т. 22. - No. 6. |
| [13] | Shedrenok V. V. et al. Clinical and radiological diagnostics of craniocerebral injuries in polytrauma // Vestnik xirurgii imeni AI Grekova. - 2012. - T. 171. - No. 2. - С. 41-44. |
| [14] | Yusupov Sh., Boymuradov Sh. Modern aspects of diagnosis and planning of surgical treatment of fractures of the maxillary-orbital complex // Journal of the doctor's announcer. - 2018. - T. 1. - No. 4. - P. 129-134. |





 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML