-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 744-748
doi:10.5923/j.ajmms.20251503.54
Received: Feb. 25, 2025; Accepted: Mar. 11, 2025; Published: Mar. 17, 2025

Clinical Significance of Duplex Scaning in the Diagnosis of Vertebrobasilar Insufficiency
Feruza Aripova1, Abdurasul Yulbarisov2, Alimjon Akhmatov1
1Republican Specialized Center of Surgical Angioneurology, Uzbekistan
2Tashkent Medical Academy, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Early diagnosis of chronic and acute cerebrovascular disorders remains a major challenge in modern medicine, as these conditions significantly impact patient outcomes and quality of life. Vertebrobasilar insufficiency (VBI), a common cerebrovascular disorder, is often difficult to diagnose due to its nonspecific symptoms. This study presents an analysis of data obtained through the duplex scanning method for diagnosing VBI. Duplex ultrasonography is a non-invasive, cost-effective, and highly informative diagnostic tool that allows for real-time visualization of blood flow in the vertebrobasilar system. A total of 117 patients with VBI were examined using this method to assess the severity of hemodynamic impairments and vascular abnormalities. The results demonstrate the effectiveness of duplex scanning in identifying stenotic changes, vascular occlusions, and blood flow disturbances, which are critical in the early detection of cerebrovascular pathology. The study highlights the importance of incorporating duplex ultrasonography into routine clinical practice for timely diagnosis and intervention. Early identification of VBI through advanced imaging techniques can significantly improve treatment strategies, reduce the risk of stroke, and enhance patient prognosis. Further research is needed to explore the integration of duplex scanning with other neuroimaging modalities to improve diagnostic accuracy and patient outcomes.
Keywords: Vertebrobasilar insufficiency syndrome, Ischemic stroke, Chronic cerebral ischemia, Duplex scaning of the vertebral arteries
Cite this paper: Feruza Aripova, Abdurasul Yulbarisov, Alimjon Akhmatov, Clinical Significance of Duplex Scaning in the Diagnosis of Vertebrobasilar Insufficiency, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 744-748. doi: 10.5923/j.ajmms.20251503.54.
Article Outline
1. Introduction
- Vertebrobasilar insufficiency (VBI) is a significant cerebrovascular disorder that can lead to transient ischemic attacks and, in severe cases, ischemic stroke. Its early diagnosis remains a crucial challenge in modern medicine due to the variability of symptoms and the complexity of cerebrovascular circulation. Duplex scanning is an effective, non-invasive imaging technique that allows for the assessment of vascular blood flow and potential abnormalities. This study aims to explore the clinical significance of duplex scanning in diagnosing VBI and to conduct a comparative analysis of its hemodynamic impact.
2. Materials and Methods
- This study was conducted at the Republican Specialized Center of Surgical Angioneurology. A total of 117 patients (100%) diagnosed with VBI were selected from December 2017 to 2025. As part of the diagnostic protocol, patients presenting with tinnitus underwent an audiogram to rule out other pathological conditions that could contribute to their symptoms.Both the observation group and the control group underwent duplex scanning to assess blood flow parameters in the internal carotid and vertebral arteries. The results were compared to determine the differences in cerebral hemodynamics. The study specifically examined blood flow velocity, vascular asymmetry, and stenotic changes in patients with VBI.
3. Objective
- The primary objective of this study is to facilitate the early diagnosis of vertebrobasilar insufficiency using duplex scanning and to conduct a comparative analysis of its impact on cerebral hemodynamics. By identifying variations in blood flow, this study aims to enhance the understanding of the vascular mechanisms underlying VBI and improve diagnostic accuracy.
4. Results
- The duplex scanning results of 117 hospitalized patients diagnosed with vertebrobasilar insufficiency revealed significant differences in blood flow velocity in the internal carotid and vertebral arteries in 80.5% (94/117) of cases. Furthermore, in 60.2% (28/70) of patients, blood flow velocity was found to vary depending on the diameter of the vertebral arteries, indicating asymmetry in vascular perfusion. These findings suggest that duplex scanning is a valuable tool in detecting hemodynamic disturbances associated with VBI. The results highlight the necessity of integrating duplex scanning into routine diagnostic procedures to improve early detection and optimize treatment strategies for patients at risk of cerebrovascular complications.Information Obtained from Changes in the Vertebral ArteriesThe results of Vs (systolic velocity), Vd (diastolic velocity), and Vm (mean velocity) of blood flow in the vertebral arteries were found to be lower in the observation group compared to the control group. In 22.6% (15/70) of cases in the observation group, where symptoms of vertebrobasilar insufficiency were predominant, pathological deformation of the internal carotid artery was observed. These pathological deformations, such as kinking and coiling, were found to have significant hemodynamic implications during duplex scanning.
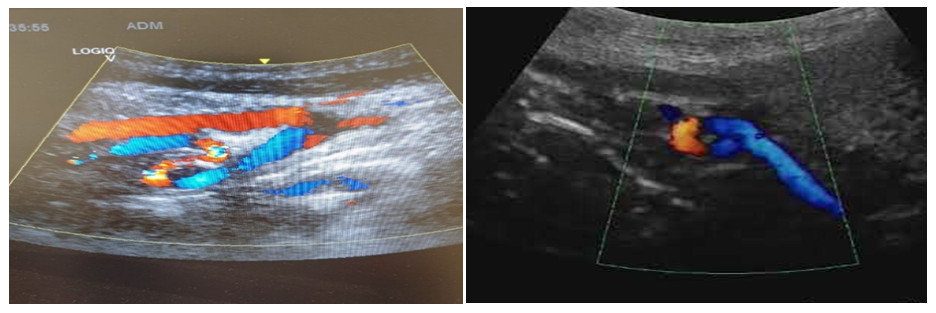 | Figure 1 |
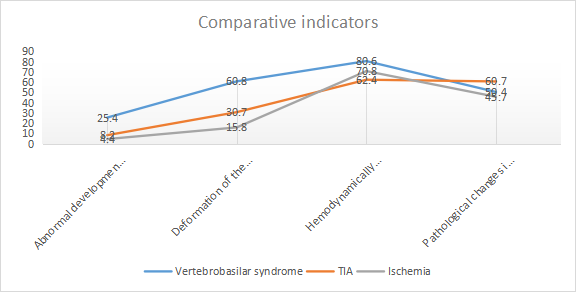 | Figure 2 |
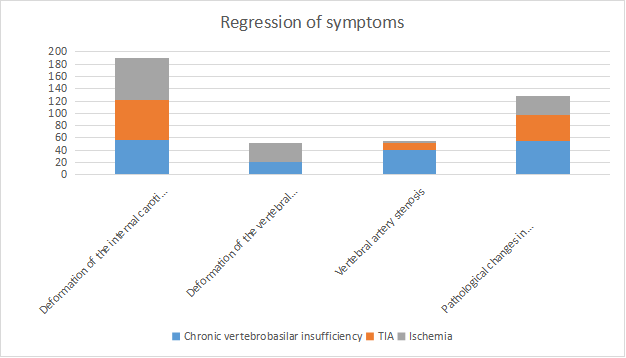 | Figure 3 |
5. Discussion
- The findings of this study emphasize the significant role of duplex scanning in diagnosing vertebrobasilar insufficiency (VBI) and its impact on cerebral hemodynamics. The results confirm that duplex ultrasonography is an effective, non-invasive method for detecting vascular abnormalities such as stenotic changes, vascular occlusions, and asymmetrical blood flow in patients with chronic cerebrovascular insufficiency. The study's outcomes provide valuable insights into the necessity of early diagnosis to reduce the risk of transient ischemic attacks (TIA) and ischemic stroke.One of the key findings of the study is the observed differences in blood flow velocities in the vertebral and internal carotid arteries among the observation and control groups. The lower systolic (Vs), diastolic (Vd), and mean (Vm) velocities in patients with VBI, compared to healthy individuals, highlight the hemodynamic disturbances associated with the condition. Additionally, the presence of pathological deformations such as kinking and coiling in 22.6% of cases further supports the hemodynamic significance of vascular anomalies detected through duplex scanning.Another crucial aspect explored in the study is the correlation between vertebral artery diameter and blood flow asymmetry, with 60.2% of cases showing variations in velocity based on vessel diameter. This finding suggests that anatomical and physiological factors contribute to hemodynamic instability in VBI, reinforcing the importance of vascular imaging in assessing disease severity. Moreover, the detection of ischemic changes in 4.4% of patients and TIA episodes in 8.2% suggests that early diagnosis through duplex scanning may facilitate timely interventions to prevent cerebrovascular complications.The study also highlights the role of functional and pharmacological tests, such as the De-Kleijn test with pyridamole, in assessing cerebral hemodynamic reserve. The ability to detect functional impairments in the Willis Circle and the tendency of intracranial arteries to spasm under dipyridamole administration underscores the need for a comprehensive diagnostic approach that integrates duplex scanning with transcranial Doppler ultrasound and neurophysiological assessments. The study's findings align with existing literature, reinforcing the importance of multimodal imaging techniques in diagnosing and managing VBI.Additionally, the analysis of symptom regression based on duplex scanning suggests that conservative and endovascular treatments may improve hemodynamic parameters in patients with vertebral artery stenosis. The observed regression of symptoms in 54.8% of patients following conservative or endovascular interventions highlights the potential of targeted therapies in improving blood flow dynamics and reducing cerebrovascular risk. However, cases with significant vertebral artery deformations showed symptom regression in 56.7% of patients, although blood flow velocity remained unchanged, indicating that structural vascular abnormalities may require long-term management strategies.Despite these significant findings, the study has certain limitations. The reliance on duplex scanning as the primary diagnostic tool, while effective, may benefit from additional neuroimaging techniques such as functional MRI and MSCT angiography to enhance diagnostic accuracy. Further studies are needed to explore the integration of these modalities in routine clinical practice. Additionally, larger sample sizes and longitudinal studies would provide a more comprehensive understanding of the long-term effects of different treatment strategies on cerebral hemodynamics.This study demonstrates that duplex scanning is a valuable diagnostic tool in detecting hemodynamic abnormalities associated with vertebrobasilar insufficiency. By providing real-time visualization of blood flow dynamics, this method enhances early diagnosis and facilitates appropriate treatment strategies, potentially reducing the incidence of stroke and other cerebrovascular complications. Future research should focus on refining diagnostic protocols and integrating advanced imaging techniques to optimize patient outcomes.
6. Conclusions
- The use of duplex scanning plays a crucial role in the early and accurate diagnosis of chronic cerebral insufficiency, particularly in patients with vertebrobasilar symptoms. This non-invasive imaging method allows for a detailed assessment of blood flow parameters, helping to identify vascular abnormalities that may contribute to cerebrovascular insufficiency.The study highlights the importance of carotid and vertebral arteries in determining the degree of hemodynamic significance of pathological deformations and stenotic changes. Duplex scanning provides valuable insights into the structural and functional state of these arteries, helping to detect vascular narrowing, occlusions, or asymmetrical blood flow that could affect cerebral circulation.Additionally, the findings emphasize the need for comprehensive vascular assessments, including functional and pharmacological tests, to evaluate the adaptive capacity of cerebral blood flow and its compensatory mechanisms. Combining duplex scanning with other advanced imaging modalities, such as transcranial Doppler ultrasound, functional MRI, and MSCT angiography, may further enhance diagnostic accuracy and improve treatment planning.In conclusion, duplex scanning remains an essential diagnostic tool for evaluating patients with suspected vertebrobasilar insufficiency. Its application in routine clinical practice can lead to timely interventions, reduced risk of ischemic events, and better management strategies for patients with chronic cerebral insufficiency.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML