Sh. A. Boymuradov, Sh. Kh. Bakieva, B. I. Karimberdiev, J. A. Djuraev
Tashkent Medical Academy, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
This article presents the results of clinical and radiological examinations of patients with trauma of maxillary sinus. Combined injuries of the paranasal sinuses (CCS) in 95% of cases are accompanied by injuries to the facial bones and skull. The presence of paranasal sinus injuries in this category of patients is characterized by a high frequency of infectious complications, manifesting both in the early and late post-traumatic periods. The frequency of complications in combined injuries reaches 80% or more, with mortality ranging from 33% to 90%. Post-traumatic sinusitis develops in patients who have been in the pulmonary ventilation apparatus for a long time, with impaired ventilation of the paranasal sinuses, causing congestion in the sinuses. These changes are a favorable background for the development of inflammatory processes.
Keywords:
Maxillary sinus, Trauma, Mucociliary transport
Cite this paper: Sh. A. Boymuradov, Sh. Kh. Bakieva, B. I. Karimberdiev, J. A. Djuraev, Characteristics of the Results of Clinical and Radiological Studies in Trauma of Maxillary Sinus, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 717-721. doi: 10.5923/j.ajmms.20251503.50.
1. Introduction
According to the World Health Organization (WHO), over the past 10 years, the number of combined injuries has more than tripled [1,2,4]. Injury is one of the three causes of death among working-age people after cancer and cardiovascular disease. Injured patients are transported to the nearest medical institutions, they receive first aid, but most often an otolaryngologist is not present during the initial examination and treatment, therefore the diagnosis and treatment of paranasal sinus injuries are delayed, and sometimes not diagnosed. Therefore, the frequency of complications in the post-traumatic period remains high [8,10,12].Combined injuries of the paranasal sinuses (CCS) in 95% of cases are accompanied by injuries to the facial bones and skull. The presence of paranasal sinus injuries in this category of patients is characterized by a high frequency of infectious complications, manifesting both in the early and late post-traumatic periods. The frequency of complications in combined injuries reaches 80% or more, with mortality ranging from 33% to 90% [3,6,10].
2. Results
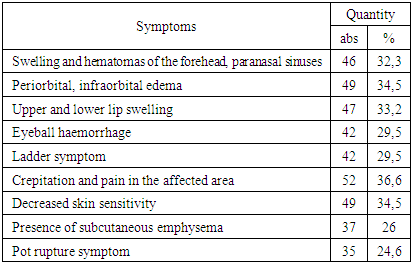
Post-traumatic sinusitis develops in patients who have been in the pulmonary ventilation apparatus for a long time, with impaired ventilation of the paranasal sinuses, causing congestion in the sinuses. These changes are favorable for the development of inflammatory processes [5,7,11].Injuries to the walls of the paranasal sinuses are often accompanied by damage and closure of the natural nasal cavities, which leads to blood filling of the cavities, which is a nutrient medium for microorganisms. In the dynamics of the course of the traumatic disease, conditions are created for hemostasis suppuration due to a decrease in the activity of the ciliated epithelium, an increase in the volume of the mucous membrane, impaired evacuation of intra-sinus substances, and functional changes in the nasal mucosa [8,9,10,11,14].Therefore, the development of therapeutic and diagnostic assistance tactics for patients with combined injuries to the maxillofacial region and the brain, the determination of rehabilitation periods for injuries to the paranasal sinuses, and the study of the functional properties of the nose are unresolved problems in modern medicine.The aim of the study is to improve the effectiveness of the results of diagnosing combined injuries of the paranasal sinuses in patients with combined injuries of the facial skeleton, skull, and other bones.The results obtained. In the study material, men constituted the majority, i.e., 78.8%, while women constituted only 21.2%. The average age of the study participants was 43.4±2.1 years. Hospitalized analysis showed that 91.5% (130 patients) were hospitalized on the first day after the injury and 7% (10 patients) on the second day after the injury, while only 1.4% (2 patients) were hospitalized on the third day after the injury.Closed craniocerebral trauma was recorded in 76.7% of patients, open craniocerebral trauma in 3.6%, craniocerebral trauma in 7.7% of patients, and no craniocerebral trauma was recorded in 12%, with other types of combined trauma identified.The overall condition and severity of the patients' injuries depended on the type of combined injury, brain damage, blood loss, shock, and the duration of first aid.Fractures of the skull bones were noted in 2.8% of patients, fractures of the nasopharyngeal-orbital complex in 10.6%, fractures of the zygomatic bone in 2.8%, fractures of the upper jaw in 2.1% of patients, fractures of the walls of the eyeball in 15.4% of patients, and in 13.4% of patients, impaired soft tissue integrity was observed, bruises and hematomas of the soft tissues of the face were noted in 48.6% of patients, and in the remaining 4.3% of patients, multiple combined.An objective examination of the patients served as the basis for the initial diagnosis, while the final diagnosis was made using the radiation method (Table 1).Table 1. Symptoms of combined traumatic brain injury n=142 (100%)
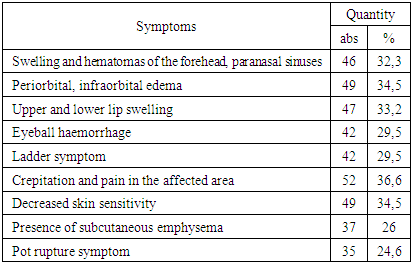 |
| |
|
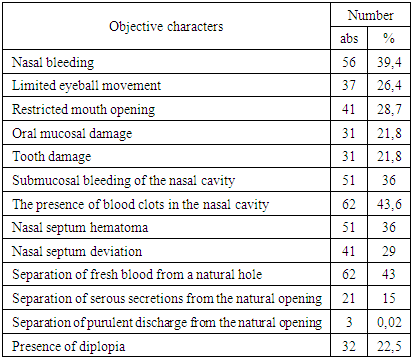
Post-traumatic edema and hematomas in the frontal and paranasal sinuses (n=46; 32.3%), periorbital, infraorbital zones (n=49; 34.5%), as well as on the upper and lower lip (n=47; 33.2%). Subcutaneous hematomas and hemorrhages of the eyeball were most frequently detected in the affected area (n=42; 29.5%).Palpation of soft and bone tissue in the affected area revealed signs of "staircase" (n=42; 29.5%), crepitus and pain in the affected area (n=52; 36.6%), as well as a decrease or disappearance of skin sensitivity in the anterior wall of the maxillary sinus (n=49; 34.5%), subcutaneous emphysema (n=37; 26%), pot rupture symptom (n=35; 24.6%).Nasal bleeding (n=56; 39.4%), limited eye movement (n=37; 26%), limited mouth opening (n=41; 29%), mucosal integrity, presence of submucosal hematomas (n=31; 21.8%), the presence of tooth lesions (n=31; 21.8% (Table 2).Table 2. Objective examination of combined injuries of the lower extremities n=142 (100%)
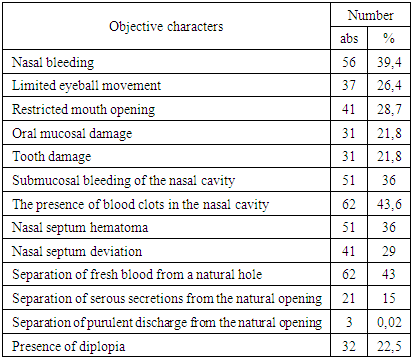 |
| |
|
Endoscopic examination of the nasal cavity revealed submucosal hemorrhages (n=51; 36%), the presence of blood clots in them (n=62; 43.6%), the condition of the lower nasal concha, the condition of the nasal septum, the condition of the natural pores, and the discharge in them.
3. Discussion
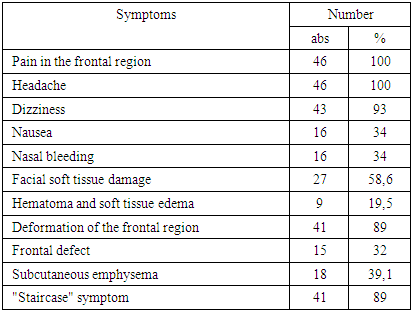
Hematoma of the nasal septum (n=51; 36%), nasal septum curvature (n=41; 28.7%), new blood from the natural opening was detected in patients (n=62; 43%), serous waste (n=21; 15%), purulent effluent (n=3; 0.02%) were detected. Purulent discharge was detected in patients with a history of chronic inflammation of the maxillary sinus. Asymmetry of the pupil line, up/down and left/right diplopia were observed in 32 (n=32; 22.5%) of patients.We divided all patients into 3 groups depending on the location of the injury:Group 1 consisted of 46 patients with combined trauma to the walls of the frontal cavity.Group 2 consisted of 49 patients with combined injuries of the maxillary sinus, nasopharyngeal-orbital complex.Group 3 consisted of 47 patients with combined damage to the walls of the upper jaw.Data from 20 healthy individuals served as a control group.Results of the clinical, radiological, and functional characteristics of patients with combined frontal wall trauma (n=46).Patients with fractures of the frontal cavities were more likely to experience pain in the frontal region (n=46; 100%), headache (n=46; 100%), dizziness (n=43; 93%), nausea (n=16; 34%), nasal bleeding (n=16; 34%) complained.Closed craniocerebral trauma was recorded in 95.6% of patients (n=44), while open craniocerebral trauma was recorded in 4.4% of patients (n=2).Of the 46 patients, 58.6% (n=27) reported facial soft tissue damage, with subcutaneous hematoma and soft tissue edema predominating, while 19.5% (n=9) showed open soft tissue damage with bone fragment displacement.In 8.6% of patients (n=4), facial bone fractures were noted, which penetrated to the base of the skull. First aid to all patients in this group included bleeding cessation, primary wound surgical treatment, respiration, and restoration of cardiovascular system function (Table 3).Table 3. Symptoms of combined frontal wall trauma n=46 (100%)
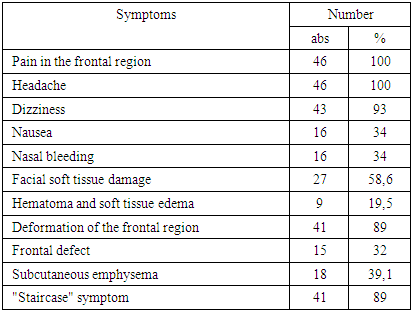 |
| |
|
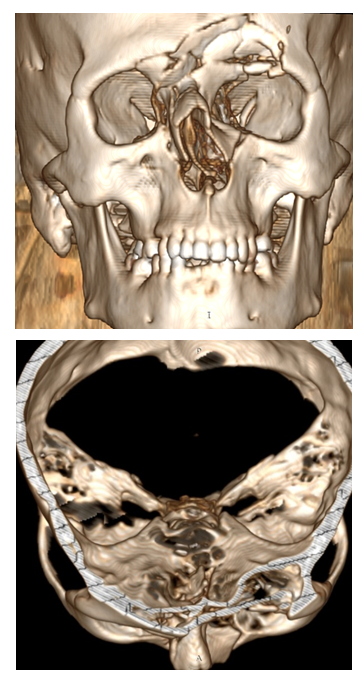
External examination revealed facial asymmetry and deformation due to soft tissue swelling in 89% (n=41), and a defect in the frontal region in 32% (n=15) of patients (Fig. 1). Palpation was painful in 100% of patients (n=46), subcutaneous emphysema was noted in 39.1% (n=18), the "step" symptom was noted in 89% (n=41), and a decrease in skin sensitivity of the frontal region was noted in 50% (n=23).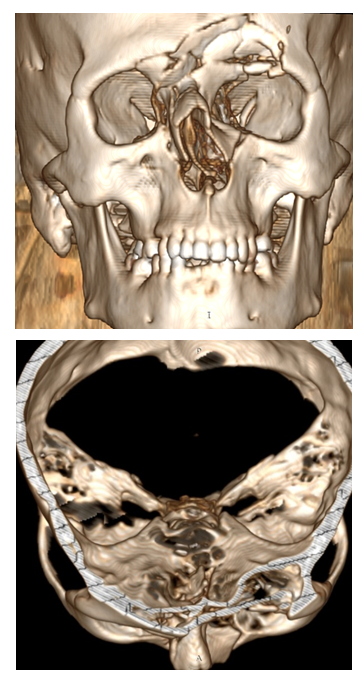 | Figure 1. Fracture of the anterior wall of the frontal sinus, sagittal section |
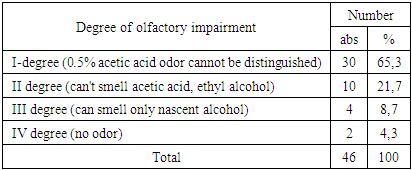
MSCT revealed anterior frontal wall fractures in 95.6% (n=44), and anterior and posterior wall fractures in only 4.4% (n=2). In 95.6% of patients (n=44), MSCT revealed the presence of blood in the sinuses, while only 1 patient showed the presence of serous fluid in the sinuses. In 34% (n=16) of patients, displacement of bone fragments of the anterior wall of the frontal cavity was observed, while in 65.3% (n=30) of patients, fractures of the frontal walls were observed without displacement of bone fragments.Furthermore, in patients with head injuries, we (n=9; 19%), nasal septum deviation (S-shaped, ridge, protrusion), pneumatization of the middle nasal concha (conha bullosa) (n=5; 11%), C-shaped curvature of the nasal septum (n=16; 34%), lateral displacement of the middle nasal concha (n=6; 13%), hypertrophy of the coracoid process (n=16; 34%), respectively.Olfactometry was performed according to the following scheme:Grade I - mild hyposmia - impaired sense of weak odors (rose oil, honey wax, ground coffee), does not smell 0.5% acetic acid;Grade II - pronounced hyposmia - does not detect weak or moderate odors (lemon oil, vanilla, ground cinnamon, valerian tincture, cloves, tobacco), cannot distinguish the odor of acetic acid, ethyl alcohol;Grade III - pronounced hyposmia - weak and moderate odor insensitivity, a decrease in strong intensity odor sensitivity, good reaction to irritants (strong substance of acetic acid solution, ethyl alcohol, menthol, camphor oil) (stimulating agents - nasathic alcohol, formaldehyde, acetone), able to distinguish only the odor of nasathic alcohol;Grade IV - anosmia (can't distinguish any odor).Olfactometry data showed that 65.3% (n=30) of patients had mild hyposmia, 21.7% (n=10) had pronounced hyposmia, 8.7% (n=4) had significant hyposmia, and 4.3% (n=2) had anosmia (Table 4). These odor disorders are associated with damage to the peripheral olfactory reflex, which can be considered a disorder of olfactory function, and in patients without bone fragment displacement, odor disorders of the nasal mucosa are caused by swelling of the nasal mucosa. Patients with displacement of bone fragments and brain damage experience impairment of both peripheral and central parts of the olfactory system.Table 4. Olfactometric parameters in patients with frontal wall damage were n=46 (100%)
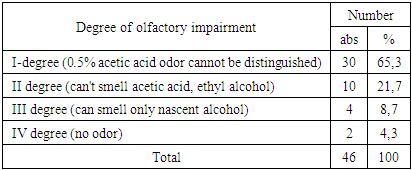 |
| |
|
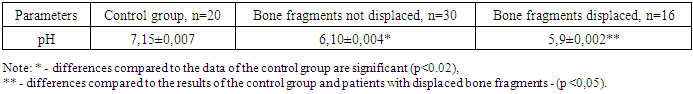
Results of the study of the pH of nasal secretion in this group of patients showed that in patients without displacement of bone fragments (n=30), the displacement (n=20) into an acidic environment was 6.10±0.004 (P<0.02) compared to the control group (7.15±0.007), and in patients with displacement of bone fragments (n=16) the indicators were even lower than in patients without displacement of bone fragments - 5.9±0.002 (P<0.05) (Table 5).Table 5. Nasal secretion indices (pH) in patients with frontal wall damage n= 46 (100%)
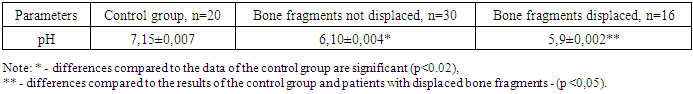 |
| |
|
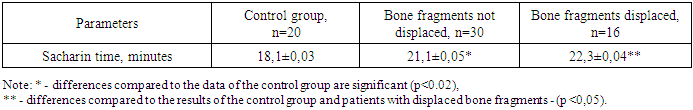
Mucociliary clearance results showed that saccharine time was 21.1±0.05 longer in patients with bone displacement n=30 compared to patients in the control group of 18.1±0.03 (P<0.02), while in patients with bone displacement n=16 this time was longer than in the control group of 22.3±0.04 (P<0.05) (Table 6).Table 6. Mucociliary clearance indices in patients with anterior wall trauma were n= 46 (100%)
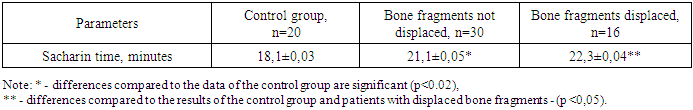 |
| |
|
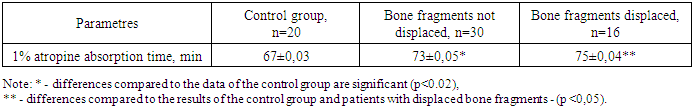
These disorders of mucociliary clearance are associated with damage and swelling of the nasal mucosa, which led to a slowing of mucosal movement, while in patients with displaced bone fragments, this disorder is exacerbated by displacement of bone fragments, which leads to a disruption of the architecture of the nasal cavity.The study of the nasal mucosa's absorptive function was conducted as follows: a gauze turunda, moistened with a 1% solution of atropine, was placed in the nasal passage of the examined nasal half for 15 minutes. The results showed that in n=30 patients without displacement of bone fragments, it was 73±0.05 minutes, i.e., midriaz (narrowing of the pupil) occurred 6±0.02 minutes later than the control group (P<0.02) and in n=16 patients with displacement of bone fragments, this indicator was 75±0.04 minutes, i.e., midriaz occurred 8±0.04 minutes later than in the control group (P<0.05) (Table 7).Table 7. The indicators of nasal mucosal absorption function in patients with damage to the walls of the frontal cavity were n=46 (100%)
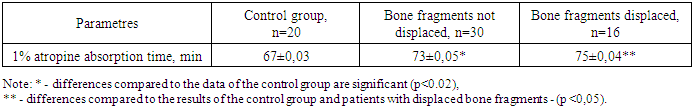 |
| |
|
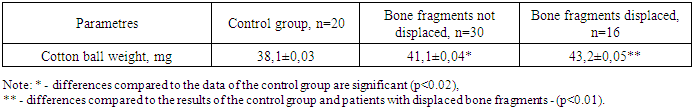
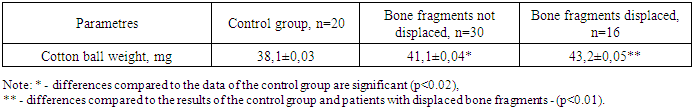
Significant attention was also paid to the study of the nasal excretory function. For this purpose, a cotton ball weighing 25 mg was inserted into the nasal cavity between the inferior nasal concha and the nasal septum. After 1 minute, the cotton ball was taken and weighed.The results showed that in patients with bone fragment displacement n=30, the mass of the sphere was 41.1±0.04 mg, which is 3.1±0.04 mg heavier than the weight of the control group (P<0.02), while in patients with bone fragment displacement n=16, this indicator was 43.2±0.05 mg, which is 5.1±0.04 mg heavier than the weight of the control group (P<0.01) (Table 8).Table 8. Nasal excretory function indices in patients with frontal cavity wall damage were n=46 (100%)
 |
| |
|
In the dynamics of treatment of patients with damage to the frontal wall, an increase in neutrophils was observed compared to the control group. The absolute number of neutrophils in the control group was 53.9±5.7, in these patients, the absolute number of neutrophils was 53.8±5.8 in the first 1-3 days, 54.7±5.4 on the 7th day, and increased to 55.9±5.6 on the 14th day, and at the end of treatment, i.e., on the 21st day, it was 56.1±5.7, the difference compared to the control group was significant (P<0.01).The absolute number of macrophages in the control group was 0.39±0.1, while in patients it increased by 0.38±0.1 on the first 1-3 days, by 0.40±0.1 on the 7th day, and by 0.39±0.2 on the 14th day, and by the end of treatment, i.e., on the 21st day, it was 0.40±0.2, which was significantly different from the control group (p<0.01).The phagocytosis index in the control group was 22.09±2.5, in patients on the first 1-3 days it was 22.07±2.4, on the 7th day it was 23.09±2.2, on the 14th day it was 23.07±2.1, on the 21st day it was 24.19±2.1, i.e. it differed significantly from the control group.The level of lymphocytes, eosinophils, cylindrical, squamous epithelium, and chyme did not differ from the control group. It can be concluded that on days 14 and 21, inflammation in the nasal cavity increases in the dynamics of treatment, which requires correction during treatment to prevent post-traumatic complications.
4. Conclusions
Therefore, it can be summarized and concluded that, according to the results of the conducted research, it has been established that damage to the maxillary sinus is accompanied by a decrease in the volume of the frontal cavity, leading to impaired function. The upper wall is most often damaged (72%). Therefore, comprehensive treatment is required. The level of lymphocytes, eosinophils, cylindrical, squamous epithelium, and chyme did not differ from the control group. In the dynamics of treatment, it can be concluded that on days 14 and 21, inflammation in the nasal cavity intensifies.
References
| [1] | Agzamova S. Retrospective analysis of the condition of ophthalmological status in traumas of the scoop-orbital complex // Stomatology. - 2021. - T. 1. - No. 1 (82). - С. 89-92. |
| [2] | Boymuradov Sh. Innovative methods of treatment of combined injuries of the bones of the facial skeleton based on algorithmization of the doctor's activities // Journal of Problems of Biology and Medicine. - 2015. - No. 1 (82). - С. 29-33. |
| [3] | Dorovskyi G.N. Radiation diagnostics of polytrauma: dis. Moscow State Medical Dental Institute named after A.I. Evdokimov. Moscow. 2014, 2014. |
| [4] | Dorovskyi G. N. Comparative analysis of sensitivity and specificity of various methods of radiation diagnostics in polytrauma // Acta Biomedica Scientifica. - 2014. - No. 4 (98). - С. 24-28. |
| [5] | Ilyasov D.M. Treatment tactics for nasal cavity injuries in patients with severe combined head trauma: dis. - Ilyasov Denis Maratovich. 2013.-24c, 2013. |
| [6] | Maday D. Yu., Golovko K. P. Minimally invasive methods in the treatment of severe craniocerebral injuries // Health. Medical ecology. Science. - 2012. - T. 47. - No. 1-2. - С. 41-42. |
| [7] | Z.K. Norboyev et al. Algorithm for diagnosing traumatic injuries and post-traumatic complications in the area of the frontal sinus // Questions of Science and Education. - 2018. - No. 26 (38). - С. 72-74. |
| [8] | Pavlova O.Yu. et al. Radiation diagnosis of facial bone injuries // Russian electronic journal of radiation diagnostics. - 2014. - T. 4. - No. 3. - С. 39-45. |
| [9] | Popova I. E. et al. Modern aspects of diagnosing severe combined trauma using computed tomography // Vestnik meditsinskogo instituta "Reaviz": rehabilitation, doctor and health. - 2021. - No. 3 (51). - С. 28-37. |
| [10] | Saurasova N.A. et al. X-ray diagnostics of traumatic injuries to the maxillofacial region. - 2017. |
| [11] | Samykin A. S. Characteristics of treatment for traumas of the scoop-orbital complex // Universum: Medicine and Pharmacology. - 2014. - No. 3 (4). - С. 4. |
| [12] | Urgunaliyev B. K., Shaiahmetov D. B., Tsoy A. R. Modern approaches to the diagnosis of fractures of the bones of the facial skeleton // Russian dental journal. - 2018. - Т. 22. - No. 6. |
| [13] | Shedrenok V. V. et al. Clinical and radiological diagnostics of craniocerebral injuries in polytrauma //Vestnik xirurgii imeni AI Grekova. - 2012. - T. 171. - No. 2. - С. 41-44. |
| [14] | Yusupov Sh., Boymuradov Sh. Modern aspects of diagnosis and planning of surgical treatment of fractures of the maxillary-orbital complex // Journal of the doctor's announcer. - 2018. - T. 1. - No. 4. - P. 129-134. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML