-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 707-710
doi:10.5923/j.ajmms.20251503.48
Received: Feb. 5, 2025; Accepted: Mar. 8, 2025; Published: Mar. 15, 2025

Results of the Analysis of Clinical-Instrumental Investigation of Patients with Upper Jaw Cyst
U. S. Xasanov, J. A. Djuraev, A. I. Muhiddinov
Tashkent Medical Academy, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Chronic sinusitis (CS) is a common disease in otorhinolaryngology. Cysts of the nasal lateral cavities play an important role in the structure of chronic sinusitis. According to foreign sources, chronic upper jaw cysts accounted for about 24% of hospitalized patients in 2021. These data correspond to the data of world literature. It is known that most cysts of the upper jaw are asymptomatic, and in almost 80% of cases they are radiographic findings [2]. The etiology of nasal lateral cavity cysts is unclear: they can be associated with allergic and other inflammatory processes of the mucous membrane of nasal approaching cavity cysts, trauma, periapical and periodontal infections, and even relative humidity and changes in room temperature [4].
Keywords: Maxillary sinuses, Tensioreceptors, Acute and chronic sinusitis, Cysts, Otorhinolaryngology
Cite this paper: U. S. Xasanov, J. A. Djuraev, A. I. Muhiddinov, Results of the Analysis of Clinical-Instrumental Investigation of Patients with Upper Jaw Cyst, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 707-710. doi: 10.5923/j.ajmms.20251503.48.
1. Introduction
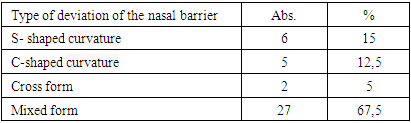
- Improved diagnosis of these diseases led to a significant increase in the percentage of cysts among the total number of diseases of the paranasal sinuses. In a study of 500 healthy people, maxillary sinus cysts were found in 9.6%, and in an analysis of 1080 panoramic radiographs, 8.7% of patients [6]. When examining patients with paranasal sinus pathology, 18.1% of such patients maxillary sinus cysts are identified [1-5]. Most often, cysts of the maxillary sinuses do not manifest themselves clinically. But if they have a large size, they can cause a headache due to the pressure of the cyst shell on the sinus walls and can be accompanied by difficulty in breathing through the nose. However, the size of the cyst does not always depend on the severity of the symptoms it causes [7].When there are clinical signs of upper jaw cavity cysts, the treatment tactics are clearly defined and consist of surgical treatment [8]. However, at the asymptomatic stage of the disease, when jaw cysts are diagnosed during a preventive X-ray examination, the approach to treatment is usually vague and in most cases determined by the size of the identified formation [10]. The introduction of microscopic and endoscopic technology into practice allowed the operation physician to perform a more detailed analysis of all endonasal anatomical structures, assess their interrelationship and their role in the development of the pathological condition [9]. From an anatomical point of view, the nasal cavity is the most complex organ, and the functional significance of many endonasal anatomical structures is still unclear today.Thus, the analysis of various literature has demonstrated that the problem of course and formation of cysts of the upper jaw cavity is one of the important points of otorhinolaryngology. All this underscores the need for a deeper study of the etiotogenetic aspects of this pathology.Despite the many studies available on upper jaw cysts, this problem continues to attract clinicians due to the trend of accelerating the growth of incidence in recent years, the uncertain etiology and complexity of the pathogenesis, and the insufficient effectiveness of available treatments. This allows us to consider that the problem of upper jaw cysts has not been fully solved and requires further study.Our analysis of the results of our survey of patients with upper jaw cysts (n = 40) showed that in 38 examined patients (95%) who presented themselves to an otorhinolaryngologist, the main complaints were frequent sinusitis and difficulty breathing through the nose. 9 (22.5%) patients reported painful sensations in the projection of the upper quadrant, which was affected by a sharp change in barometric pressure (taking a high-speed elevator or flying an airplane). 3 (7.5%) patients noted a feeling of heaviness that occurs intermittently in the affected upper quadrant projection, which is exacerbated when the head is bent.The intensity of the headache does not depend on the size of the cyst: in some patients, despite the presence of a large cyst that fills the entire sinus, there may be no complaints about headache, and in some patients small cysts can cause enough swelling. severe headache.The mechanism of headache with sinus cysts is complex and poorly understood. In our opinion, the occurrence of headache depends on the specific characteristics of the innervation of the mucous membrane. Morphological studies show that one of the main forms of receptors in the mucous membrane of the upper jaw are simple widespread receptors with diffuse branching of the terminals, which can be observed in many fields of view of the microscope. Similar sensitivity nodes are found in many connective tissue membranes of the body: sclera; in the pia mater, in the dura mater, in the mucous membrane of the sphenoid sinus. Such receptors respond to stretching, that is, they are tensioreceptors.In the mucous membrane of the upper jaw, these receptors probably respond to irritation caused by changes in air pressure that occur in the sinuses during breathing. Apparently, thanks to the impulses received by these receptors, the mucous membrane of the upper jaw is involved in the reflex regulation of breathing. In our opinion, these receptors sense irritation from large areas of the mucous membrane, affect the pressure that occurs in the sinuses during various injuries (acute and chronic sinusitis, cysts) and painful sensations in case of strong irritation. gives Impulses from these sensory receptor devices reach afferent sympathetic fibers along the fibers of the trigeminal and vagus nerves and are manifested in headaches of varying intensity. Irritation of receptors increases as the cyst enlarges and the pressure of the cyst contents accumulated in it gradually increases.Headaches in patients with cysts of the maxillary head are often dull and intermittent, but their intensity has increased over the years. Taking analgesics that are widely used in everyday life (citramon, analgin, pyramidon, baralgin) led to the elimination of headache. Since most patients did not have rhinologic symptoms, 27.5% of patients (11 patients) we observed sought medical help from a therapist or neurologist, who immediately or after some time referred patients for diagnostic x-rays of the paranasal sinuses. Unsuccessful treatment allowed to confirm the diagnosis of this cyst.There were no headaches in 3 patients, which was 7.5% of the treated patients, X-rays were found at the medical examination or military medical commission;37 patients with cysts of the maxillary head had different degrees of nasal breathing difficulties. Patients describe nasal congestion that bothers them in different ways: some patients experience nasal congestion at night on the side facing the pillow; in other patients, breathing difficulties occurred several times during the day in one or the other half of the nose; 12 patients had to take vasoconstrictor drops intermittently for a period of 1 to 7 months due to difficulty in nasal breathing.During endoscopic examination, swelling and congestive hyperemia of the lower and middle turbinates on both sides were found in these patients. After lubricating the nasal passages with a 0.1% solution of adrenaline, they are reduced and nasal breathing is restored. Thus, the expansion of the nasal cavity and, as a result, the obstruction of the nasal cavity was associated with the filling of the cavernous venous plexuses with blood. Some of these patients had scanty, mild mucus discharge.In 80% of patients with cysts of the upper jaw, difficulty in nasal breathing was previously explained by their allergic background. However, our careful study of the allergic history of these patients did not confirm allergy. In our opinion, nasal breathing disorders in some patients with maxillary sinus cysts are not only due to local changes in the blood and lymph circulation of the sinus and nasal mucosa as a result of mechanical pressure of the cyst on the mucous membrane. as well as a reflex developing imbalance of the autonomic nervous system in the direction of increasing the tone of its parasympathetic division, which is manifested by vasodilatation in both halves of the nose, filling of the cavernous venous plexuses with excess blood, and obstruction of the lumen. of the nasal cavity.Thus, the leading complaint in the clinical symptoms of cysts of the upper jaw is headache. Without being strong, it has a tendency to increase gradually, it limits the patient's ability to work, causes a state of constant discomfort and eventually forces him to seek medical help.55% of patients reported that they had between 1 and 3 to 5 sinusitis within 5 years. 5 patients underwent surgical treatment in accordance with professional requirements. According to the anamnesis that we collected, the above complaints disturbed patients with cysts of the upper jaw at the age of 1,5 to 10 years, whereas in 36 patients, the average duration of the disease was 3,6 years, and in 4 patients at the next dispensary examination revealed nasal cavities and nasal cavities. We also found that 35 patients used decongestants or topical corticosteroids on a regular basis.According to the results of the previous rhinoscopy and endoscopic examination of the nasal cavity, we diagnosed a deviation of the nasal septum. More than 2/3 (70%) of the patients we observed had a mixed form of curvature of the nasal septum, that is, there is a combination of several types of deviations (see Table 1).
|
2. Discussion
- The results of our study provide a deeper understanding of the clinical manifestations, diagnostic findings, and therapeutic approaches for upper jaw cysts. Our findings align with previous literature that highlights the asymptomatic nature of many maxillary sinus cysts, as well as their incidental discovery through radiographic imaging in a significant percentage of patients. The observed prevalence of upper jaw cysts in our sample is consistent with global trends, reinforcing the notion that these formations are an important clinical concern in otorhinolaryngology.One of the key findings of our study is the complex and variable nature of the symptoms associated with maxillary cysts. While a large proportion of patients reported symptoms such as frequent sinusitis and nasal congestion, others experienced intermittent headaches and sensations of heaviness, particularly influenced by changes in barometric pressure. Interestingly, our findings support previous studies indicating that the intensity of headache does not necessarily correlate with cyst size. This suggests that the mechanism of headache in such cases may be more closely related to the involvement of sensory receptors and neural pathways rather than mechanical compression alone. The role of tensioreceptors in the mucous membrane of the maxillary sinus, as proposed in our study, could provide a plausible explanation for this phenomenon and warrants further histopathological investigation.The study also highlights the significant impact of nasal obstruction among patients with maxillary cysts. Our findings suggest that nasal congestion in these patients is not merely due to physical obstruction by the cyst but may also result from reflex autonomic dysfunction. The observed vasodilatation and congestion of venous plexuses in the nasal cavity could be attributed to an increased parasympathetic response, leading to further impairment of nasal airflow. This is an important consideration for clinicians, as it underscores the need for a comprehensive assessment of nasal function in patients presenting with upper jaw cysts.From a diagnostic perspective, the role of endoscopic and radiological evaluation in identifying cystic formations was reaffirmed in our study. The use of computed tomography (CT) and panoramic radiography proved to be essential tools in detecting cysts that were otherwise asymptomatic. Additionally, our findings suggest that deviation of the nasal septum is frequently observed in patients with maxillary cysts, with a majority exhibiting mixed forms of septal curvature. This raises an important clinical question regarding the potential relationship between anatomical variations and the development or exacerbation of cyst-related symptoms.In terms of treatment strategies, our findings reinforce the necessity of individualized management approaches based on symptom severity and cyst characteristics. While surgical intervention remains the preferred option for symptomatic or enlarging cysts, there is ongoing debate regarding the management of asymptomatic cases. Our study supports the idea that cysts detected incidentally should be carefully monitored, with a particular emphasis on evaluating their potential impact on nasal breathing and overall quality of life. Furthermore, the role of minimally invasive surgical techniques, such as endoscopic sinus surgery, should be further explored to optimize treatment outcomes and reduce post-operative complications.Overall, the results of our study highlight the need for continued research into the etiology, pathophysiology, and management of upper jaw cysts. Despite advancements in diagnostic imaging and surgical techniques, several aspects of this condition remain poorly understood. Future studies should focus on identifying predictive factors for cyst progression, as well as evaluating the long-term outcomes of different treatment modalities. By addressing these knowledge gaps, we can improve the clinical approach to maxillary sinus cysts and enhance patient care in otorhinolaryngology.
3. Summary
- Thus, our study showed that cysts of the maxillary cavity are a common pathology that an otorhinolaryngologist should deal with in his clinical practice.By examining the CT anatomy of the nose and the nasal lateral cavities, we found that the crista conchalis area of the upper jawbone is the anterior part of the medial wall of the upper jaw, which is located significantly ahead of the crescent crescent. The lateral wall of the lower nasal cartilage. It is also worth noting that the crista conchalis is located 3.49±0.02 mm below the protrusion level of the upper jaw cavity. In this regard, we chose the crista conchalis area as the site for endonasal trefation of the upper jaw.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML