U. S. Xasanov, J. A. Djuraev, A. I. Muhiddinov
Tashkent Medical Academy, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Among all forms of chronic sinusitis, maxillary sinus cysts are a common pathology. According to different authors, the prevalence of cysts of the mucous membrane of the upper jaw, in turn, is 3.5-16.4%. Depending on the diagnostic method used by sinus pathologists, the numbers can vary significantly. Thus, according to CT data of the paranasal sinuses, the incidence rate of maxillary cysts in the general population ranges from 1.4% to 35.6%. Cysts of the mucous membrane of the maxillary cavity are benign tumors that occur as a result of the blockage of the seromucous gland duct in the mucous membrane of the cavity or as a result of the accumulation of fluid between the epithelial layer and the mucous membrane. In the first case, the pathological process leads to the accumulation of mucus and cystic expansion of the gland. Such cysts are called secretory cysts of the mucous membrane or retention cysts. Retention cysts are lined by epithelium and contain mucous or serous fluid. In the second case, they talk about secretory cysts of the mucous membrane.
Keywords:
Cyst, Membrane, Allergy, Air, Gland, Tissue
Cite this paper: U. S. Xasanov, J. A. Djuraev, A. I. Muhiddinov, Surgical Treatment Cysts of Maxillary Sinuses, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 704-706. doi: 10.5923/j.ajmms.20251503.47.
1. Introduction
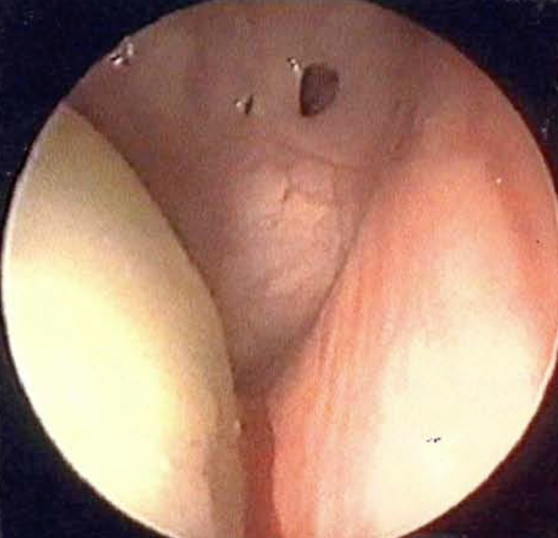
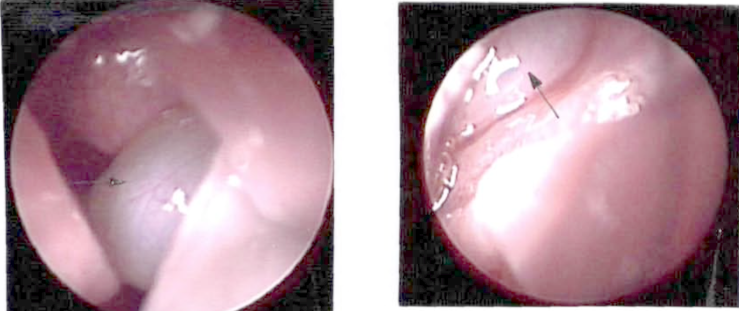
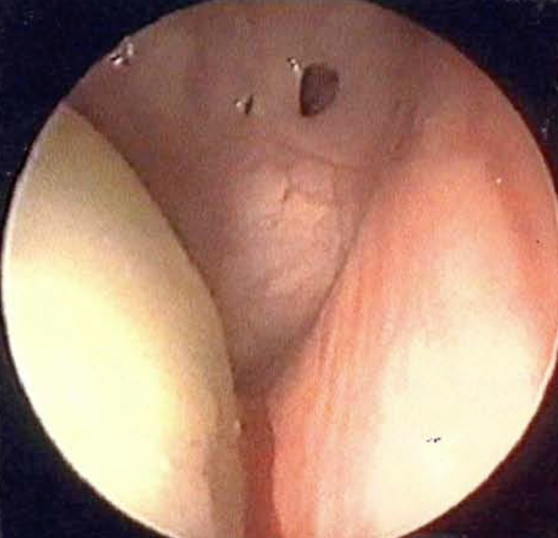
All patients with cysts of the maxillary cavity underwent endoscopic examination of the nasal cavity before surgery in the endoscopic dressing room or in the operating room. Before the endoscopic examination, the surface of the nasal mucosa was anesthetized with a 3% solution of dicaine or a 10% solution of lidocaine, to which a 0.1% solution of adrenaline was added to achieve a vasoconstrictor effect. After that, a complete examination of the nasal cavity was carried out with special attention.They consider the nasal passages, the nasal septum, the ostiomeatal complex, the lateral wall of the middle concha, and the nasopharynx. The examination was carried out using 0°, 30°, 70° optical endoscopes with simultaneous recording of the endoscopic image on a video recorder. During endoscopy, attention was paid to the location and size of the uncinate process, ethmoid bladder, natural sinus anastomosis, their interrelationship, and the presence of purulent discharge from the sinus through the anastomosis.The anastomosis was open in all patients with maxillary cysts. Only 3 patients had an anastomotic obstruction: in 2 cases - large cysts squeezed into the nasal cavity through the anastomosis (Picture 1 a, b), and in one case the anastomosis was closed with a stem. antrochoanal polyp developed from a sinus cyst. This patient developed chronic suppurative sinusitis (Picture 2).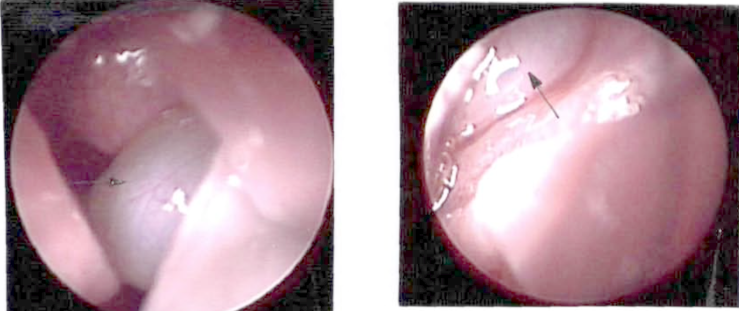 | Picture 1. a, b. Endoscopic picture of a) left half of the nose, b) right half of the nose. The part of the cyst that came out through the anastomosis into the nasal cavity (shown in white) |
 | Picture 2. Purulent discharge from the left upper jaw above the antrochoanal polyp |
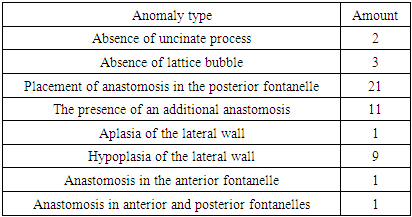
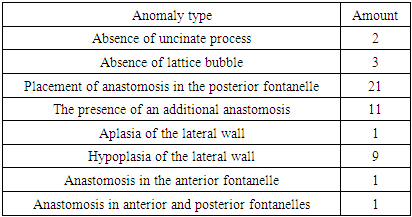
The exudative form of damage to the mucous membrane of the cavity develops in cases where the anastomosis is blocked, secretion products of the cavity accumulate, bacterial and viral microflora are activated. If the anastomosis is open, unhindered outflow of secretion from the cavity is ensured, therefore, in our other patients with cysts, we did not observe accumulation of exudate in the cavity. The study of the transport function confirmed the active work of ciliated epithelial cilia.Analyzing the structural features of the lateral wall of the nasal cavity during endoscopic examination from both the nasal cavity through the infundibulum and from the maxillary cavity, we noted various anomalies of its development in 40% of patients: the uncinate process or absence, hypoplasia or. aplasia of the lateral wall of the nasal cavity with the formation of posterior or anterior fontanelles, the absence of the ethmoid bladder and crescentic fissure, the location of the anastomosis in the posterior fontanelle, the presence of an additional anastomosis, the fontanelle combination of the anterior and posterior anastomoses (Picture 3). The developmental abnormalities we identified are listed in Table 1.Table 1. Anomalies in the development of the lateral wall of the middle shell in cysts of the upper jaw cavity
 |
| |
|
 | Picture 3. Endoscopic image of the medial wall of the upper jaw cavity. Three fistulas were formed in the large background, and a large cyst was formed in the sinus |
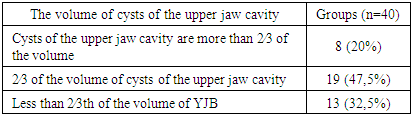
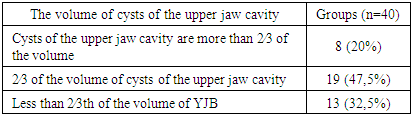
A combination of several anomalies was noted in 9.9% of patients, the most common of which were one or more large anastomoses in the posterior fontanelles, absence of the uncinate process, and ethmoid bladder.When the middle passage of the nasal cavity was examined, In all patients with cysts of the upper jaw, the mucous membrane of this area is moist and light pink in color, corresponding to a VAS score of 0 with n = 40 (p<0,01).The result of this study was one of the indirect signs in the comprehensive assessment of the condition of the mucous membrane of the upper jaw and the structures of the cerebral cortex. We determined the diagnosis of chronic rhinitis together with the patient's complaints, anamnesis and objective rhinoscopic picture (front and back rhinoscopy, endoscopic examination of the nasal cavity), diagnostic anemia of the mucous membrane of the lower nasal passage. As a result of our study, we found that all 40 (100%) patients had fibrous hypertrophy of the posterior parts of the lower nasal passage.The distribution by the occupied volume of upper jaw cavity cysts is presented in the table. Table 2. The size of the maxillary cyst in the studied patients
 |
| |
|
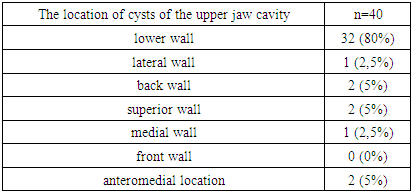
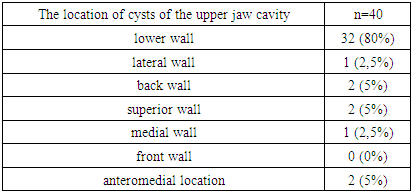
The data presented in Table 2 show that in our study, upper jaw cysts occupied 2/3 of the MS volume in 19 (47.5%) people, and less than 2/3 of the MS volume in 13 (32.5%) people. 3 of the MS volumes were in 8 (20%) patients.The location of upper jaw cavity cysts in patients examined by CT data of nasal proximal cavity cysts is shown in Table 3.Table 3. Location of maxillary cyst in the maxillary cavity in the examined patients (n=40)
 |
| |
|
From the data presented in Table 3, it can be seen that in 80% of patients in our study, the cyst was located in the area of the lower wall of the maxillary cavity, 2.5% was located in the area of the lateral wall, 5% - in the area of the back wall, and 2.5% in the anteromedial location, 2.5% - in the anterior wall soxida, and approximately 2.5% - medial and 5% from the superior wall.The anatomical features of the nasal cavity do not allow to measure it completely. In this regard, we decided to use the CT method in our work. This study allows to recreate the image of anatomical structures in any selected plane with high spatial resolution. Spiral CT allows not only to identify the pathology, but also to determine the syntopy of the area of interest to the surgeon. This method allows to visually assess the options of the anatomical structure of the studied area and measure the structures, to get a more complete picture of the individual form of the studied object.We identified the diagnosis of upper jaw cavity cysts by X-ray examination of the nasal adjacent cavities, while the upper jaw cavity cysts were partially blackened by a round shade. Subsequently, we performed a computed tomography of the nasal proximal cavities in order to rule out the presence of periapical pathology of the upper jaw teeth and to determine the nature of the lesion in the upper jaw and the individual structural features of the cavity structures. According to the results of the X-ray examination, we ruled out the odontogenic nature of the disease.Examining a CT scan of the nasal proximal cavities, we found that in all studies, the cysts of the damaged upper jaw cavity did not show radiographic signs of free exudate, which corresponds to a VAS score of 0 with n = 40 (p<0.01). The result of this study became one of the indirect markers in a comprehensive assessment of the state of transportation of the mucous membrane of the upper jaw and the structures of the cerebral hemisphere.
2. Conclusions
In order to develop a method of safe surgical access of the maxillary cavity through the crista conchalis, we conducted a vector CT study of the maxilla aimed at determining the angular values of the bone thinning direction. stack using a surgical drill. After carrying out vector analysis and statistical processing of the obtained data, we found that the desired value Ů is equal to 30.01±0.01° (p<0.01). Based on objective research results, we have developed an original endonasal surgical approach of the upper jaw that does not damage adjacent structures such as the lacrimal drainage system.
References
| [1] | Akhundjanov U. S. K. N. A., Djuraev A. Z. S. J. A. INITIAL STATE OF COCHLEOVESTIBULAR FUNCTION IN PATIENTS WITH HD WITH CVD. – 2022. |
| [2] | Botirov A. J. et al. Clinical and morphological results of xenografts to use in myringoplasty // The International Tinnitus Journal. – 2020. – Т. 24. – №. 1. – С. 1-6. |
| [3] | Boymuradov S. A. et al. RESULTS OF ELIMINATION OF POST-TRAUMA DEFORMATIONS OF THE FACIAL AND JAW AREA (LIPOFILLING) // Oriental Journal of Medicine and Pharmacology. – 2023. – Т. 3. – №. 02. – С. 1-13. |
| [4] | Djuraev J. A. et al. MIGRAINE: BASIC PRINCIPLES OF TREATMENT AND PREVENTION // International Journal of Medical Sciences And Clinical Research. – 2023. – Т. 3. – №. 02. – С. 88-91. |
| [5] | Djuraev J. A. et al. MODERN METHODS OF TREATMENT OF VIRAL HEPATITIS // International Journal of Medical Sciences And Clinical Research. – 2023. – Т. 3. – №. 02. – С. 69-75. |
| [6] | Djuraev J. A. et al. POLYCYSTIC OVARY SYNDROME: A MODERN VIEW ON THE PROBLEM // International Journal of Medical Sciences And Clinical Research. – 2023. – Т. 3. – №. 02. – С. 83-87. |
| [7] | Djuraev J. A. et al. Results of Frequency Analysis Distribution of Polymorphism Rs1800895 592c> A In Il10 Gene among Patients with Chronic Polypoid Rhinosinusitis // The International Tinnitus Journal. – 2021. – Т. 25. – №. 2. – С. 176-180. |
| [8] | Djuraev J. A. Prevalence of Allelic and Genotypic Variants of Il4, Il10, Il12b and Tlr2 Gene Polymorphism in Patients with Chronic Polypoid Rhinosinusitis. |
| [9] | Djuraev J. A., Fayozov S. F. Rhinoplasty In Combined Deformations Of The Nose // International Scientific and Current Research Conferences. – 2021. – С. 58-59. |
| [10] | Khasanov U. S. et al. A COMPLEX APPROACH TO THE TREATMENT OF ACUTE SENSONEURAL HEARING LOSS OF DIFFERENT GENES // Oriental Journal of Medicine and Pharmacology. – 2023. – Т. 3. – №. 02. – С. 14-25. |
| [11] | Khasanov U. S. et al. BOLALARDA EKSUDATİV OTITNI DAVOLASH USULI // Oriental Journal of Medicine and Pharmacology. – 2022. – Т. 2. – №. 1. – С. 64-80. |
| [12] | Khasanov U. S. et al. INITIAL STATE OF COCHLEOVESTIBULAR FUNCTION IN PATIENTS WITH HD WITH CVD // The American Journal of Medical Sciences and Pharmaceutical Research. – 2022. – Т. 4. – №. 01. – С. 60-73. |
| [13] | Khasanov U. S. et al. METHOD FOR THE TREATMENT OF EXUDATIVE OTITIS MEDIA IN CHILDREN // Oriental Journal of Medicine and Pharmacology. – 2022. – Т. 2. – №. 01. – С. 64-81. |
| [14] | Khasanov U. S. et al. Results of audiometrical indicators of cochlevestibular disorders in patients with arterial hypertension disease // Oriental Journal of Medicine and Pharmacology. – 2023. – Т. 3. – №. 02. – С. 26-36. |
| [15] | Khasanov U. S. et al. Results of audiometrical indicators of cochlevestibular disorders in patients with arterial hypertension disease // Oriental Journal of Medicine and Pharmacology. – 2023. – Т. 3. – №. 02. – С. 26-36. |
| [16] | Khasanov U. S. et al. Results of frequency analysis distribution of A1188C RS3212227 polymorphism in the IL 12B gene among patients with chronic rhinosinusitis polyposis // Oriental Journal of Medicine and Pharmacology. – 2022. – Т. 2. – №. 01. – С. 104-115. |
| [17] | Khasanov U. S. et al. VESTIBULAR ANALYZATOR TEST RESULT INDICATORS OF COCHLEOVESTIBULAR DISORDERS ON THE BACKGROUND OF ARTERIAL HYPERTENSION // Oriental Journal of Medicine and Pharmacology. – 2023. – Т. 3. – №. 02. – С. 37-44. |
| [18] | Khasanov U. S., Abdullaev U. P., Djuraev J. A. Results of audiological examination in acute sensorineural hearing loss of various genesis // Oriental Journal of Medicine and Pharmacology. – 2022. – Т. 2. – №. 01. – С. 24-50. |
| [19] | Khasanov U. S., Akhundjanov N. A., Djuraev J. A. DYNAMICS OF HEARING DISORDERS IN PATIENTS WITH ARTERIAL HYPERTENSION UNDER THE INFLUENCE OF HYPOTENSIVE THERAPY // International Journal of Medical Sciences And Clinical Research. – 2022. – Т. 2. – №. 10. – С. 16-20. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML