-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 675-677
doi:10.5923/j.ajmms.20251503.40
Received: Feb. 19, 2025; Accepted: Mar. 11, 2025; Published: Mar. 13, 2025

Adverse Effects of Anti-Tuberculosis Drugs in Patients with Pulmonary Tuberculosis Carrying Different Haptoglobin Phenotypes
Tashpulatova Fatima Kudratovna
Doctor of Medical Sciences, Associate Professor of the Department of Infectious Diseases, Pediatric Infectious Diseases, Phthisiology and Pulmonology, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Correspondence to: Tashpulatova Fatima Kudratovna, Doctor of Medical Sciences, Associate Professor of the Department of Infectious Diseases, Pediatric Infectious Diseases, Phthisiology and Pulmonology, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

226 patients with pulmonary tuberculosis were examined, of whom 144 (64.1%) experienced adverse events (AE) from anti-tuberculosis drugs during treatment. All patients were tested for haptoglobin (Hp) phenotype carriers. Analysis of the obtained data showed that AEs occurred predominantly in patients carrying homozygous variants of haptoglobin Hp1-1 and Hp2-2. It is recommended to determine the haptoglobin phenotype to predict the risk of AE development from anti-tuberculosis drugs.
Keywords: Tuberculosis, Haptoglobin, Adverse events, Anti-tuberculosis drugs
Cite this paper: Tashpulatova Fatima Kudratovna, Adverse Effects of Anti-Tuberculosis Drugs in Patients with Pulmonary Tuberculosis Carrying Different Haptoglobin Phenotypes, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 675-677. doi: 10.5923/j.ajmms.20251503.40.
1. Relevance
- The current epidemiological situation regarding tuberculosis is characterized by changes in its pathomorphism - the emergence and increase in the number of severe, progressive forms of the disease, an increase in the frequency of polyresistant forms of MBT, and drug-induced complications from chemotherapy [9].Undoubtedly, social and economic shocks, environmental and radiation factors in the regions, the increase in HIV infection, drug addiction, irrational chemotherapy, high frequency of concomitant diseases such as viral hepatitis, CNSLE, diabetes mellitus, and gastrointestinal tract diseases played a major role in this.While acknowledging the social and hygienic aspects of tuberculosis, one should not forget about its biological characteristics, which may be the most important and at the same time insufficiently studied, which affect the body's reactivity [1]. Biological factors undoubtedly play a crucial role in the development of both the human disease itself and the course of the tuberculosis process and the effectiveness of the treatment being administered. Reflecting the characteristics of the body's response to external influences, reactivity allows for "passing the bridge" between biological and socio-hygienic factors in the development of tuberculosis [1].Important importance is given to assessing the individual reactivity of the organism from a genetic perspective [3,5]. It has been established that many normal and pathological reactions of the body are determined by genetic background, which determines the variation of physiological reactions in response to the action of the same factor. Consequently, it can be assumed that the difference in the formation of clinical variants of tuberculosis, the progression of the process, its complications, transition to a chronic form in some and complete recovery in others, along with other factors, is also explained by genetic features [1,8].The diversity of forms of pulmonary tuberculosis, the chronic nature and phased course of the disease, and the deep impression of the disease on the psychosomatic appearance of the patient indicate a significant influence of reactivity on the course of pulmonary tuberculosis and, at the same time, a change in the body's reactivity under the influence of the disease. All this prompted us to address the problem of reactivity in pulmonary tuberculosis.One of the genetic markers associated with the occurrence and course of tuberculosis is the haptoglobin (Hp) phenotype, with carriage of homozygous variants, a severe course and low treatment efficacy were noted [6,7,8]. However, we have not encountered any association between the carriage of haptoglobin phenotypes and the development of adverse effects from anti-tuberculosis drugs in the available literature.Purpose: To study the frequency and nature of adverse effects from anti-tuberculosis drugs in patients with pulmonary tuberculosis carrying different phenotypes of haptoglobin (Hp).
2. Material and Methods
- A comprehensive examination of 226 patients with pulmonary tuberculosis aged 17 to 65 who were undergoing treatment in the therapeutic departments of the Republican Ftiziatrics and Pulmonology Center and the city of Tashkent was conducted. Of the total number of examined, 111 (49.1%) were men and 115 (50.9%) were women.Among the clinical forms of tuberculosis, infiltrative pulmonary tuberculosis was most common - 134 (59.3%) and fibro-cavernous pulmonary tuberculosis - 30 (13.3%). The first-time identified patients were -85.8%.In 177 (77.8%) patients, concomitant diseases were identified: COPD - in 31.5%, anemia - in 18%, gastrointestinal tract and liver diseases - in 17%, diabetes mellitus - in 19.3%.Taking into account the results of the drug resistance test, the examined patients were prescribed, according to WHO standards, first-line anti-tuberculosis drugs - isoniazid, rifampicin, pirazinamide, and etambutol. The patients were hospitalized for 2 to 3 months.To identify the association between the frequency, nature, and characteristics of NA manifestation and the carriage of genetic markers, the haptoglobin (Hr) phenotype was determined by electrophoresis of the blood serum disc in a polyacrylamide gel according to the Davis method, modified by N.A. Osina (1982).
3. Results and Discussion
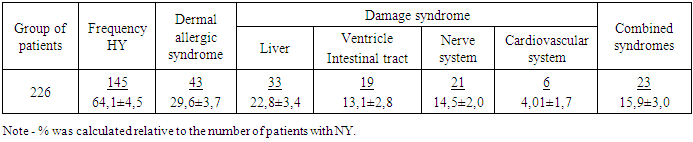
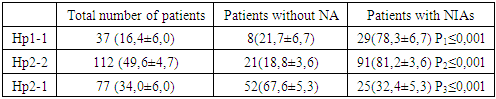
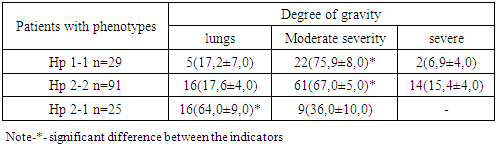
- During treatment, 144 (64.1%) patients developed TN due to anti-tuberculosis drugs (Table 1). In our work, we used the syndromic classification of adverse effects from anti-tuberculosis drugs.
|
|
|
4. Conclusions
- Thus, tuberculosis patients carrying homozygous variants of haptoglobin phenotypes Hp 1-1 and Hp 2-2 are predisposed to frequent development of adverse effects from anti-tuberculosis drugs, indicating the necessity of including haptoglobin phenotype determination in the battery of laboratory tests before initiating chemotherapy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML