-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 670-674
doi:10.5923/j.ajmms.20251503.39
Received: Feb. 17, 2025; Accepted: Mar. 3, 2025; Published: Mar. 13, 2025

Effectiveness of Local Ocular Applicators in the Treatment of Myopia and Accommodation Spasm
Fayzieva D. B.
Tashkent Military Medical Academy, Tashkent, Uzbekistan
Correspondence to: Fayzieva D. B., Tashkent Military Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Refractive disorders, including myopia, hypermetropia, and astigmatism, are among the most common eye conditions, affecting millions of people worldwide. These disorders can reduce vision quality and contribute to the development of other eye diseases. Timely identification and prevention of these disorders are crucial. Factors such as genetic predisposition, environmental influences, and lifestyle changes play a significant role in the development of refractive conditions. Myopia and accommodation spasm are especially prevalent among the youth and significantly impair vision and quality of life. These conditions have been on the rise in recent years, increasing their epidemiological and medical relevance. Existing treatment methods for myopia, such as glasses and contact lenses, do not stop the progression of the disease. This study evaluates the effectiveness of local eye applicators and alternative treatment methods for myopia. The results demonstrate that these methods contribute to improving visual acuity at different distances and help reduce symptoms of accommodation spasm. These new approaches are crucial in early diagnosis and treatment of myopia.
Keywords: Myopia, Accommodation spasm, Refraction, Prevention, Treatment, Diagnosis
Cite this paper: Fayzieva D. B., Effectiveness of Local Ocular Applicators in the Treatment of Myopia and Accommodation Spasm, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 670-674. doi: 10.5923/j.ajmms.20251503.39.
1. Introduction
- Refractive disorders are among the most common eye diseases, affecting millions of people worldwide. These disorders include conditions such as myopia, hyperopia, and astigmatism, which can lead to a decrease in visual quality and may also contribute to the development of other eye diseases. Timely detection and prevention of these disorders are crucial, as many of these conditions can develop with age or due to external negative factors [1].Identifying and analyzing the risk factors associated with refractive disorders is necessary for effective treatment and prevention [2,3]. These factors include genetic predisposition, environmental influences, and lifestyle changes. Additionally, modern diagnostic and treatment approaches can help prevent the further progression of these diseases.Today, new diagnostic and treatment methods are being developed in the fields of medicine and ophthalmology, aiming to reduce the prevalence of these diseases and improve patients' quality of life. In this regard, it is important to create a system capable of predicting the development of refractive disorders at an early stage and responding quickly to changes [4].Developing a system for predicting the risk factors of refractive disorders offers a new approach to the treatment and prevention of these diseases. A systematic approach, considering both individual and external factors, can significantly improve the effectiveness of prevention and treatment in the future [5]. This work is dedicated to the development of a system for predicting the risk factors of refractive disorders and providing methodological recommendations for researchers in this field.Myopia and accommodative spasm are among the most common eye conditions in modern ophthalmology. They not only complicate visual acuity but also significantly impact the patient's quality of life, causing headaches, eye strain, reduced performance, and general discomfort. The prevalence of these diseases continues to rise each year, making them relevant from both an epidemiological and medical perspective [6,7].Myopia (nearsightedness) remains the most common cause of visual impairment worldwide. According to the World Health Organization (WHO), myopia affects approximately 30% of the global population, and the number of cases continues to grow each year. The development of myopia, particularly among children and adolescents, significantly increases the risk of complications such as glaucoma, cataracts, and retinal detachment, making myopia an important issue in prevention and treatment [8]. In developed economies, myopia has increased significantly among youth and adolescents, which is associated with prolonged near-vision activities (reading, working on a computer) and insufficient outdoor physical activity. Current methods for treating myopia (correcting vision with glasses or contact lenses) do not stop the disease's progression and do not resolve issues with eye accommodation, creating a demand for new and effective approaches [2,7].Accommodative spasm is a condition where the muscles responsible for focusing the eye at different distances remain in a constant state of contraction. This can result from prolonged strain on the eye muscles, insufficient relaxation, and disruption of the accommodation process. Accommodative spasm is commonly seen in children, adolescents, and people who spend excessive time in front of computer or phone screens. This condition not only causes eye fatigue and discomfort but can also lead to worsening vision, accelerating the development of myopia [9].Diagnosing and treating accommodative disorders and myopia are key aspects of ophthalmological practice. A challenge in timely diagnosis is that many patients do not notice the symptoms related to accommodation disorders, and myopia often develops unnoticed at an early age. Therefore, early diagnosis and prevention are crucial to avoid disease progression. There are several methods available for correcting and treating visual impairment, including traditional methods (glasses and contact lenses) as well as innovative approaches aimed at improving accommodation, slowing myopia progression, and treating accommodative spasms, such as local eye applicators and alternative treatments [10].Prevention and treatment issues remain critical tasks. Modern recommendations include limiting screen time, taking regular breaks, and ensuring physical activity outdoors. However, effective treatment methods for accommodative spasm and myopia require further research. Specifically, the use of local applicators aimed at improving accommodation is a promising direction that could be applied in daily practice to improve patients' quality of life [11].Thus, myopia and accommodative spasm are serious issues that require a comprehensive approach to diagnosis, treatment, and prevention. Given the global increase in the prevalence of these conditions and their impact on quality of life, investigating new treatment and prevention methods, such as local applicators, is an important step toward improving visual health in the future.The goal of this study was to compare the effectiveness of local eye applicators and alternative treatments for myopia based on changes in visual acuity at different distances.
2. Materials and Methods
- In 2023-2024, data from individuals who underwent medical-expert commissions for eye health prophylactic measures among the sharpshooters of the Northern Military Unit were analyzed. The study was conducted on individuals with various ophthalmological conditions, including ophthalmologically healthy individuals (15 people), those with accommodative spasm or strabismus (23 people), and individuals with severe myopia (13 people).Visual acuity was assessed using the Sivtsev-Golovin chart, which determines the ability to distinguish objects of various sizes from a specified distance. The chart contains letters and symbols of various sizes, and the individual is asked to read them from the designated distance. Visual acuity is expressed as a "vision ratio" and is evaluated first monocularly and then binocularly. In monocular testing, one eye is covered with a special patch. The number of fingers counted or light sensitivity is also considered when determining visual acuity. This method is widely used in ophthalmology and is effective in detecting visual impairment [12,13].
3. Results and Discussion
- This study aimed to evaluate the changes in accommodation in patients receiving different treatment methods. Three groups were compared: the control group (healthy participants who did not receive treatment), the group receiving alternative treatment, and the group using local ocular applicators. The control group, consisting of healthy participants who did not undergo any treatment, showed no changes in accommodation, as the participants did not receive any intervention. The pre-treatment measurements for this group were 1.0±0.01 diopters for both eyes (right and left). These values served as the baseline for comparing changes in the other groups.Participants in the alternative treatment group had pre-treatment values of 0.54±0.01 diopters for the right eye and 0.61±0.02 diopters for the left eye. After the first month of treatment, a noticeable improvement was observed, with 63% improvement for the right eye and 54% for the left eye, corresponding to an improvement of 1.63 and 1.54 times, respectively. These changes confirm the effectiveness of the treatment, although the results continued to improve after two months: the right eye showed a 78% improvement, and the left eye showed 61%, which corresponds to an improvement of 1.78 and 1.61 times, respectively.However, the group using local ocular applicators demonstrated the greatest improvement. Before treatment, their measurements were 0.61±0.06 diopters for the right eye and 0.61±0.02 diopters for the left eye. After one month of using the applicators, the right eye showed a 49% improvement, and the left eye showed a 55% improvement, which corresponds to an improvement of 1.49 and 1.55 times, respectively. After two months, the results improved even further: the right eye showed a 61% improvement, and the left eye showed a 63% improvement, corresponding to 1.61 and 1.63 times, respectively. These results significantly surpass those of the alternative treatment group, both in terms of speed and overall treatment effectiveness (Figure 1).
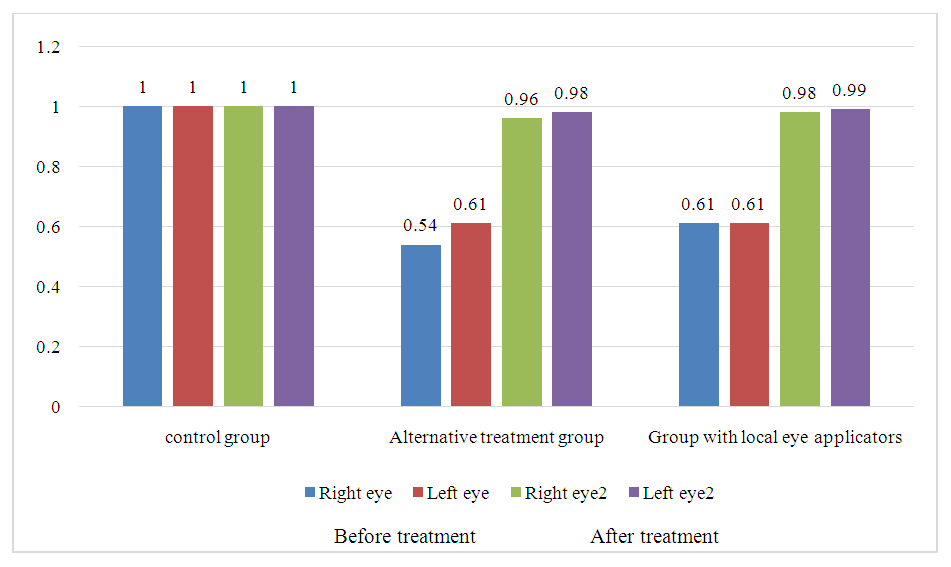 | Figure 1. Accommodation Changes Before and After Treatment in Different Groups According to Right and Left Eye Measurements |
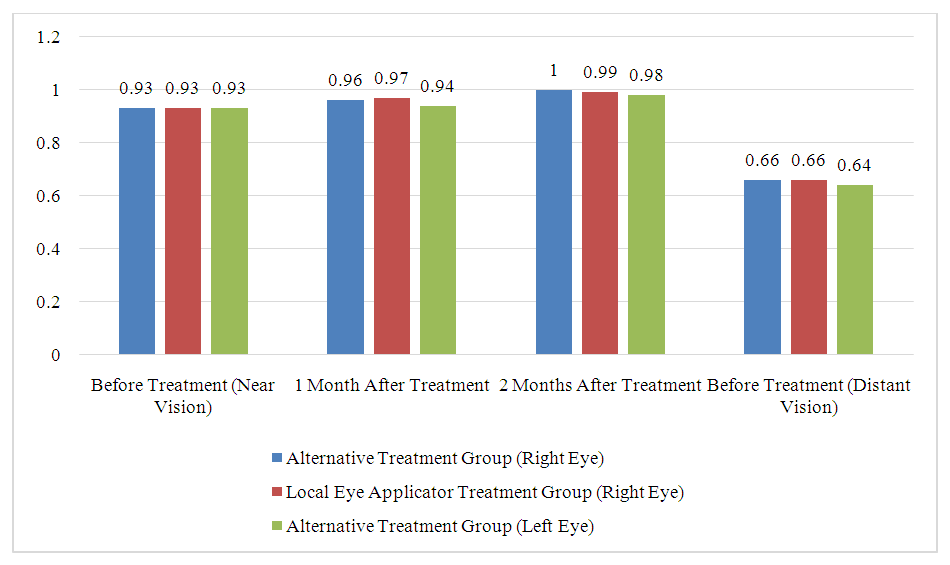 | Figure 2. Сomparative Results of Myopia Treatment in Different Groups |
4. Conclusions
- The study assessed the changes in accommodation in patients using different treatment methods for myopia. The comparison of three groups—control (healthy participants), alternative treatment, and local ocular applicators—revealed distinct differences in the outcomes.In the control group, no changes were observed, as no intervention was applied. This group served as the baseline for comparison.The alternative treatment group showed notable improvements in accommodation after one and two months of treatment. However, these changes were less pronounced compared to the local ocular applicator group. After one month, improvements were recorded for both eyes, but after two months, the alternative treatment group still had lower improvements than the group using local ocular applicators.The local ocular applicator group demonstrated the most significant and sustained improvements. After one month, this group showed a marked improvement in accommodation, and by the second month, their performance surpassed that of the alternative treatment group, with the right eye showing a 61% improvement and the left eye a 63% improvement. These results demonstrate the high effectiveness of local ocular applicators over time.In conclusion, local ocular applicators are a more effective method for treating accommodation disorders compared to alternative treatments. The results show that local ocular applicators provide faster and more significant improvements, both in the short and long term, making them a promising option for clinical use.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML