O. Z. Yangibaev
Tashkent Medical Academy, Toshkent, Uzbekistan
Correspondence to: O. Z. Yangibaev, Tashkent Medical Academy, Toshkent, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Today, laparoscopic cholecystectomy (LC) is widely used in the treatment of uncomplicated types of gallstone disease (UTGD), and the recovery rate of patients remains only around 75-85%. As a result, LC patients suffer from post-cholecystectomy syndromes of various forms (recurrence and residual choledocholithiasis, Vaters papilla stenosis (VPS), gallbladder biliary tract remnant - ductus syndrome, chronic biliary cholangitis-hepatitis, pancreatitis, diarrhea, etc.) up to 50% to repeated treatments and sometimes reoperations (up to 10-25%) are also in need. Up to 85-95% of reoperations after LCs in the biliary tract are performed due to relapse and residual choledocholithiasis, Vaters papilla stenosis, gallbladder remnant bile duct syndrome - ductus syndrome, etc. This indicates that there are some problems in the diagnosis of this disease. Namely, in the diagnosis of UTGD, when jaundice, choledocholithiasis, VPS and are not detected, the diameter of the hepaticocholedochus is within 6-8, and sometimes 9-10 mm, etc. Therefore, in such cases, since 2020, we have decided to use fibrocholangioscopy (with a diameter of 2.6 mm), through the cystic duct during LC, we used it in 416 patients, of which 36 (8,65%) were diagnosed with choledocholithiasis and VPS (this endoscope with an external diameter of 2.6 mm does not pass from the VP to the duodenum). In 22 of these patients, revealed small stones measuring 3-4 mm in size in the area of the Vaters papilla which were removed through the gallbladder ductus after cysticotomy-ductotomy (using a Dormia basket, vacuum suction, etc.), and In the 10 patients, due to the larger stones (6-10 mm in size), cystico-choledochotomy,and in the remaining 4 patients, even microlaparotomy and cysticocholedocholitotomy and PST were performed using our special papillotome to eliminate the VPS. Тhe operations were completed with choledochal cannulation through the gallbladder duct.
Keywords:
Сholelithiasis, Choledocholithiasis, Stenosis of the Vaters papilla, Choledochoscopy, Cholecystectomy, Choledocholithotomy, Papillosphincterotomy
Cite this paper: O. Z. Yangibaev, Some Causes and Prophylactic Factors of Postcholecystectomy Syndrome, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 666-669. doi: 10.5923/j.ajmms.20251503.38.
1. Introduction
Currently, laparoscopic cholecystectomy (LC) is recognized globally as the "gold standard" for treating uncomplicated gallstone disease (UCGD). Despite its established efficacy, the long-term recovery rate for patients following the procedure seems to plateau at around 75-85% [1,21,22,23,24,25,26,27,28,29,30,31]. This indicates that while laparoscopic cholecystectomy is largely successful, there are still some issues associated with the surgery that warrant attention. It's crucial for healthcare providers to remain vigilant about these potential issues and to communicate them effectively to patients to ensure informed decision-making.Particularly in the long-term period following laparoscopic cholecystectomy (LC), there has been an increase in the occurrence of various complications such as recurrent and residual choledocholithiasis (CDL), regarding Vaters papilla stenosis (VPS), “ductus” syndrome (due to residual or remnant cystic duct related issues), chronic cholangitis-hepatitis, pancreatitis, biliary hepatitis, diarrhoea, and others. These incidences of what is collectively referred to as 'post-cholecystectomy syndrome' (PCS) have been observed [1,2,3,5,8,9,11,15,17,18,19,20]. to rise notably in recent years (from 2015 to 2025). As a result, patients are often required to undergo repeated treatments with some needing reoperations in 10-25% of cases. Studies indicate that the rate of these reoperations in 85-90% cases primarily linked to recurrent or residual choledocholithiasis, VPS, “ductus” syndromes etc. [4,6,7,10,12,13,14,16]. This highlights the importance of thorough preoperative evaluation and postoperative follow-up to minimize these risks.If we consider the residual or recurrent nature of these complications, it indicates that there are indeed certain issues in both the diagnosis and treatment of so called “uncomplicated” gallstone disease (GSD). It's essential to recognize these challenges to improve patient outcomes. The purpose of the research work is focused on improving the treatment outcomes for patients diagnosed with UGSD. The objective of the research is to explore specific causes of the complications and shortcomings encountered in treating UGSD with LC. We will explore various strategies to address and mitigate these issues effectively.
2. Material and Methods
Between 2015 and 2025, we conducted a comprehensive objective diagnostic evaluation of 4,820 patients who underwent laparoscopic cholecystectomy (LC) for the diagnosis of uncomplicated gallstone disease (UGSD). Out of these, 420 patients experienced persistent symptoms following the procedure and these patients underwent various outpatient investigations (including clinical-laboratory tests, ultrasound diagnostics, gastroduodenoscopy, X-rays, CT, MRI, cholangiography, etc.).Out of total of 420 patients underwent evaluation, 362 were diagnosed with chronic gastrointestinal conditions, including chronic gastroduodenitis, hepatitis - hepatosis, pancreatitis, diarrhoea etc., and these patients were advised to undertake conservative treatment interventions. Notably, no severe pathological conditions requiring surgical intervention on the biliary tract were identified, such as significant dilation of the bile ducts, choledocholithiasis, or stenosis of papilla of Vater. This suggests that the conservative management strategies proposed are appropriate and warranted for this patient cohort.Remaining 116 patients with various forms of post-cholecystectomy syndrome (PCS) underwent various investigation, including ultrasonography, endoscopic retrograde cholangiopancreatography (ERCP), and magnetic resonance cholangiography (MRCP) (36 patients). In every instance, we observed notable dilation of both the intrahepatic and extrahepatic bile ducts, measuring over 15 mm. Out of these cases, 32 were determined to have choledocholithiasis, one presented with stenosis of the sphincter of Oddi, and 4 patients exhibited symptoms consistent with "ductus" syndrome. To ascertain the underlying aetiologies, the pathological processes documented during the initial laparoscopic cholecystectomy (LC) procedures of all 116 patients were meticulously analyzed.
3. Results and Discussion
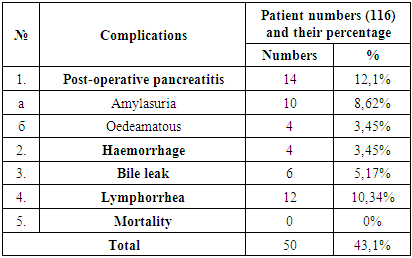
Suggests that LC is typically conducted on patients with UGSD only when there are no apparent clinical indicators of mechanical jaundice, hyperbilirubinemia, choledocholithiasis, or stenosis of the ampulla of Vater, either in the patient's medical history or during objective assessment. Furthermore, during the LC procedure, the diameter of the gallbladder duct and common bile ducts were measured, revealing no significant dilation, remaining within the range of 8-11 mm. This adherence to stringent clinical criteria underscores the necessity for thorough preoperative evaluation in ensuring patient safety and optimizing surgical outcomes.In this study, we present a comprehensive analysis of postoperative complications observed in a cohort of 116 patients classified within this specific category. The complications were systematically documented in the accompanying tables, detailing both the initial and long-term sequelae following surgical intervention.Table 1. Early complications following the initial LC in patients with PCS
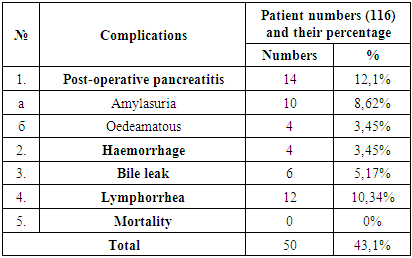 |
| |
|
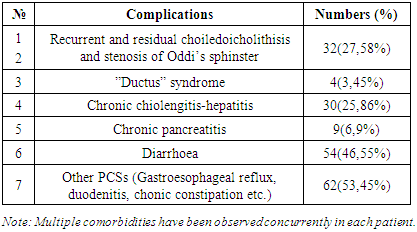
Table 2. Long term complications following the initial LC in patients with PCS
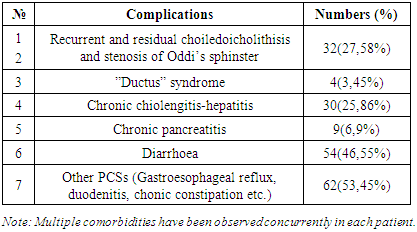 |
| |
|
To determine the causes of complications arising post-LC in patients with UGSD, we conducted an analysis of the pathological characteristics recorded in the operative notes.At the initial stage of LHEC, i.e. at the stage of diagnostic laparoscopy, significant hepatomegaly was observed in almost all patients, characterized by blunting of the edges of the liver and markedly dilated lymphatic capillaries on the surface of the liver in 48 cases, in addition, in 42 cases, widespread small yellowish areas measuring from 1 to 2 mm were noted, and in 72 cases, noticeable adhesions were observed between the liver and the diaphragm. The gallbladder demonstrated significant distention and wall thickening in 72 cases, while 44 cases exhibited wall thinning, permitting the visualization of calculi, and 24 cases indicated reticular cholesterosis within the lumen; additionally, in 52 instances, notable adhesions to adjacent structures, including the stomach, duodenum, jejunum, and colon, were observed, along with the enlargement of paravesical and paracholedochal lymph nodes in 56 cases, and morphological anomalies such as bulbous enlargement of Hartmann's pouch and two instances resembling an "hourglass" shape were also documented.Subsequently, considerable attention was paid to documenting the measurements of the diameter of the gallbladder duct and common bile duct in the protocols of the LC operation. Specifically, in 88 cases, the diameter of the common bile duct exhibited a range of 9-10 mm, 18 cases measured between 7-8 mm, and 10 cases ranged from 6-7 mm, and regarding the cystic duct, 90 cases demonstrated a diameter of 3-4 mm, 22 cases showed 2-2.5 mm, and 4 cases were noted to have diameters less than 2 mm.In a post-operative evaluation of 36 patients diagnosed with choledocholithiasis and stenosis of the papilla of Vater following LC, the majority (32 patients) presented with common bile duct diameters ranging from 9 to 10 mm, while only 4 patients demonstrated diameters of 7 to 8 mm; furthermore, the diameter of the cystic duct was consistently recorded at 3 to 4 mm across all examined patients.Therefore, we concluded that, starting in 2020, in all cases of USI, MRI cholangiography before LC, and especially during LC, when the hepaticocholedoch diameter is 7-8 mm or larger (around 9-10 mm), it is necessary to use a new ultrathin fiberoptic cholangioscopy (diameter 2.6 mm), and we used it in 416 patients (specifically those who were scheduled for LC according to the UCGD), of whom 38 had choledocholithiasis and VPS (this endoscope does not pass freely from the VP to the duodenum) and its normal function (that is, its normal rhythmic opening and closing during choledochoscopic examination) was not observed. In 22 of these patients, At the beginning of LHEC, a single clip was placed in the proximal part of the gallbladder duct (in the area of the beginning of the gallbladder), and in the distal part of it, a longitudinal microcysticotomy-ductotomy was performed. Тhrough this hole cholangioscopy was performed. During fibrocholangioscopy, small stones measuring 2-4 mm were detected in the area of the VP ampulla. These stones were removed through ductotomy using a Dormia basket, vacuum suction, etc., and then antegrade PST was performed using our special papillotome, eliminating VPS. In the remaining 8 patients, due to the fact that the stones were larger (6-10 mm in size), cysticoductotomy was expanded i.e., cysticoductocholedochotomy was performed, and in the remaining 4 patients after LC, microlaparotomy and cysticocholedochotomy were performed to remove the stones. Stones were removed and PST was performed, operations were completed by draining the choledoch through the remnants of the cystic duct. In the postoperative period, only 4 patients exhibited short-term amylasuria. The remaining patients experienced a smooth recovery, and all were discharged from the hospital in a satisfactory condition.
4. Conclusions
Contemporary use of ultra-thin fibro-cholangioscopes may play a critical role in significantly reducing the risk of post-cholecystectomy syndromes, including choledocholithiasis and VPS, following laparoscopic cholecystectomy for so called “uncomplicated” gallstone disease (UGSD).
References
| [1] | Danilov M.V., Aripova N.N., Zarubiani V.G. On the history of cooperation between academicians A.A. Vishnevsky and U.A. Aripov in the field of biliary-pancreatic system surgery // Bulletin of Emergency Medicine, 2018, Vol. 11, No. 4. P. 90–95. |
| [2] | Snigirev A.Yu., Alekseev N.A., Snigirev Yu.V., Baranov A.I. Assessment of the risk of acute post-manipulative pancreatitis during antegrade endoscopic papillosphincterotomy // “Medicine” V. 18. No. 2. 2019. P. 44–47. |
| [3] | Topchiev M.A. Complications of videolaparoscopic cholecystectomy // Abstracts of reports of the XVII Congress of the Russian Society of Endoscopic Surgeons. – Endoscopic surgery. – 2014. – No. 1. – P. 404-405. |
| [4] | Ali Zahedian, Sekineh Kamali Ahangar, Yasser Asghari. Post cholecystectomy syndrome need to redo laparoscopic completion surgery: A case report. // Int J Surg Case Rep. 2018. 42. P. 145–147. |
| [5] | Bader Hamza Shirah, Hamza Asaad Shirah, Syed Husham Zafar, Khalid B Albeladi. Clinical patterns of postcholecystectomy syndrome // Ann Hepatobiliary Pancreat Surg. 2018 Feb; Т. 22. №1. P. 52–57. |
| [6] | Binit Sureka, Amar Mukund. Review of imaging in post-laparoscopy cholecystectomy complications // Indian J Radiol Imaging. 2017 Oct-Dec; T.27. № 4. P. 470–481. |
| [7] | Daniel Mønsted Shabanzadeh. // The Symptomatic Outcomes of Cholecystectomy for Gallstones // J Clin Med. 2023 Mar; Т. 12. №5. 1897. |
| [8] | Divya Arora, Robin Kaushik, Ravinder Kaur, Atul Sachdev. // Post-cholecystectomy syndrome: A new look at an old problem // J Minim Access Surg. 2018 Jul-Sep; Т. 14. №3. p. 202–207. |
| [9] | Doina Georgescu, Alexandru Caraba, Ioana Ionita, Ana Lascu, Emil Florin Hut, Simona Dragan, Oana Elena Ancusa, Ioana Suceava, Daniel Lighezan. // Dyspepsia and Gut Microbiota in Female Patients with Postcholecystectomy Syndrome // Int J Womens Health. 2022; 14: p. 41–56. |
| [10] | Hongbeom Kim, In Woong Han, Jin Seok Heo, (47) Min Gu Oh, Chi Yeon Lim, Yoo Shin Choi, Seung Eun Lee. Postcholecystectomy syndrome: symptom clusters after laparoscopic cholecystectomy // Ann Surg Treat Res. 2018 Sep; Т. 95. № 3. Р. 135–140. |
| [11] | Noor LH Bekkali, Kofi W Oppong. (81) How to manage postcholecystectomy abdominal pain // Frontline Gastroenterol. 2021; Т.12. № 2. Р. 145–150. |
| [12] | Oliver Burckhardt, Sarah Peisl, Benoit Rouiller, Emilie Colinet, Bernhard Egger. Length of the Remnant Cystic Duct and Bile Duct Stone Recurrence: a Case‒Control Study // J Gastrointest Surg. 2023; Т.27. № 6. Р.1122–1129. |
| [13] | Rang-Lang Huang, Wen-Kai Huang, Xiang-Yi Xiao, Lin-Feng Ma, He-Zi-Rui Gu, Guo-Ping Yang. Diagnosis and treatment of post-cholecystectomy diarrhoea // World J Gastrointest Surg. 2023 Nov 27; Т.15. № 11. Р. 2398–2405. |
| [14] | Saket Kumar, Nishant Kurian, Rakesh Kumar Singh, Venkat Rao Chidipotu, Sanjay Kumar, Amarjit Kumar Raj, Manish Mandal. Surgical management of cystic duct stump calculi causing post-cholecystectomy syndrome: A prospective study // J Minim Access Surg. 2023 Apr-Jun; Т. 19. № 2. Р. 257–262. |
| [15] | Tami Moore, Manish Amin. Post-Cholecystectomy Syndrome // Clin Pract Cases Emerg Med. 2017 Nov; Т. 1. №4. Р. 446–447. |
| [16] | Wen-Lin Zhang, Rui Ji. Cystic duct stump stone removal by retrieval basket under direct visualization using a novel peroral choledochoscope // Endoscopy. 2023 Dec; Т.55. (Suppl. 1). Р. 100– 101. |
| [17] | Khamdamov I.B. Improving tactical approaches in the treatment of hernias of the anterior abdominal wall in women of fertile age // New day in medicine. Bukhara, 2022. -№ 10(48) - Р. 338-342. |
| [18] | Khamdamov I.B. Morphofunctional features of the abdominal press in women of reproductive age // New day in medicine. Bukhara, 2022. -№3(41) - Р. 223-227. |
| [19] | Khamdamova M.T., Akramova D. E. Genetic aspects of genital prolapse in women of reproductive age // New day in medicine. Bukhara, 2023. - No. 5 (55). - Р. 638-643. |
| [20] | Khamdamova M.T., Akramova D. E. Genetic aspects of genital prolapse in women of reproductive age // New day in medicine. Bukhara, 2023. - No. 5 (55). - Р. 638-643. |
| [21] | Khamdamova M.T., Teshaev Sh.Zh., Hikmatova M.F. Morphological changes of the thymus and spleen in renal failure in rats and correction with pomegranate seed oil // New day in medicine. Bukhara, 2024. - N. 3(65). - Р. 167-187. |
| [22] | Khamdamova M. T. The state of local immunity in background diseases of the cervix // Eurasian journal of medical and natural sciences Innovative Academy Research Support Center. Volume 3 Issue 1, January 2023 ISSN 2181-287X R. 171-175. |
| [23] | Khamdamova M.T., Khasanova M.T. Various mechanisms of pathogenesis of endometrial hyperplasia in postmenopausal women (literature review) // New day in medicine. Bukhara. 2023. - No. 8 (58). - Р. 103-107. |
| [24] | Khamdamova M.T. Reproductive Health of Women Using Copper-Containing Intrauterine Contraception // Eurasian Medical Research Periodical Volume 28 January 2024, ISSN: 2795-7624.www.geniusjournals.org P. 39-45. |
| [25] | Khamdamova M.T., Zhaloldinova M.M., Khamdamov I.B. The state of nitric oxide in blood serum in patients with cutaneous leishmaniasis // New day in medicine. Bukhara, 2023. - No. 5 (55). - Р. 638-643. |
| [26] | Khamdamova M.T., Zhaloldinova M.M., Khamdamov I.B. The value of ceruloplasmin and copper in blood serum in women wearing copper-containing intrauterine device // New day in medicine. Bukhara, 2023. - No. 6 (56). - Р. 2-7. |
| [27] | Khamdamov I.B. Improving tactical approaches in the treatment of hernias of the anterior abdominal wall in women of fertile age // New day in medicine. Bukhara, 2022. -№ 10(48) - Р. 338-342. |
| [28] | Khamdamov I.B. Morphofunctional features of the abdominal press in women of reproductive age // New day in medicine. Bukhara, 2022. -№3(41) - Р. 223-227. |
| [29] | Khamdamov А.B. The state of carbohydrate and lipid metabolism in obese patients after biliopancreatic bypass surgery // International conference on interdisciplinary science Volume 03, Issue 11, 2024. Р. 169-175. |
| [30] | Khamdamova M. T., Khasanova M.T. Genetic mechanisms of development of endometrial hyperplastic processes in women in menopacteric age // American Journal of Medicine and Medical Sciences 2025. - № 15(2): Р. 372-375. DOI: 10.5923/j.ajmms.20251502.22. |
| [31] | Khamdamov I.B. Advantages Of Laparoscopic Hernioplasty in Obesity Women of Fertile Age // Eurasian Medical Research Periodical Volume 28 January 2024, ISSN: 2795-7624. www.geniusjournals.org P. 33-38. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML