Urinov Muso Boltayevich, Mustafayev Muhammad Olim Ugli
Bukhara State Medical Institute, Uzbekistan
Correspondence to: Mustafayev Muhammad Olim Ugli, Bukhara State Medical Institute, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Introduction. Transient ischemic attack is an acute ischemic cerebrovascular accident that often precedes an ischemic stroke. The prevalence of transient ischemic attack is difficult to assess because many patients do not attach significant importance to transient short-term disorders and do not seek medical advice. Materials and methods. We analyzed the clinical characteristics of transient ischemic attacks in 96 patients with transient ischemic attack who were admitted to the Kashkadarya branch of the Scientific Center for Emergency Medical Care of the Republic. There were 61 women and 35 men among the subjects, their average age was 55±2.7 years, and there were 19 (19.8%) patients aged 18-44, 45 (46.9%) patients aged 45-59, and 32 (33.3%) patients aged 60-74. Results. All the admitted patients had a family vascular history. Characterizing the risk factors that caused the development of transient ischemic attack in the examined patients, it is necessary to identify atherosclerotic, hemodynamic, cardiogenic, vertebrogenic, and the negative effects of bad habits. Conclusions. Transient ischemic attacks have an etiopathogenetic diversity. The features of the clinical course of transient ischemic attack depend on the risk factor, the phylogenetic heterogeneity of the affected brain structures, and the timeliness and adequacy of the treatment.
Keywords:
Transient ischemic attack, Cerebral stroke, Diagnosis, Clinic, Prognosis
Cite this paper: Urinov Muso Boltayevich, Mustafayev Muhammad Olim Ugli, Features of Transient Ischemic Attacks, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 632-636. doi: 10.5923/j.ajmms.20251503.31.
1. Introduction
Transient ischemic attack (TIA) is an acute ischemic cerebrovascular accident that often precedes an ischemic stroke. The prevalence of TIA is difficult to assess because many patients do not attach significant importance to transient short-term disorders and do not seek medical advice. After undergoing a TIA, the risk of developing not only stroke, but also myocardial infarction and death from cardiovascular diseases increases. For example, in the age group from 60 to 74 years, the risk of stroke is 5-8% per year for people who have had TIA, and only 1% in the absence of TIA; within 5 years, 60% of people who have had TIA die from cardiovascular diseases [1]. Currently, timely diagnosis of TIA, determining the prognosis of possible stroke and other cardiovascular diseases, and patient management tactics after TIA are regarded as urgent problems of neurology [2-5]. In connection with the above, the aim of the study was to study the clinical manifestations of various variants of transient ischemic attacks.
2. Materials and Methods
We analyzed the clinical characteristics of transient ischemic attacks in 96 patients with TIA who were admitted to the Kashkadarya branch of the Scientific Center for Emergency Medical Care of the Republic. There were 61 women and 35 men among the subjects, their average age was 55±2.7 years, and there were 19 (19.8%) patients aged 18-44, 45 (46.9%) patients aged 45-59, and 32 (33.3%) patients aged 60-74.
3. Results
All the admitted patients had a family vascular history. Characterizing the risk factors that caused the development of TIA (Fig. 1) in the examined patients, it is necessary to identify atherosclerotic, hemodynamic, cardiogenic, vertebrogenic, and the negative effects of bad habits.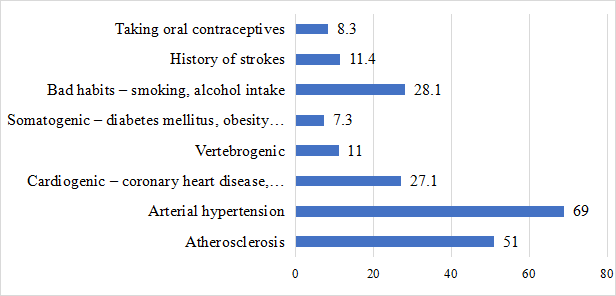 | Figure 1. TIA risk factors in the examined patients |
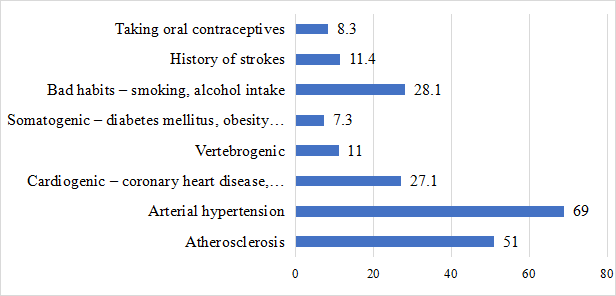
It should be noted that there is an aggravating vascular history in 87% of cases. 72 (75)% of patients with TIA developed in the vertebrobasilar vascular basin. These data coincide with the literature, according to which the ratio of TIA of the vertebrobasilar and carotid basins is 4:1, while in MI this ratio changes in favor of the carotid vascular basin and is 1:4 or 1:5 [6-8]. The focal neurological symptoms that occurred in patients with TIA were divided into symptoms of prolapse — paresis, hypesthesia, speech disorders, visual disturbances, ataxia and symptoms of irritation — paresthesia, twitching, hallucinations, photopsia. 61 (63.5%) patients had symptoms of irritation over symptoms of prolapse. The symptoms of ischemic attacks in the carotid basin revealed in patients generally corresponded to WHO criteria (Fig. 2). The most common neurological syndrome of carotid TIA was visual impairment (transient monocular blindness or decreased vision). They were usually characterized by decreased vision or complete loss on the side of the stenosed carotid artery, as well as episodes of a sudden feeling of "curtains" or "shutters" in front of the eyes.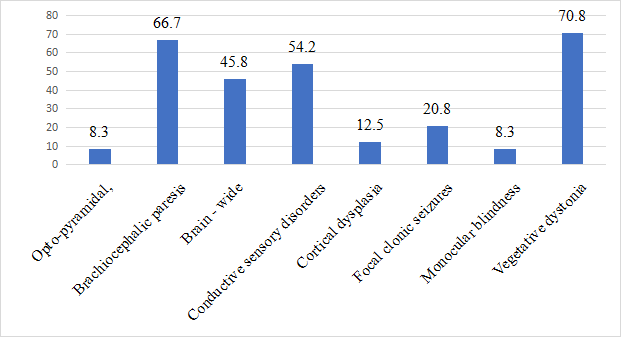 | Figure 2. Symptoms of carotid transient ischemic attacks |
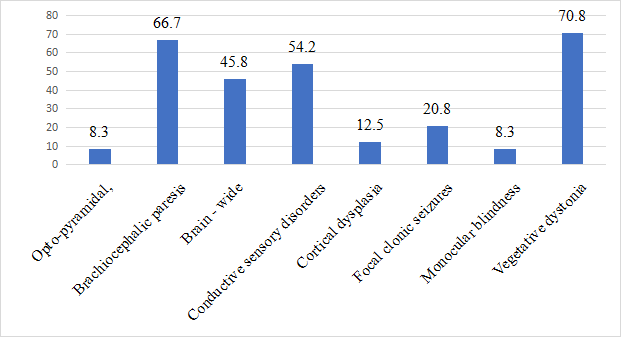
Along with visual disorders, motor disorders in the form of optic-pyramidal syndrome, brachiofacial paresis, and cortical dysphasia were not uncommon in our patients. Significantly less frequently, TIA occurred with paroxysmal states in the form of short-term, lasting several minutes, focal clonic seizures in the extremities, and contralateral artery stenosis. In the structure of clinical symptoms characterizing transient ischemic attacks of the vertebrobasilar basin, the leading ones were vestibulocochlear disorders, which manifested themselves as systemic or non-systemic dizziness, sometimes combined with hearing loss or noise in the ear, shakiness, and moderate ataxia (Fig. 3). Vegetative disorders were also common, more often of a paroxysmal nature, in the form of syncopal states, vestibulovegetative crises, cerebral phenomena, motor disorders that manifested themselves as tetra- or hemitype pyramidal insufficiency, diplopia, moderate dysarthria, choking, and sometimes hiccups. Transient global amnesia, flickering, or photopsies from both sides were less common.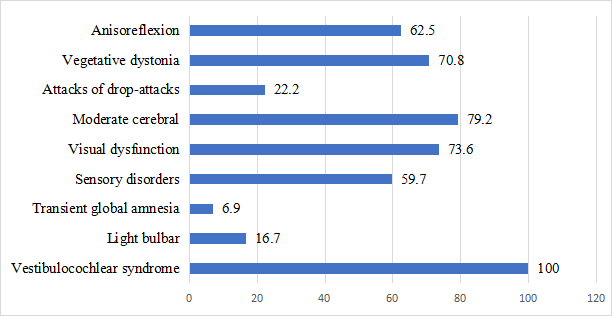 | Figure 3. Symptoms of transient ischemic attacks in the vertebrobasilar basin |
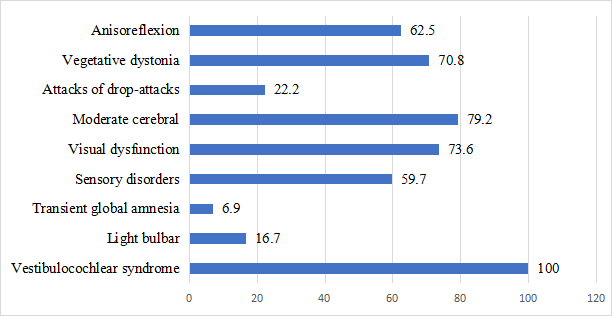
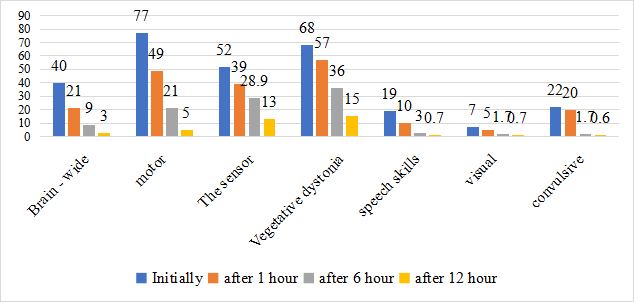
It was noted that often the provoking moments for the occurrence of stem symptoms in patients with TIA were a sharp turn or tilting of the head. Such situations are usually characteristic of disorders of cerebral circulation caused by stenosis of the vertebral arteries, combined with severe cervical osteochondrosis. Usually, such TIAs were accompanied by a sudden fall without loss of consciousness, seizures, and enuresis, and were diagnosed as drop attacks. In the development of these conditions, it can be assumed that there is a connection with transient ischemia of the reticular formation and the subsequent shutdown of postural tone. In one patient, nocturnal stem TIAs were triggered by snoring. Ischemia of the mediobasal areas of the temporal lobes, which was observed in 6 subjects, was accompanied by the development of global amnesia — loss of memory for events that took place over a certain period of time. During this period, patients were not fully adequate, lost their plan of behavior, and vaguely expressed their thoughts. The vegetative-vascular disorders observed in patients were characterized by fluctuations in blood pressure, hyperhidrosis, hyperthermia, and vestibulovegetative paroxysms. Disorders of the atactic motor sphere are often combined with spontaneity and disorders of muscle tone, vestibular dysfunctions [9-10]. Results and discussion. The sequence of regression of focal neurological disorders and their duration over time in patients with carotid TIA is of interest. At an earlier time (1-3 hours), speech was restored, brachiofacial paresis and cerebral symptoms disappeared. By the end of the first day, sensory and autonomic disorders were leveled (after 18-24 hours) (Figure 4).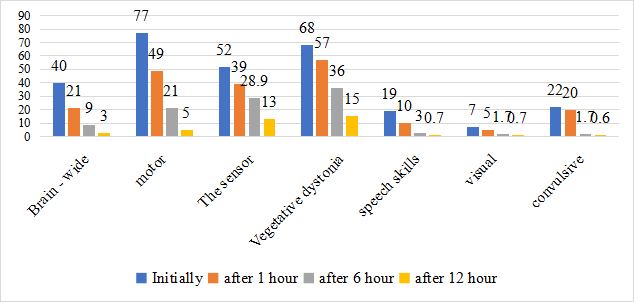 | Figure 4. Dynamics of recovery of neurological disorders in patients with TIA of the carotid basin |
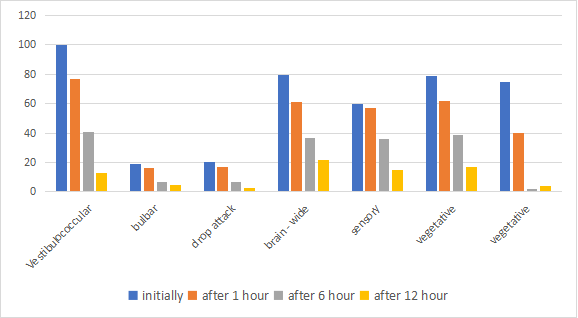
The dynamics of recovery of neurological disorders in patients with vertebrobasilar TIA was characterized by earlier leveling of motor, cochlear, and visual disorders (after 1-4 hours) and later — vestibular, autonomic, and sensory disorders (up to 24 hours) (Figure 5).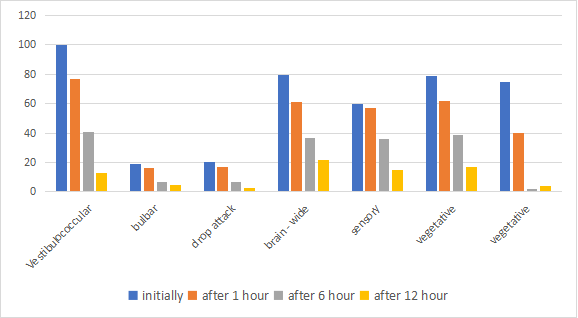 | Figure 5. Dynamics of recovery of neurological disorders in patients with TIA of the vertebrobasilar basin |
Describing the overall sequence of recovery of pathological neurological symptoms in patients with TIA in both vascular basins, it should be noted that symptoms of irritation and motor disorders regress earlier, while changes in the sensory analyzer turn out to be more persistent. The prognosis for TIA is a very complex, multifaceted and insufficiently studied problem. To date, it is unclear why TIAs of the vertebrobasilar basin occur 4 times more often than those of the carotid basin, and the number of carotid infarcts is as many times higher than the number of stem infarcts. The following explanation is very convincing: vertebrobasilar ischemia develops in very small stem structures and is accompanied by more pronounced symptoms compared to subclinical manifestations of carotid TIA. Therefore, patients with stem ischemia go to the doctor earlier and are treated more actively. In turn, it is known that brain infarction is often more severe in patients who have not had TIA compared to patients who have had them. In the patients we examined who underwent TIA, neurological symptoms regressed completely in absolutely all cases. The timing of its disappearance varied in the time range as follows: within the first hour of the development of TIA, neurological disorders disappeared in only 5 patients (5.2%), after 3 hours — in 22 people (22.9%), after 6 hours — in 32 patients (33.3%), that is, in most of the examined neurological disorders The symptoms persisted for up to 6 hours. Thus, in the TIA clinic there are mild, moderate and severe degrees of severity of the clinical course, the knowledge of which can be successfully used in predicting the possible transformation of TIA into cerebral strokes. Observations of our patients allowed us to establish different outcomes of TIA. Recovery was observed in 81 patients (84.4%), transformation of TIA into cerebral infarction occurred in 7 patients (7.3%), repeated TIA was observed in 8 cases (8.3%). The dependence of the TIA clinic on the etiological factor has been established. Risk factors and their combination, such as atherosclerosis and cervical osteochondrosis or atherosclerosis and hypertension, corresponded to the predominant localization of TIA in the vertebrobasilar basin, and the combination of cerebral atherosclerosis with cardiogenic factors or cerebral atherosclerosis with diabetes mellitus contributed to a more frequent lesion of the carotid basin. Taking into account the etiopathogenetic heterogeneity of TIA, appropriate therapeutic measures should be carried out, taking into account the most likely vector of development of the pathological process according to atherothrombotic, cardioembolic, vertebrogenic or hypertensive type. In this regard, there is a need to develop algorithms for various treatment options depending on the etiopathogenetic heterogeneity of transient ischemic attacks.
4. Conclusions
Transient ischemic attacks have an etiopathogenetic diversity. The features of the clinical course of TIA depend on the risk factor, the phylogenetic heterogeneity of the affected brain structures, and the timeliness and adequacy of the treatment. Prognostically unfavorable factors for the transformation of TIA into MI are old age, a combination of risk factors such as hypertension, cardiogenic factor, diabetes mellitus, duration of neurological symptoms of more than 1 hour and predominantly carotid localization of the affected vascular basin.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest. The authors have no conflicts of interest.
References
| [1] | Differential diagnosis of nervous diseases / Edited by G.A. Akimov and M.M. Odinak. Moscow: Hippocrates, 2001. pp. 415-439. |
| [2] | Voloshin P.V., Mishchenko T.S. Prevention of cerebral stroke // Health Ukraine. - 2012. - No. 5. - S. 14. |
| [3] | Diseases of the nervous system (a guide for doctors) / Edited by N.N. Yakhno, Moscow: Medicine, 2005, vol. 1. |
| [4] | Vinichuk S.M. Strategy for the treatment of cerebral stroke in the first hours and days after its development // Journal of Practice. the doctor. - 2008. -No. 5. - S. 4. |
| [5] | Vibers D.O., Feygin V.L., Brown R.D. Handbook of cerebrovascular diseases: Translated from English. - M.: 2009. - 672 p. |
| [6] | Vereshchagin N.V., Suslina Z.A., Piradov M.A. Principles of diagnosis and treatment of patients with acute cerebrovascular accident. Moscow: 2010. 320 p. |
| [7] | Mastykin A.S., Drivotinov B.V., Apanel E.N. Heterogeneity of the nosological concept of transient ischemic attack // Belarusian Medical Journal, 2014, No. 4, pp. 18-21. |
| [8] | Suslina Z.A., Vereshchagin N.V., Piradov M.A. Subtypes of ischemic disorders of cerebral circulation: diagnosis and treatment // Consilium Medicum. - 2011. - Vol. 3. - No. 5. - pp. 26-26. |
| [9] | Whisnant Y.P., Cartidge N. E., Elveback L.R. Carotid and vertical basilar transient ischemic attacks effect of anticoagulants hypertension and cardiac disorders on survival and stroke occurrence a population study // Ann. Neurol. - 2008. - Vol. 3, No. 2. - pp. 107-115. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML