-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 611-614
doi:10.5923/j.ajmms.20251503.26
Received: Jan. 2, 2025; Accepted: Feb. 1, 2025; Published: Mar. 10, 2025

Rare Malformations Identified During Prenatal Screening
Abdullayeva Gulrux Baxtiyorovna1, Akhmedova Shirin Nusratovna1, 2, Fаrаjov Azar Tofikovich3, Kamalidinova Shaxnoza Maxmudxanovna1, 4, Bahramova Nigina Alisherovna1, Abdullayev Baxtiyor Saidovich5
1Center for the Development of Professional Qualifications of Medical Workers
2Israeli Medical Center
3Oksigen Klinik Azerbaycan
4Republican Center for Mother and Child Screening Center Uzbekistan
5Samarkand State Medical University, Uzbekistan
Correspondence to: Abdullayev Baxtiyor Saidovich, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction. Today, great attention is paid to the fetal venous system in connection with the study of not only the ductus venosus, which is part of the ultrasound screening of the first trimester and plays an important role in the fetal circulation, since it allows oxygenated placental blood to bypass the liver and ensures preferential blood flow through the right atrium and oval window into the left atrium but also of interest in normal umbilical blood flow by participating in the development of the intrahepatic portal venous system. Objective. To evaluate the prenatal diagnosis and prognosis of ductal venous agenesis (DVA), umbilical varices and persistent superior vena cava and describe the outcome of this case. Methods. Systematic color Doppler ultrasound of the intrahepatic venous system, including the DV and portal system, was offered to all pregnant women in the first and second trimesters of pregnancy. Scanning of the fetal veins was carried out simultaneously with a routine ultrasound. Results. This case, 39-year-old pregnant woman, 4th pregnancy, scanned at 25 + 3 weeks, the scan revealed a combined change in the fetal venous system, umbilical varices, agenesis of the ductus venosus and PLSVC. The diagnosis was made on four main images: a three-vessel view and a tracheal view, where four vessels could be seen instead of three: 4CV wall of the left atrium with a dilated coronary sinus. Varicose veins of the umbilical cord were observed in the intra-abdominal section of the umbilical vein and direct communication was observed between the umbilical vein and the right atrium, bypassing the hepatic circulation, a typical ultrasound picture was observed - against the background of cardiomegaly, there was no connection between the umbilical vein and the portal vein, the connection of the umbilical vein with the right atrium was visualized. Taking these changes into account, karyotyping was recommended and performed with normal results. Conclusions. Thus, agenesis of the ductus venosus is a rare anomaly that can accompany various malformations and also be an isolated finding. If this pathology is detected, not only should all organs and systems of the fetus be thoroughly examined, but also prenatal karyotyping should be performed. With multiple developmental anomalies, the prognosis is determined by the severity of the combined changes. In the absence of other defects, the postnatal prognosis for agenesis of the ductus venosus can be considered favorable.
Keywords: Ductus venosus, Fetal veins, Malformations, Prenatal screening
Cite this paper: Abdullayeva Gulrux Baxtiyorovna, Akhmedova Shirin Nusratovna, Fаrаjov Azar Tofikovich, Kamalidinova Shaxnoza Maxmudxanovna, Bahramova Nigina Alisherovna, Abdullayev Baxtiyor Saidovich, Rare Malformations Identified During Prenatal Screening, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 611-614. doi: 10.5923/j.ajmms.20251503.26.
1. Introduction
- Today, great attention is paid to the fetal venous system in connection with the study of not only the ductus venosus, which is part of the ultrasound screening of the first trimester and plays an important role in the fetal circulation, since it allows oxygenated placental blood to bypass the liver and ensures preferential blood flow through the right atrium and oval window into the left atrium but also of interest in normal umbilical blood flow by participating in the development of the intrahepatic portal venous system [1,2,8,11]. Critical anastomoses with agenesis of the ductus venosus and shunting of umbilical cord blood directly into the right atrium are rare. In addition, more than 22% of patients have concomitant congenital heart defects. Two main types of ADV have been described depending on the course and connection of the umbilical vein (UV): intra- and extrahepatic [3,4,12,20]. Assessment of the umbilical portal venous system (UPVS) has become an important part of antenatal fetal assessment. UPVC abnormalities associated with chromosomal and structural abnormalities, Doppler assessment of ductus venosus flow has become a screening tool for Down syndrome in the first trimester of pregnancy. In addition, recent studies have shown the need to assess hepatic blood flow in fetuses with intrauterine growth restriction. In the fetus, venous blood flow in the liver is unique, as it is provided by two embryonic and functionally different systems: the umbilical and portal/vitelline systems [1,2,7,14]. From 5 to 10 weeks of pregnancy, a network of anastomoses is formed in the liver between the umbilical and vitelline systems, and the volume of placental blood flow increases, which then flows to the heart through this hepatic system. The intra- and extra portal venous system develops from the right vitelline vein. In the umbilical system, the right umbilical vein regresses, and the portal system directly develops from the left umbilical vein [1,2,12,14,16,18]. Varicose veins of the umbilical vein can be observed in any part of it. Research in color flow mode Allows you to determine the intense flow in cyst originating in the umbilical cord vein. In addition to ectasia of the vein in the area of the umbilical cord located in the waters, possible varicose veins of the intra-abdominal vein of the umbilical cord. Differential diagnosis in these cases usually occur with urachus cyst and cyst ovary based on the results of a Doppler study. Clinical significance of varicose veins umbilical cords have not yet been identified, although in some messages there was an opportunity its negative result for the fetus. In the work of P. Rank et al. [13,16,17,18].Persistent left superior vena cava (PLSV) is a congenital cardiac anomaly occurring in 0.3–0.5% of the general population and may be associated with congenital heart defects in 8% of cases. Prenatal identification of PLSVC is important for extensive cardiac and extracardiac evaluation of the fetus. We retrospectively re-evaluated abnormality scans performed in our department at 2-year intervals according to national guidelines to assess the incidence of PLSVC and its association with prenatal morbidity. In our population, the incidence of PLSVC was 0.31%, and we found a low association with cardiac and noncardiac anomalies. Standard views (three-vessel and tracheal view, four-chamber view, and outflow tract view) are not sufficient to rule out cardiac abnormalities when PLSVC is detected. Prenatal diagnosis of PLSVC may raise counseling issues; therefore, it is important to recognize the good outcome in an isolated case and the need for extensive workup to rule out other abnormalities [5,9,16,17,21].
2. Objective
- To evaluate the prenatal diagnosis and prognosis of ductal venous agenesis (DVA), umbilical varices and persistent superior vena cava and describe the outcome of this case.
3. Materials and Methods
- The ultrasound scans were performed according to the National Protocols approved by the Ministry of Health during the second (20–23 weeks) and the third trimester (and 30–32 weeks) by two fetal medicine certified specialists, using equipment with a probe of 3.5 MHz. The patients were informed about the scans prior to examination and provided consent for examination and medical data use for research and teaching purpose. Standard sections of the heart obtained from all patients included: thoracal transverse sections in 4-chamber view, three-vessel and trachea view (TTVV) and images of the left and right outflow tract. Systematic color Doppler ultrasound of the intrahepatic venous system, including the DV and portal system, was offered to all pregnant women in the second trimesters of pregnancy. Scanning of the fetal veins was carried out simultaneously with a routine ultrasound.The PLSVC is diagnosed in three main sections: 3-vessel view, where a small additional vessel is found at the main pulmonary artery (MPA) left, 4-chamber view (4 CV), where the PLSVC is detected as a round shape adjacent to the wall of the left atrium and a dilated coronary sinus is present, and in a sagittal view that shows the “pipe”-like aspect of the PLSVC. Whenever a suspect image is found, an extracardiac detailed scan is also performed. Images and clips are stored for further examination and as a proof if required. The cardiac images were reviewed, and for the cases with PLSVC, we retrieved from the patients file the following data: mothers’ age, pregnancy age, parity, history of previous congenital anomalies, cardiac or extracardiac associated anomalies, pregnancy and fetal outcome, age and type of delivery, neonate outcome.
4. Results
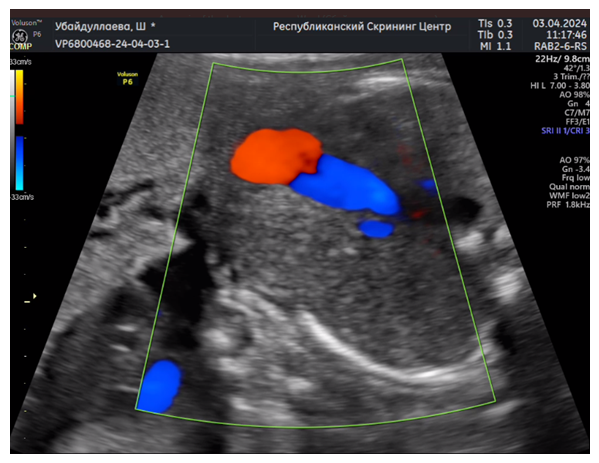
- This case, 39-year-old pregnant woman, 4th pregnancy, scanned at 25 + 3 weeks, the scan revealed a combined change in the fetal venous system, umbilical varices, agenesis of the ductus venosus and PLSVC. The diagnosis was made on four main images: a three-vessel view and a tracheal view, where four vessels could be seen instead of three: 4CV wall of the left atrium with a dilated coronary sinus. Varicose veins of the umbilical cord were observed in the intra-abdominal section of the umbilical vein and direct communication was observed between the umbilical vein and the right atrium, bypassing the hepatic circulation, a typical ultrasound picture was observed - against the background of cardiomegaly, there was no connection between the umbilical vein and the portal vein, the connection of the umbilical vein with the right atrium was visualized. Taking these changes into account, karyotyping was recommended and performed with normal results. Thus, agenesis of the ductus venosus is a rare anomaly that can accompany various malformations and also be an isolated finding. If this pathology is detected, not only should all organs and systems of the fetus be thoroughly examined, but also prenatal karyotyping should be performed. With multiple developmental anomalies, the prognosis is determined by the severity of the combined changes. In the absence of other defects, the postnatal prognosis for agenesis of the ductus venosus can be considered favorable. In this case, given the direct course of the umbilical cord vein into the right atrium, it caused a complication, heart failure developed, intrauterine fetal death was observed at 32 weeks of pregnancy.
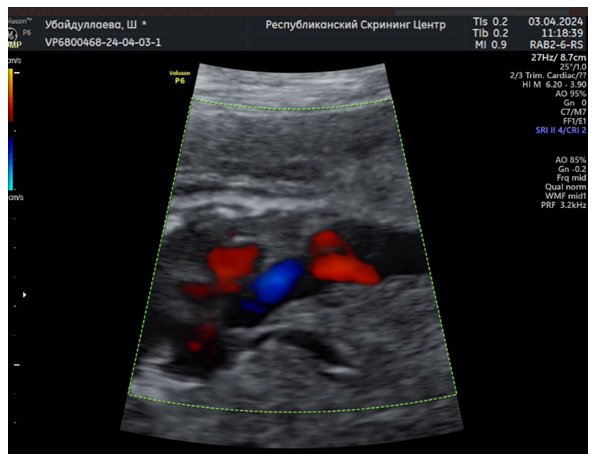 | Figure 1. direct communication between the umbilical vein and the right atrium, bypassing the hepatic circulation |
 | Figure 2. Direct communication between the umbilical vein and the right atrium, bypassing the hepatic circulation (coronary sinus) |
 | Figure 3. Varicose veins of the umbilical cord |
 | Figure 4. PLSVC |
5. Conclusions
- Assessment of the umbilical-portal venous system (UPVS), i.e., umbilical cord, ductus venosus, has become an important part of the antenatal examination of the fetus. It should be noted that pathology the condition of the umbilical cord is extremely diverse. Part of which are associated with an increase in the ability of congenital malformation, chromosomal abnormalities in the fetus, perinatal changes, and, in a number of cases and perinatal losses. Diagnosis of almost all pathological conditions of the umbilical cord is actually possible in the antenatal period thanks to the capabilities of modern echography. Enabling mandatory carefully evaluate the condition of the umbilical cord and ductus venosus in the protocols screening echography of the first and second trimesters will allow level of decline in perinatal mortality, as well as early neonatal morbidity. Prenatal diagnosis of PLSVC is feasible and relatively easy if standard protocols are respected at the time of a second-trimester anomaly scan. Once a suspicion of PLSVC is raised, an extended examination of the fetal heart is mandatory. Coronary sinus and innominate vein are clue markers in order to rule out some rare conditions such as the absence of RSVC or TPVRA. Isolated PLSVC has no significant consequences in utero and in infancy, but its presence can require further cardiac surgery. DV anomalies were found at a higher than reported frequency in scanned population. This associated anomaly was a rare pathology of the venous system. We believe that the diagnosis of ADV should automatically lead to the assessment of PVS, since portal anomalies represent an important outcome, predictor of ADV cases. PLSVC is highly correlated with extrahepatic umbilical bypass and is associated with poor outcome independent of genetic and morphological associations.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest. The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML