-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 591-593
doi:10.5923/j.ajmms.20251503.22
Received: Feb. 1, 2025; Accepted: Feb. 22, 2025; Published: Mar. 8, 2025

Clinical-Functional and Immunological Changes in Oral Organs During Prosthetics with Zirconia and Metal-Ceramic Bridge Prostheses
Akhmedov Xurshid Kamalovich
Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Akhmedov Xurshid Kamalovich, Bukhara State Medical Institute, Bukhara, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Clinical-functional and immunological changes in the oral cavity during prosthetics with zirconia and metal-ceramic bridge prostheses were studied. A study of 160 patients was conducted, divided into groups based on the type of prosthesis and the condition of the periodontal tissues. Patients with mild periodontitis demonstrated an increased frequency of symptoms such as tooth mobility (33.9% and 35.5%), gum bleeding (25.2% and 37.7%), and impaired chewing function. Microbiological analysis revealed an elevated concentration of Porphyromonas gingivalis and Fusobacterium nucleatum in groups with periodontitis, correlating with levels of inflammatory markers. Immunological studies recorded increased levels of sIgA (up to 201.5 mg/L), IL-6 (18.3 pg/mL), and IL-10 (22.2 pg/mL) in periodontitis groups. The obtained data indicate significant clinical and immunological differences between the groups, emphasizing the importance of accounting for inflammatory changes when selecting prosthetic treatment strategies.
Keywords: Bridge prostheses, Zirconia, Metal-ceramic, Clinical-functional changes, Immunological markers, Periodontitis, Microbiota, sIgA, IL-6, IL-10, Prosthetics
Cite this paper: Akhmedov Xurshid Kamalovich, Clinical-Functional and Immunological Changes in Oral Organs During Prosthetics with Zirconia and Metal-Ceramic Bridge Prostheses, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 591-593. doi: 10.5923/j.ajmms.20251503.22.
Article Outline
1. Introduction
- Clinical, functional and immunological changes occurring in the oral cavity during prosthetics are important aspects of orthopedic dentistry. The choice of bridge material, such as zirconium and metal ceramics, has a direct impact on the condition of oral tissues, microbial composition and immunological parameters. In the conditions of existing periodontal pathologies, these changes acquire additional significance for predicting treatment outcomes. Patients with periodontitis demonstrate an increased level of pathogenic microflora and activation of inflammatory processes, which leads to deterioration of clinical parameters and an increase in the frequency of repeated prosthetics. Immunological parameters, including the levels of secretory immunoglobulin A (sIgA), interleukin-6 (IL-6) and interleukin-10 (IL-10), reflect the degree of the inflammatory process and the adaptive response of oral tissues to the installation of orthopedic structures. Zirconium and metal-ceramic bridges, despite their clinical advantages, cause different reactions from tissues and the immune system, requiring a comprehensive assessment.The aim of this study is a comparative analysis of clinical, functional and immunological changes in patients who received zirconium and metal-ceramic bridges, taking into account the state of the periodontium. The study is aimed at identifying the relationships between the type of prosthesis, tissue condition and immune response, which will improve the effectiveness of orthopedic treatment.
2. Literature Review
- Prosthetic restoration with metal-ceramic and zirconium bridges occupies a central place in modern dentistry, ensuring the restoration of functionality and aesthetics of the dentition. Clinical studies demonstrate differences in the impact of these materials on oral tissues and immune mechanisms [1]. Metal-ceramics are characterized by high strength, but their metal framework can cause changes in periodontal tissues, including inflammatory reactions and disruption of the microbial ecosystem [2]. Zirconium, on the contrary, has a more pronounced biocompatibility due to its inertness. Studies have recorded a lower frequency of inflammatory changes in peri-implant tissues and a lower level of microbial load when using zirconium prostheses [3]. In addition, zirconium structures help reduce the level of proinflammatory cytokines, which confirms their positive effect on the local immune status [4].Immunological aspects play a key role in assessing the quality of prostheses. The effect of metal ceramics is associated with the activation of proinflammatory reactions, which can contribute to the development of periodontal diseases [5]. Zirconium, in turn, demonstrates a neutral effect on immunological parameters, maintaining the stability of the cytokine profile [6].The research results emphasize the importance of choosing the prosthesis material depending on the condition of the oral tissues and the individual characteristics of the patient. Zirconium bridge structures, due to their biocompatibility and stability, are a more preferable choice for patients with a predisposition to inflammatory processes.
3. Materials and Methods
- The study was performed based on the analysis of data from 160 patients aged 25 to 55 years. Patients were divided into two main groups depending on the material used for the bridge prostheses. The first group included 115 patients with metal-ceramic prostheses, the second group - 45 patients with zirconium prostheses. Each group was divided into subgroups "A" and "B" to study the differences depending on the periodontal condition. Subgroup "A" included patients without periodontal pathologies, subgroup "B" included patients with mild periodontitis. The control group consisted of 30 patients without periodontal pathology and prosthetic experience.The clinical examination included assessment of complaints, collection of anamnesis, examination of soft tissues of the oral cavity and analysis of the condition of the dentition. The following indicators were used: PMA index for assessment of gingival inflammation, CPITN index for characterization of periodontal condition, depth of periodontal pockets, Russell index and Green-Vermillion hygiene index for determination of the level of oral hygiene.For microbiological examination, oral fluid samples collected from periodontal pockets under sterile conditions were used. Samples were cultured on blood agar, Sabouraud agar and other media to detect aerobic and anaerobic microorganisms. Qualitative and quantitative analysis included counting colony-forming units (Porphyromonas gingivalis, Fusobacterium nucleatum, Candida albicans).Immunological examination was conducted by enzyme immunoassay. The levels of secretory immunoglobulin A (sIgA), interleukin-6 (IL-6), interleukin-10 (IL-10) and procalcitonin were determined in the patients’ saliva using automated laboratory systems with validated results.Descriptive and analytical statistics methods were used for statistical processing. The normality of data distribution was tested using the Shapiro-Wilk criterion. Comparative analysis between groups was performed using the Student t-test and the Mann-Whitney U-test. Correlation relationships between clinical, microbiological and immunological parameters were assessed using the Pearson method. All differences were considered statistically significant at p<0.05.
4. Results and Discussion
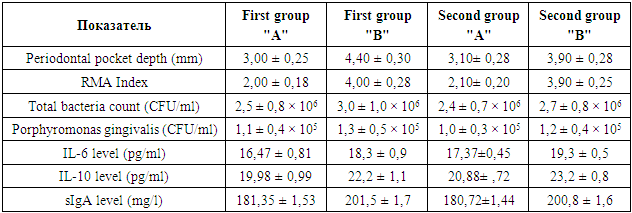
- The conducted study allowed us to analyze clinical, functional and immunological changes in the oral cavity organs in patients who underwent prosthetics with zirconium and metal-ceramic bridge structures. The study involved 160 patients, divided into groups depending on the material used and the state of the periodontal tissues. For an objective assessment, the depth of periodontal pockets, microbial load indicators and the level of inflammatory markers were studied. Clinical assessment showed that the depth of periodontal pockets in patients with mild periodontitis (subgroup "B") was 4.40 ± 0.30 mm in the first group and 3.90 ± 0.28 mm in the second group, which indicates a lower inflammatory response in patients with zirconium prostheses. In subgroups "A" (without periodontal pathologies), this indicator was stable and was within the physiological values.Microbiological analysis revealed an increase in the concentration of pathogenic microorganisms, including Porphyromonas gingivalis and Fusobacterium nucleatum, in subgroup "B". The level of Porphyromonas gingivalis in the first group was 1.3 ± 0.5 × 105 CFU/ml, in the second group - 1.2 ± 0.4 × 105 CFU/ml. The total number of bacteria was also higher in patients of the first group with periodontitis (3.0 ± 1.0 × 106 CFU/ml) compared to the second group (2.7 ± 0.8 × 106 CFU/ml).Immunological study confirmed the presence of inflammatory response in patients with periodontitis. The level of interleukin-6 (IL-6) reached 18.3 ± 0.9 pg/ml in subgroup "B" of the first group and 19.3 ± 0.5 pg/ml in the second group. The concentration of interleukin-10 (IL-10) was higher in the second group (23.2 ± 0.8 pg/ml) compared to the first (22.2 ± 1.1 pg/ml). The level of secretory immunoglobulin A (sIgA) was 201.5 ± 1.7 mg/l in subgroup "B" of the first group and 200.8 ± 1.6 mg/l in the second, indicating activation of local immunity.
|
5. Conclusions
- The study demonstrated significant differences in clinical, functional and immunological changes in patients who underwent prosthetics with zirconium and metal-ceramic bridge structures. It was found that the use of zirconium prostheses is accompanied by less inflammatory changes in the periodontal tissues, which is manifested in a decrease in the depth of periodontal pockets, a decrease in the microbial load and lower levels of proinflammatory cytokines (IL-6 and IL-10). This confirms the high biocompatibility of zirconium and its minimal impact on the local immune response. Metal-ceramic structures, despite their strength and aesthetic properties, demonstrate a more pronounced effect on the tissues of the oral cavity, accompanied by an increase in the level of pathogenic microflora (Porphyromonas gingivalis, Fusobacterium nucleatum) and inflammatory markers. Such changes require mandatory sanitation of the oral cavity and treatment of periodontitis before installing metal-ceramic prostheses.The results of the study emphasize the need to select bridge materials taking into account the periodontal condition and the oral microbial profile. Zirconium structures are the optimal choice for patients at risk of developing inflammatory diseases. The data obtained can be used to improve orthopedic treatment protocols and develop individualized approaches in dentistry.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML