-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 562-564
doi:10.5923/j.ajmms.20251503.15
Received: Feb. 12, 2025; Accepted: Feb. 26, 2025; Published: Mar. 8, 2025

Risk Factors Leading to Kidney Damage in Patients with Ischemic Heart Disease
Akhmedova Nilufar Sharipovna1, Zaripov Odil Olimovich2
1Professor, Deparmnent of Faculty and Hospital Therapy, Bukhara State Medical Institute, Bukhara, Uzbekistan
2Independent Researcher, Department of Faculty and Hospital Therapy, Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Akhmedova Nilufar Sharipovna, Professor, Deparmnent of Faculty and Hospital Therapy, Bukhara State Medical Institute, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Coronary heart disease (CHD) is currently one of the most common diseases among the population and one of the leading causes of death. Fatal outcomes associated with this disease are caused not only by the underlying pathology, but also by its complications. One of these complications is renal dysfunction in CHD, which increases the mortality rate due to the comorbid condition. In our study, we studied the significance of etiologic risk factors contributing to the development and progression of nephropathy in patients with CHD of different ages and genders.
Keywords: CHD, Chronic kidney disease, Age, Gender, Risk factor
Cite this paper: Akhmedova Nilufar Sharipovna, Zaripov Odil Olimovich, Risk Factors Leading to Kidney Damage in Patients with Ischemic Heart Disease, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 562-564. doi: 10.5923/j.ajmms.20251503.15.
1. Introduction
- In recent years, the world community has been facing a global problem not only in the field of medicine, but also of socio-economic importance for countries - the annual increase in mortality and disability among the population as a result of the pandemic of chronic non-communicable diseases and their complications [2,4]. In particular, based on scientific research, it is shown that the incidence of ischemic heart disease, hypertension, atherosclerosis, depression, diabetes mellitus, obesity, gastric and intestinal ulcers, and tumor diseases, as well as disability and mortality as a result of them, are increasing [1,6]. The results of kidney function and urine analysis, studied during screening processes among tens of thousands of people in different countries, showed that one in ten people in the world has chronic kidney damage of varying degrees. All cases of kidney damage of varying degrees, not detected and not treated in a timely manner, develop over the years, as a result of which patients are forced to resort to dialysis or kidney transplantation procedures. Chronic kidney disease is considered one of the socially urgent problems that can negatively affect public health and the economic situation of the country, occurring in almost 15% of the population of developed countries, and the resulting chronic kidney disease is characterized by a high incidence of disability and mortality among patients [2,3,6]. The concept of chronic kidney disease was introduced into science and put into practice at the beginning of the 21st century in the USA after numerous scientific studies and publications of their results by the National Kidney Foundation (NKF). In 2002, a practical recommendation on the principles of identifying and treating patients with chronic kidney disease K/DOQI (Kidney Disease Outcomes Quality Initiative) was developed and implemented in the USA [6]. The widespread introduction of the concept of CKD into medical practice leads to the early identification of risk factors and causes of the development of this disease and the need for patients to consult a nephrologist and cardiologist in the early stages of the disease.The aim of the research is to study the age-related features of renal dysfunction and the development of renal tissue fibrosis in patients of different ages with coronary heart disease and to improve the prevention of nephropathies.
2. Materials and Methods
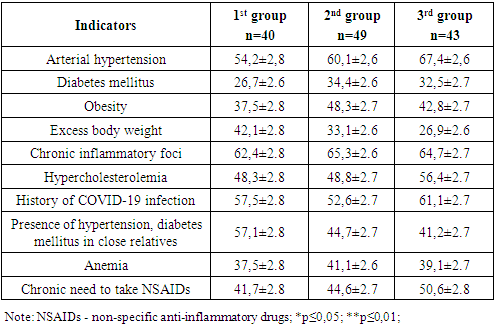
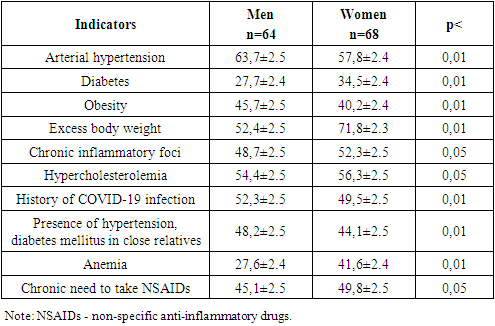
- The study involved 132 patients who received outpatient treatment and inpatient treatment in the therapy department of the Kagan City Medical Center of the Bukhara region during 2021-2023. Taking into account the established criteria, 132 patients under the age of 18 with coronary heart disease were included in the study. Of these, 68 were women and 64 were men, with an average age of 54.8±4.7 years.Since the purpose of the work was to study the significance of age in the manifestation of renal dysfunction, the patients were divided into 3 groups.1 group - 40 patients aged 18-44 years (30.3%)2 group - 49 patients aged 45-59 years (37.1%)3rd group - 43 patients aged 60-74 years (32.6%)To assess kidney function, the content of Cystatin C, creatinine, urea in blood and urine, galectin 3 in blood serum, urine analysis, and collagen 4 in urine were determined.Statistical analysis of the obtained results was carried out using Microsoft Office Excel 2010 (Microsoft Corp., USA) and Portable Statistica 8 (StatSoft, Inc., USA). The description of categorical data was carried out in the form of level indicators, expressed as percentages. Considering that most of the analyzed properties have a different distribution than usual, non-parametric statistical tests were used for statistical analysis of the obtained results. The relationship between the studied properties was assessed using the Spearman degree correlation method (r - correlation coefficient).
3. Results and Discussion
- Analysis of the research results showed that in patients with coronary heart disease, a number of risk factors leading to renal dysfunction are important, and the significance of these factors varies depending on age. Table 1 presents an age-related analysis of the significance of risk factors in patients with CHD. From the data presented in the table, it can be concluded that risk factors such as arterial hypertension, hypercholesterolemia, and the use of nephrotoxic drugs increase with age. It was noted that the incidence of such risk factors as chronic inflammatory foci, diabetes mellitus, and obesity was 0.6 and 0.9 times higher in the middle-aged group compared to the 1st and 3rd groups. In the younger group, there was a high risk of excess body weight, a tendency towards kidney damage, i.e., the presence of arterial hypertension, diabetes mellitus, and kidney diseases in close relatives.
|
|
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML