-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 539-541
doi:10.5923/j.ajmms.20251503.10
Received: Jan. 28, 2025; Accepted: Feb. 20, 2025; Published: Mar. 8, 2025

Immunoglobulins of Newborns Who Underwent Intrauterine Transfusion in the Antenatal Period
Salimova K. A., Jabborov U. U.
Republican Perinatal Center, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

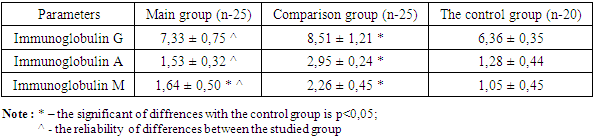
To study the indices of innate humoral immunity such as immunoglobulins G, M, A in umbilical cord blood of newborns with haemolytic disease who underwent high-tech fetal surgeries during pregnancy. The studies were conducted at the Republican Perinatal Center in 2024. A total of 70 newborns participated in the study and were divided into 3 groups. 1st main group of 25 newborns with haemolytic disease and who underwent ‘intrauterine, intravascular haemotransfusion to fetus’ operation in antenatal period, 2nd comparison group of 25 newborns with haemolytic disease and who did not undergo fetal surgery in antenatal period and 3rd control group of 20 healthy newborns. Immunological studies were done at the Institute of Immunology of the Academy of Sciences of the Republic of Uzbekistan. IgG in newborns in the comparison group was significantly increased 1.4 times in relation to the control group, and IgA and IgM were also significantly increased 2.3 times and 2.2 times in relation to healthy newborns. IgG, A, M indices in the main group of newborns where fetal technology was performed were not significantly different from those of the healthy control group. Fetal technologies not only improve haematological indices of fetal blood, but also improve the indices of humoral immunity of the newborn after birth, in particular, contribute to the decrease in the level of IgG, A and M. All this indicates a decrease in the inflammatory potential and prevents the formation of immunodeficiency state at birth.
Keywords: Immunoglobulins G, M, A, Rh-immunisation, Haemolytic disease of the newborn (HDN), Intrauterine blood transfusion (IUT)
Cite this paper: Salimova K. A., Jabborov U. U., Immunoglobulins of Newborns Who Underwent Intrauterine Transfusion in the Antenatal Period, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 539-541. doi: 10.5923/j.ajmms.20251503.10.
1. Introduction
- Intrauterine intravascular blood transfusion (IVF) remains the principal therapeutic intervention for severe fetomaternal anemia secondary to Rhesus immunization. As the destruction of fetal red blood cells happens due to maternal antibodies, the procedure is necessary to replace lost blood and to prevent anemia and complications related to that. Fetal humoral immunity and its immunological effectiveness of GDP has recently been focused on. VVPC is primarily aimed at replenishing the fetal red blood cell deficiency due to hemolysis and preventing the subsequent deterioration of anemia and its complications. This process is typically done via umbilical cord vein under ultrasound guidance. The indication for MIC according to the researchers is severe fetal anemia, which is characterized by hematocrit below 15-25% in relation to normal for gestational age as well as hemoglobin levels below 80-90 g/l [1,2,3].The best hematological parameters of offspring are found in newborns delivered to patients who had undergone intrauterine intravascular transfusion (IVF) for rhesus alloimmunization, according to data published internationally [4]. Existing studies of perinatal outcomes in cases of severe erythrocyte alloimmunization treated with IUT have mainly centered around the perinatal survival outcome after IUT. Most of these studies were performed in developed countries. Limited studies have evaluated the effect of IUT on newborn clinical outcomes postnatally. Furthermore, data on fetal and neonatal outcomes in women with a diagnosis of rhesus conflict that underwent intrauterine transfusion (IUT) in developing countries are very scarce [5,6,7].Most studies of transfusion-induced immunological modulation have been performed in adult patients and children in intensive care settings. Under the perspective of encompassing the physiology of the maternal-fetal interface and intrauterine tolerance, the features of the development of fetal immune response in presence of allogeneic donor erythrocytes, and its implications on transplantation, preservation of erythrocytes, and effectiveness of intrauterine blood transfusions remain unanswered. [8,9,10].The aim of the study: was comparative assessment of humoral immunity factors (G, M and A immunoglobulins), as well as in the cord blood of newborns with hemolytic disease of the newborn caused by rhesus-conflict in pregnant women who have undergone inutero therapeutic ecos-peritoneal and intrauterine intravascular blood transfusion to the fetus.
2. Research Materials
- The research was conducted on a total of 70 newborns born at the Republican Perinatal Center in 2024. They were separated into 3 classes. The 1st main group included 25 newborns with hemolytic disease, who underwent the operation "intrauterine, intravascular hemotransfusion to the fetus" during the antenatal period, the 2nd comparison group included also 25 newborns with hemolytic disease, who did not undergo fetal surgery in the antenatal period, and the 3rd control group included 20 healthy newborns.Immunological research methods: the newborn immune status studies were carried out on and cord blood on the 1st day of life in the Laboratory of Fundamental Immunology in Institute of Human Immunology and Genomics of the Academy of Sciences of the Republic of Uzbekistan.Levels of the basic immunoglobulin and cytokines in biological fluids were determined by way of enzyme immunoassay (ELISA) using commercial Human test systems (Germany). The test systems are based on solid–phase enzyme immunoassay using horseradish peroxidase as an indicator enzyme of the sandwich method. Reagent kits are a set, wherein the principal reagents are MCATs for the studied cytokines, sorbed on a surface of hills of a collapsible polystyrene tablet. The kits are for the quantitative determination of human cytokines in peripheral blood serum and in biological fluids. The optical density of the wells was read at 450 nm using an automatic photometer for microplates (Stat-Fax analyzer, USA) by enzyme immunoassay.Statical analysis of results was performed by parametric and nonparametric methods. The information was accumulated, corrected, systematized and the results were visualized in Microsoft Office Excel 2018 spreadsheets. The statistical analysis was performed using the IBM SPSS Statistics v.26 software (IBM Corp, Armonk, NY). For normally distributed quantitative data sets, the Student's t-test was calculated for the comparison of averages. The values of Student's t-test obtained were assessed against critical values. Differences in the indicators were considered statistically significant p<0.05.
3. Result and Discussion
- Implementing an immunological examination and validating the effectiveness of intrauterine intravascular fetal hemotransfusion provided an evaluation of humoral immunity in neonates on background of fetal surgery. To this end, immunological studies of humoral immunity in the umbilical cord blood of newborns with HDN, who have undergone intrauterine hemotransfusion, were carried out, and who have not undergone hemotransfusion. The results are depicted below in Table 1.
|
4. Conclusions
- 1. Umbilical cord blood IgG index was not significantly increased in the main group newborns who received fetal technologies during the antenatal period against the group of healthy newborns.2. In the umbilical cord blood of newborns not subjected to intrauterine hemotransfusion of the antenatal period, IgA, increased 2.3 times compared to the control group and IgA was not increased in newborns in the main group.3. The level of IgM in the umbilical cord blood of newborns of the comparison group, i.e., where pregnancy occurred traditionally significantly increased 2.2 times compared with the control group.4. Hemotransfusion of the fetus, intrauterine, through the blood stream also led to an improvement in fetal blood hematological parameters and to humoral immunity changes, particularly a need from immunoglobulins G, A, M. All of this indicates a reduced inflammatory potential and prevents the formation of an immunodeficiency state at birth.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML