-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(3): 504-508
doi:10.5923/j.ajmms.20251503.04
Received: Feb. 6, 2025; Accepted: Feb. 26, 2025; Published: Mar. 5, 2025

Informative Value of Spinal Biopsy in Diagnosing Tuberculous Spondylitis
Babоev Abduvakhob Sakhibnazarovich
Deparment of Osteoarticular Tuberculosis of Rebuplican Specialized Scientific Practical Medical Center of Phtiziology and Pulmonology, Tashkent, Uzbekistan
Correspondence to: Babоev Abduvakhob Sakhibnazarovich, Deparment of Osteoarticular Tuberculosis of Rebuplican Specialized Scientific Practical Medical Center of Phtiziology and Pulmonology, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Medical data of 75 patients (age range 25-80 years, average age 60 years) with tuberculous spondylitis (TS) who underwent percutaneous spinal biopsy, surgical debridement and spinal fusion with titanium mesh cages analyzed to determine the accuracy of vertebral biopsy in the diagnosis of TS. Histology of the spine biopsies showed tuberculous inflammation in 8(10.7±3.6%) cases, and open surgical specimens histological assessment showed tuberculous inflammation in 30(40±5.7%) cases. Gene Xpert® MTB/Rif positive results achieved in 23(30.7±5.3%) of the biopsy aspirates and lavage fluids, and in 37(49.3±5.8%) open surgery specimens. The informational value of percutaneous fluoroscopy guided vertebral biopsy is lower than the informational value of the open biopsy for diagnosing TS. A negative result of percutaneous vertebral biopsy requires dynamic monitoring, empirical treatment, and open surgical procedure in case of complications.
Keywords: Tuberculous spondylitis, Biopsy, Surgical treatment
Cite this paper: Babоev Abduvakhob Sakhibnazarovich, Informative Value of Spinal Biopsy in Diagnosing Tuberculous Spondylitis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 3, 2025, pp. 504-508. doi: 10.5923/j.ajmms.20251503.04.
Article Outline
1. Introduction
- Approximately a quarter of the world’s population is infected with Mycobacterium tuberculosis. According to the WHO, in 2021, 537 million adults worldwide were living with diabetes [19]. The total number of people living with HIV in 2023 was 39.9 million [20]. In 2019, the global prevalence of liver diseases was 1.69 billion [7]. One in ten individuals suffers from autoimmune diseases [3] and periodically or continuously takes corticosteroids. Consequently, individuals diagnosed with spondylitis, especially from these high-risk groups, require early verification of the diagnosis, as widespread and complicated forms of tuberculosis spondylitis (TS) occur in 70% of adults due to delayed diagnosis [15].Additionally, identifying the pathogen and drug sensitivity allows effective, targeted antimicrobial therapy [5,12,17]. Drug resistance of Mycobacterium tuberculosis reaches 40-56% among previously treated patients and 15-20% among primary cases [2,16].Radiological methods currently play a leading role in diagnosing TS. Depending on the duration and activity of the tuberculous process in the spine, the combined specificity of MRI and CT is sufficiently high, exceeding 85% [10]. However, the longer and more active the TS, the more complications arise.At early stages of TS, before abscesses and significant destruction and collapse of vertebral bodies occur, the combined specificity of MRI and CT is low [14]. Therefore, when immunological skin and laboratory tests are negative, percutaneous biopsy is recommended for patients with inflammatory spine diseases.Currently, there are no definitive criteria predicting the effectiveness of biopsy in detecting the pathogen, and reported data show varying diagnostic efficacy. Moreover, spinal biopsy is not a technically simple procedure and can lead to various complications such as pain, bleeding, neurological disturbances, pneumothorax, and others [6,8,13,17,18].
2. Purpose
- To determine the accuracy of vertebral biopsy in the diagnosis of tuberculous spondylitis.
3. Materials and Methods
- The study involved 75 (100%) patients with TS hospitalized to the bone and joint tuberculosis surgery department in 2023-2024. The patients' ages ranged from 25 to 80 years, with a mean age of 60. Males accounted for 46(61,3±0,56%), and females for 29(38,7±0,56%).During the general examination, complaints, duration of the primary disease, treatment received, identified comorbidities and their complications, harmful conditions, and habits were recorded.Orthopedic examination assessed the source of pain, pain intensity, mobility, and any accompanying orthopedic pathology.Neurological examination provided information on neurological impairments, the level of damage, and accompanying neurological diseases.All patients underwent ECG, echocardiography, Doppler ultrasound, general blood and urine analysis, coagulation profile, and biochemical blood tests for internal organ function assessment. Based on indications, bacteriological and cytological studies were performed.For spinal visualization, all patients underwent both MRI (1.5 Tesla) and CT (Siemens Definition AS 64, Germany) to analyze bone structures and soft tissues of the affected segment. Chest radiography was performed for lung pathology assessment, and MSCT of the chest was done if indicated.Surgical treatment was indicated after ineffectiveness of anti-tuberculous therapy proved on MRI and/or CT and in cases of progression of neurological deficits. Prior to surgical procedures, potential complications were explained to the patients, and written consent was obtained.A surgical approach to the lumbar spine was obtained through a lateral skin incision, oblique (external and internal) and transverse abdominal muscle incisions, via the retroperitoneal space and the psoas muscle. The thoracic spine was exposed by a lateral intercostal thoracotomy on the right side. The cervical spine was approached by standard anterior technique. Then, removal of abscesses and necrotic tissues, spinal cord decompression, and spinal fusion using titanium mesh cages were performed.Before open surgery, a percutaneous spine biopsy was performed in each case under fluoroscopic control using an 8-11G, 150 mm trepan needle. Standard transpedicular, costotransverse, and anterolateral cervical approaches were used. Approachable paravertebral abscesses were also punctured. Abscesses, aspirates, and lavage fluids underwent bacteriological testing using the molecular genetic method GeneXpert® MTB/Rif (Sunnyvale, California, USA).Biopsy and removed pathological tissues during surgeries were macroscopically selected by the morphologist, fixed in formalin for 2-3 weeks, then 10-15 slices were prepared on a microtome and stained with hematoxylin-eosin using standard methods.The TS diagnosis was made based on combined findings from MRI, CT, tuberculin skin tests, bacteriological, and histological reports.Statistical analysis of the study was carried out using modern computer systems such as IBM/PQ of the latest generation using a package of standard Excel programs.
4. Results
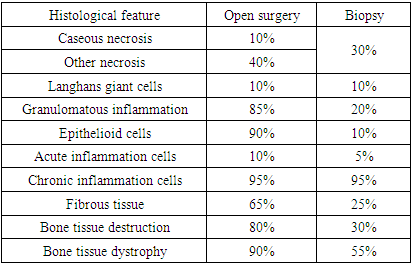
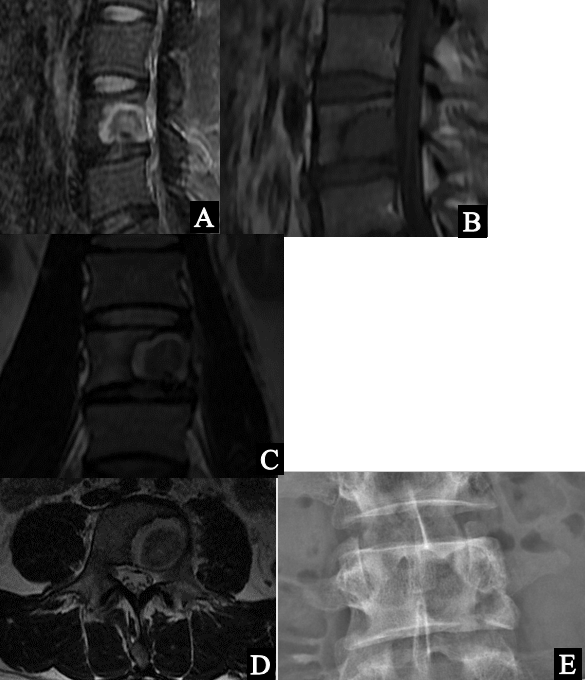
- The duration of the disease before hospitalization to our clinic in our patients was 12.1±5.3 months. Intoxication was observed in all 75 (100%) of the patients we examined, manifested as fatigue, sweating, periodic fever, decreased appetite, and weight loss. High pain intensity was noted in 27 (36±5.5%) patients, moderate in 44 (58.7±5.7%) patients, and mild in only 5 (6.7±2.8%) patients. Instability was observed in 70 (93.3±2.8%) patients, with a sharp increase in pain during axial and angular load. Radicular pain occurred in 36 (48±5.8%) cases. Paresis and paralysis were noted in 7 (9.3±%) patients with TS of the thoracic spine. Tuberculin skin test showed a positive result in 56 (74.7±0.5%) patients.According to the results of radiographic and tomographic lung studies, previous pulmonary and pleural tuberculous lesions were found in 24 (32±0.54%) patients, and active pulmonary and pleural tuberculosis was found in 14 (18.7±0.45%) patients.We examined 2 (2.7±1.9%) patients in the early spondylitic phase of tuberculous inflammation. One had a focus of destruction in the body of the VL4 vertebra, without sequestration, with a destroyed lower endplate, a hypointense signal of the destruction focus in the T1 mode, an uneven signal in the T2 and STIR modes, an intact intervertebral disc, and no soft tissue reaction such as infiltration or abscess in one case (Figure 1). Another had a focus of destruction in the body of the VTh5 vertebra, without sequestration, with a destroyed lateral shell, soft tissue infiltration, a hypointense signal of the destruction focus in the T1 mode, a hyperintense signal in the T2 and STIR modes, and an intact intervertebral disc (Figure 2).
 | Figure 1. Tuberculous focus in VL4 vertebral body. MRI A- sagittal fat-suppressed T2 weighted; B – sagittal T1 weighted; C – frontal T2 weighted; D- axial T2 weighted. E – plain X-ray |
 | Figure 2. Tuberculous focus in VTh5 vertebral body. CT scan: axial(A), frontal (B) and sagittal (C) reconstructions |
|
5. Discussion
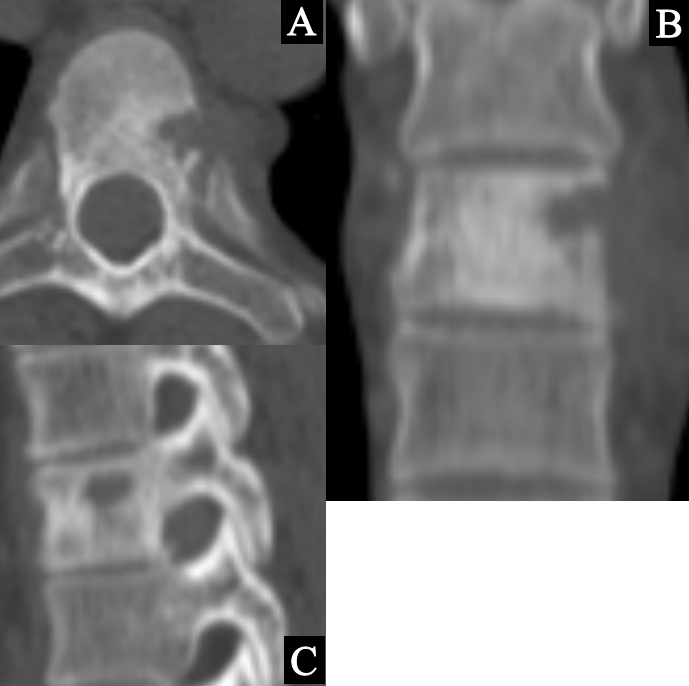
- In the prespondylitic phase of tuberculous spondylitis, when the destruction focus is located within the vertebral body, local discomfort or pain may occur, along with possible symptoms of intoxication, such as sweating, weakness, and fever. On MRI, the signal from the focus of destruction and the vertebral body is hypointense on T1-weighted images, hyperintense or more frequently heterogeneous due to the destruction focus, sequestrum, and surrounding bone tissue edema on T2-weighted images. It is hyperintense on the STIR sequence, and surrounding soft tissues are either intact or infiltrated [9,10]. The same signs can be find in metastases, neoplasms, and vertebral cysts. On CT, during that phase, focus of destruction with osteoporotic ages can be identified, according to the literature in 89% of cases that destruction contains a sequestrum. In our study, only 2 (2.7±1.9%) patients were hospitalized in the early spondylitic phase of tuberculous inflammation and the sequestration was identified only in 10 (13.3±3.9%) cases. With the progression of TS and the onset of the spondylitic phase, both local and general clinical symptoms worsen. The patient is suffering from intense pain due to instability of the affected spinal segment and compensatory skeletal muscle spasms, radicular pain due to irritation of nerve roots and the spinal cord. According to the literature, in 40-80% of cases, TS presents with the most typical form of contact destruction of two or three (30-35%) vertebral bodies, abscess formation, vertebral subtotal destruction and pathological fractures, making the radiographic image clearer and also indicating a prolonged process [10,13]. In our study the duration of the disease before hospitalization to our clinic was 12.1±5.3 months. Intoxication was observed in all the patients. High pain intensity was in 27(36±5.5%) cases, patients, contact destruction of two adjacent vertebrae occurred in 48(64.0±5.5%) cases, more than two vertebrae in 17(22.6±0.48%), and abscesses in 56 (74.7±5.0%) patients. Subtotal vertebral destruction occurred in 27 (36±5.5%) patients. Lee JE et al, 2011 evaluated sensitivity, specificity, positive predictive value, and negative predictive value of tuberculin skin test equal to 94% (95% CI, 87-98%), 88% (95% CI, 74-96%), 95% (95% CI, 88-98%), and 86% (95% CI, 72-94%), respectively in suspected active TB in South Korea [11]. In our study tuberculin skin test showed a positive result in 56 (74.7±0.5%) patients.Because of oligobacillary nature of extrapulmonary tuberculosis, MBT detection in bone and joint tuberculosis patients does not exceed 40-60% according to various authors [1].Cuong NK et al, 2023 found positive MGIT culture among surgical vertebral specimens in 51.3%, fine needle aspiration positive MIGT culture rates were 26.3% in lymph node and 25.3% in pleural specimens. The most common histopathoglogical suggestive finding of TB was the presence of epithelioid cell (83.3%), Langhans giant cells (75.9%), and caseous necrosis (75.5%) [4]. In our study, histological confirmation of tuberculous inflammation achieved in 8(10.7±3.6%) biopsies, but in 30(40±5.7%) open surgical specimens.
6. Conclusions
- The informational value of percutaneous fluoroscopy guided vertebral biopsy is lower than the informational value of the open biopsy for diagnosing TS. A negative result of percutaneous vertebral biopsy requires dynamic monitoring, empirical treatment, and open surgical procedure in case of complications.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML