-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(2): 487-489
doi:10.5923/j.ajmms.20251502.48
Received: Jan. 20, 2025; Accepted: Feb. 23, 2025; Published: Feb. 28, 2025

Purulent Bacterial Complications in Children with Infectious Mononucleosis
1Republican Specialized Scientific and Practical Medical Center of Epidemiology, Microbiology, Infectious and Parasitic Diseases of Ministry of Health Republic of Uzbekistan, Tashkent, Uzbekistan
2City Clinical Infectious Disease Hospital No.1 in Tashkent, Uzbekistan
Correspondence to: Shermukhamedova G. T., Republican Specialized Scientific and Practical Medical Center of Epidemiology, Microbiology, Infectious and Parasitic Diseases of Ministry of Health Republic of Uzbekistan, Tashkent, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

According to WHO, 90% of people on the globe are infected with the herpes virus, of which 50% have a manifest form of the disease, a recurrent course. Infectious mononucleosis (IM) affects 16 to 800 people per 100 thousand people per year. One of the main clinical symptoms of MI is damage to the oropharynx in the form of catarrhal or exudative lesions of the oropharynx. Since the 60s of the twentieth century, it has been suggested that the cause of sore throat during MI (exudative sore throat, plaque on the tonsils) is of a viral-bacterial nature, in which the leading place is occupied by the microbial flora [2,3,4]. This fact became an indication for the prescription of antibacterial therapy in the treatment of MI. However, in parallel with this, other scientists emphasized that the leading place in pathological changes in the throat is occupied by viral etiology, and pathogenic microorganisms have minimal importance in the development of sore throat [6,7]. Rodionova O.V. (2000) in their studies argues that sore throats during MI are caused by virus-microbial interaction, with the virus taking the leading place. According to Bernstein B. (2006), in 30% of cases, secondary flora is associated with MI accompanied by angina, and in a third of patients, Str. pyogenes, and the author noted the advisability of prescribing antibacterial therapy to these patients.
Keywords: Infectious mononucleosis, Children, Procalcitonin, Bacteriological examination
Cite this paper: Shermukhamedova G. T., Purulent Bacterial Complications in Children with Infectious Mononucleosis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 2, 2025, pp. 487-489. doi: 10.5923/j.ajmms.20251502.48.
1. Material and Methods of Research
- A prospective study of 120 patients with the diagnosis of infectious mononucleosis hospitalized in the box department of the City Clinical Infectious Diseases Hospital No.1 in Tashkent was conducted.
2. Results Obtained
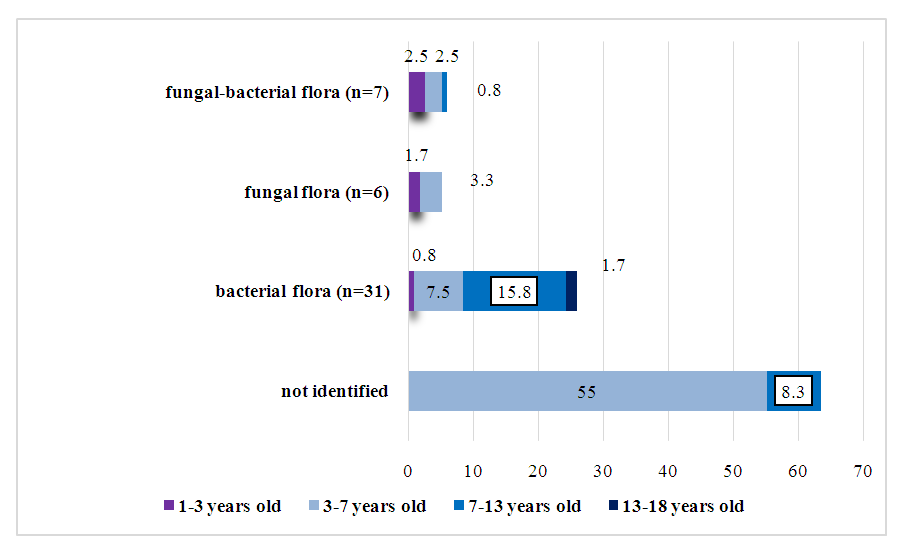
- In all examined children there were no significant differences depending on sex, a significant part of patients were 82 (68.3%) children of preschool age (3-7 years), the rest were school-aged children (7-13 years) - 30 (25.0%) children, while children of early (1-3 years) and pubertal age (13-18) were 6 (5.0%) and 2 (1.7%) children, respectively. When analyzing the results of bacteriological examination, pathogenic microflora was isolated in 31.7% of patients in the main group, of which Staphylococcus aureus was detected in 21.7% of patients, Streptococcus pyogenes - in 10.0%. Candida albicans was isolated in 10.8% of patients, and pathogenic microflora was also detected in 7 patients, i.e. patients with bacterial-fungal association amounted to 5.8% of all examined patients. Based on these data, the patients were divided into the following groups: patients with identified bacterial flora (n=31), with identified fungal infection (n=6), with fungal-bacterial association (n=7), as well as patients with no pathogenic flora in the number of 76 children (Fig. 1).
 | Figure 1. Results of bacteriologic examination of swabs from the pharynx taken from patients (n=120) |
 | Figure 2. Formation of purulent-inflammatory process depending on the age of patients |
3. Conclusions
- 1. At viral etiology of purulent-inflammatory process the disease runs with febrile fever (p<0,05), catarrhal changes of oropharynx, at bacterial and bacterial-fungal association hectic fever is characteristic (p<0,05), and at fungal etiology - febrile (χ2 =3.745), and at three of these conditions inflammation of pharynx is manifested with obvious plaque (χ2 = 64.039). 2. In infectious mononucleosis the etiologic factor of purulent-inflammatory process in the oropharynx in 31.7% of cases is pathogenic bacterial flora, in particular Staphylococcus aureus - 21.7%, Streptococcus pyogenes - 10.0%, and Candida albicans - 10.8%, and also in 5.8% of cases is bacterial-fungal association.3. In children with infectious mononucleosis, the age of children older than 7 years (χ2=29.358), the age of children younger than 3 years (P<0.05), artificial feeding before 1 year of age (χ2=28.4), the presence of concomitant diseases such as anemia, rickets, chronic inflammatory diseases of the respiratory system (p<0.05) are important in the development of secondary bacterial infection.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML