Khasanova Kamola Musadjanovna
Republican Specialized Scientific and Practical Medical Center of Cardiology, Uzbekistan
Correspondence to: Khasanova Kamola Musadjanovna, Republican Specialized Scientific and Practical Medical Center of Cardiology, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Nowadays, sleep disorders, in particular obstructive sleep apnea syndrome and insomnia, are one of the most common problems. The study used CBT methods on patients with a high apnea-hypopnea index and evaluated their effects on sleep quality, psychoemotional state and cognitive functions. The results of the study showed that CBT significantly improves parameters such as time to fall asleep, degree of insomnia and sleep quality in patients. However, the effect on snoring and apnea/hypopnea episodes was minimal. It was also observed that CBT therapy led to positive changes in the psychoemotional state of patients. This study confirms that CBT is one of the effective approaches in eliminating problems associated with OSAS and insomnia.
Keywords:
Cognitive-behavioral therapy (CBT), Obstructive sleep apnea syndrome (OSAS), Insomnia, Sleep disorders, CPAP therapy, Psychoemotional state, Cognitive functions, Sleep quality, Apnea-hypopnea index, Polysomnography (PSG), Snoring, Quality of life, Depression
Cite this paper: Khasanova Kamola Musadjanovna, Cognitive-Behavioral Therapy for Obstructive Sleep Apnea Syndrome and the Effect on Insomnia, American Journal of Medicine and Medical Sciences, Vol. 15 No. 2, 2025, pp. 453-456. doi: 10.5923/j.ajmms.20251502.39.
1. Introduction
Globalization and lifestyle changes in the world are leading to an increase in complaints of insomnia. In developed countries, insomniacs account for about 25% of the population, and millions of people are dependent on sleeping pills. At the same time, the demand for sleeping pills is increasing day by day. Among sleep disorders, obstructive sleep apnea syndrome is the most common, which occurs in obesity, due to anatomical anomalies of the facial and upper respiratory tract. Studies have shown that obstructive sleep apnea syndrome (OSAS) is significantly higher in obese patients (30-98%), while this indicator is lower in patients with normal body weight (15-26%) [1]. The literature also shows that metabolic changes occur in OSAS [1].Recent literature has reported the use of psychotherapy to improve adherence to CPAP therapy. The use of psychotherapy not only helps to improve adherence to therapy, but also to correct psychoemotional disorders and insomnia caused by the disease [2]. Among the psychotherapy methods, cognitive behavioral therapy (CBT) is the most effective, helping to shift sleep from the wakefulness to the Non-REM phase and has a positive effect on increasing the duration of REM sleep [3]. CBT has been shown to be effective not only in insomnia but also in COMISA syndrome [4].Despite its widespread prevalence worldwide, this syndrome is underdiagnosed and undertreated. In 80% of cases, moderate to severe sleep apnea remains undiagnosed and untreated. This leads to a deterioration in quality of life, insulin resistance, and an increased risk of cardiovascular disease (CVD) [5].
2. Research Objective
The main objective of this study is to evaluate the effect of cognitive behavioral therapy (CBT) on the course of obstructive sleep apnea syndrome (OSAS) and insomnia. The study investigated the effectiveness of CBT in correcting sleep disorders in patients with a high apnea-hypopnea index. The effect of CBT on factors such as psychoemotional state, cognitive functions, and quality of life was also analyzed.
3. Material and Methods
During our study, 94 patients (81%) with an apnea - hypopnea index of more than 5/hour (norm ≥5/hour) underwent CBT to treat sleep disorders, explain sleep hygiene, and correct anxiety and depression, and the results of the individual psychotherapy treatment method conducted for each patient showed that it was statistically significant. The correction of psychoemotional and cognitive changes resulting from sleep disorders using cognitive-behavioral therapy (CBT) was one of the main tasks of our research. We know that the psychoemotional and cognitive state of patients is one of the main factors affecting the course of ischemic heart disease (IHD). It is no coincidence that IHD has recently been included in the group of psychosomatic diseases.
4. Results
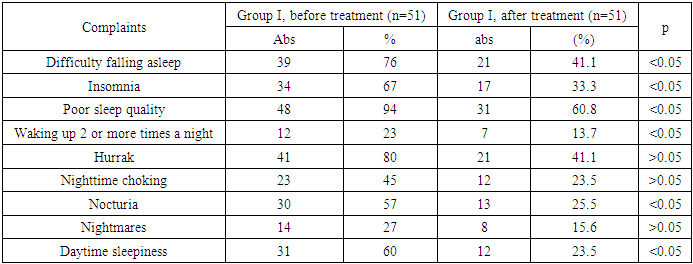
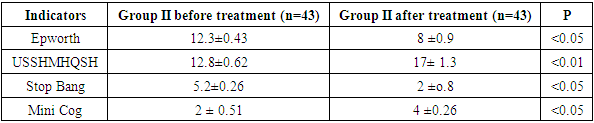
When PSG was performed on subjects who complained of subjective sleep disturbances, 19% of subjects (n=116) who complained of sleep disturbances did not have sleep disturbances confirmed by objective tests. This indicated that the sensitivity of the sleep scales was 81%.To assess the effectiveness of treatment, patients were divided into 2 groups. Group I (n=51) patients underwent CBT in combination with the basic treatment of UIC. Group II (n=43) underwent CPAP therapy (continuous positive airway pressure) and CBT in combination with the treatment standards of UIC. In order to assess the effectiveness of CBT, CBT methods were used only in group I patients. Patients who were offered CBT underwent CBT 3-6 times in inpatient conditions and 3 times a month in outpatient conditions.When performing CBT in group I patients, statistically significant (p<0.05) dynamics were observed in all indicators of subjective complaints about sleep (Table 1).Table 1. Dynamics of subjective complaints of sleep disorders after ENT in group I
 |
| |
|
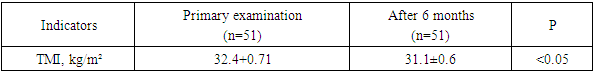
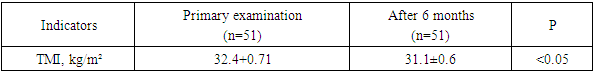
If we focus on the analysis of subjective sleep complaints I group of patients reported a significant decrease in complaints, ENT as a result to sleep of leaving difficulty, insomnia, sleep quality, night awakenings and ten-day in drowsiness positive and convincing we can see the dynamics (p<0.05). But, snoring and apnea / hypopnea in episodes positive changes not detected.It is known that CBT also affects weight indicators in patients. In group I patients, positive dynamics were observed in BMI (body mass index) against the background of CBT, which was found to be statistically significant p<0.05 (Table 2).Table 2. Comparative analysis of TMI before and after treatment in group I
 |
| |
|
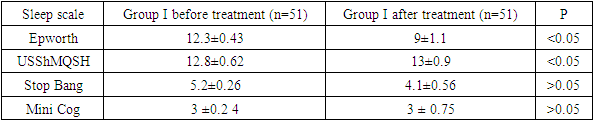
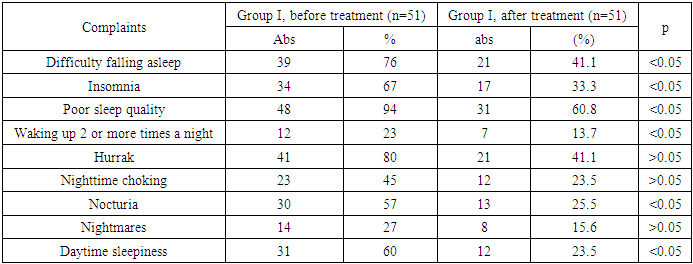
Surveys patient of life quality in determining significant to be, to be using patient spiritual status about general to the concept has let 's be and treatment directions our change possible. As we mentioned in the literature review, the Epworth questionnaire provides a broad measure of insomnia and sleep quality. From this perspective, this questionnaire is widely used worldwide. After CBT, in our patients, positive dynamics were detected when studying sleep quality using the Epworth and USSHMQSH (Modified Subjective Sleep Complaints Scale), but no positive dynamics were detected on the STOP BANG, i.e. snoring scale (p>0.05) (Table 3).Table 3. Analysis of sleep scales in group I
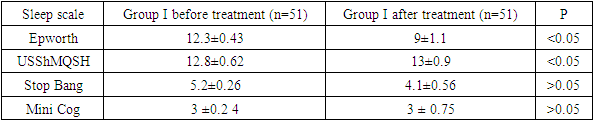 |
| |
|
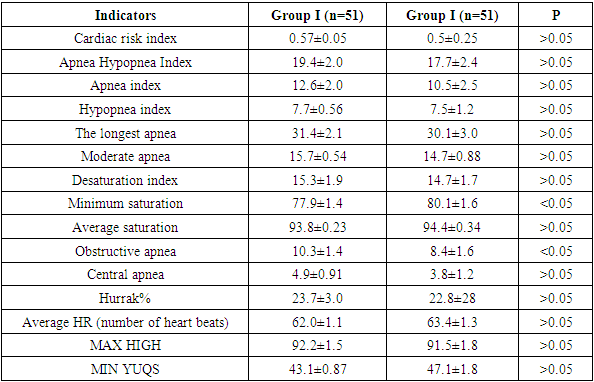
As we can see, many questionnaires are used to assess sleep disorders and their causes. The “Sleep Disorders Screening Questionnaire” (DGU No. 18036) developed by us is convenient for patients and doctors, and allows us to simultaneously determine the psychoemotional state, sleep quality, sleep snoring and cognitive disorders. With this questionnaire, we saw that the quality of sleep, psychoemotional state improved in group I patients (p<0.05), while no differences were found when comparing the results with Epworth, STOP BANG, USSHMQSH and Mini Cog.Although there were statistically significant changes in subjective complaints of anxiety, depression, and insomnia in patients who underwent CBT (p>0.05), the gold standard for diagnosing sleep disorders No significant dynamics were observed in the standard PSG parameters (p>0.05). This can be explained by the preservation of snoring and the fact that the effect of apnea/hypopnea syndrome was not eliminated by CBT (Table 4).Table 4. Analysis of polysomnography results in group I patients
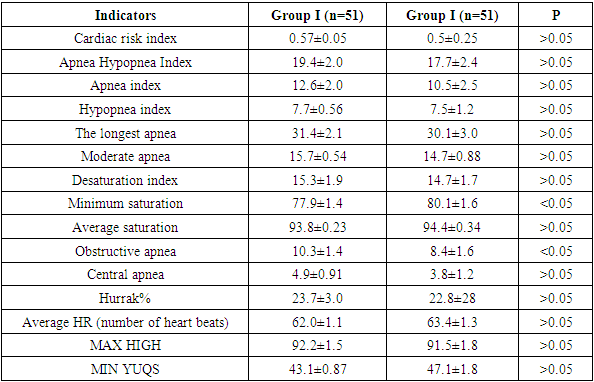 |
| |
|
Analysis of the results of a combined CPAP therapy and CBT course.An analysis of the average data on the CPAP device over 6 months in patients who underwent CPAP therapy is presented in Table 5.Table 5. Indications for CPAP therapy in patients
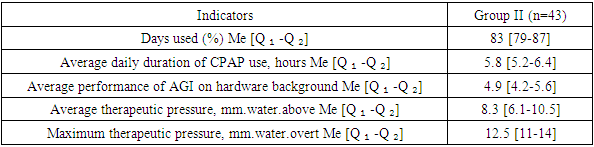 |
| |
|
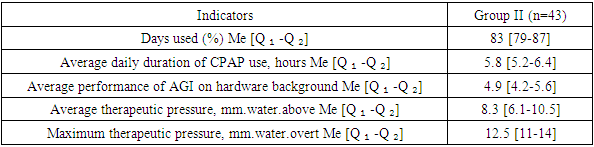
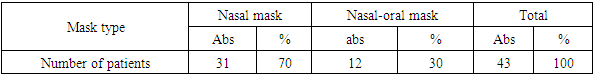
According to the data obtained, CPAP therapy was used in more than 71% (83 [3]) of cases over 6 months, which corresponds to the treatment standards. The recommended time of using the device during the night was on average 6 hours, and our patients also adhered to the recommendations (5.8 [5.2-6.4]). The average results of AGI against the background of treatment were 4.9 [4.2-5.6]/hour, which is a normal indicator according to the recommendations. The average (8.3 [6.1-10.5]) and maximum therapeutic pressure (12.5 [4]) were selected individually for each patient, and the above results indicate that the above-mentioned indicators were achieved in the right direction. The use of a humidifier was recommended for all patients to prevent side effects of the CPAP device.During treatment, an individual mask was selected for each patient. 70% of patients preferred nasal (through the nose) masks, 30% preferred oro-nasal masks (Table 6).Table 6. Masks used during CPAP therapy
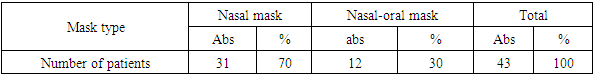 |
| |
|
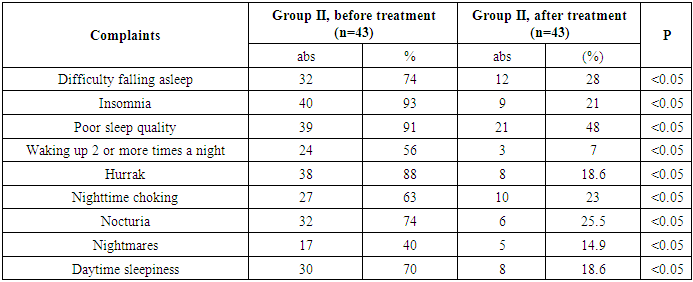
Scientists have recognized CPAP therapy as the most effective method of treating patients with obstructive sleep apnea syndrome (OSAS) and insomnia (COMISA). We have also witnessed this in our observations. This was especially evident in the subjective complaints of patients (p<0.05) (Table 7).Table 7. Dynamics of subjective sleep complaints in group II
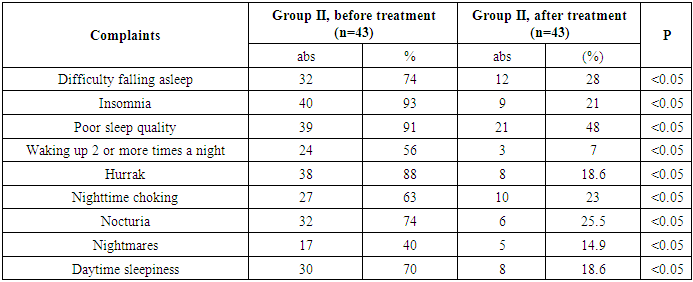 |
| |
|
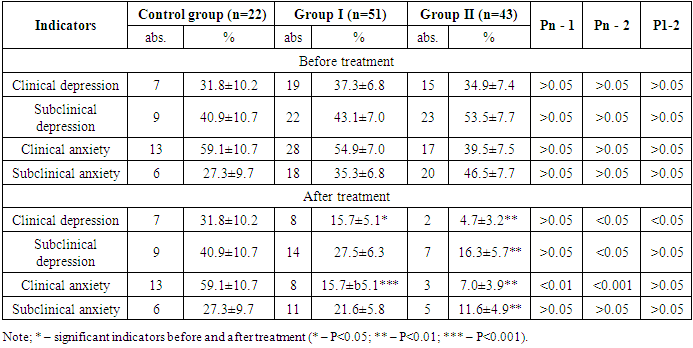
In order to identify anxiety and depression in our group I patients When analyzing the Hospital Anxiety and Depression Scale (HADS) questionnaire, subclinical anxiety was detected in 54.9±7.0% of patients (n=17) and pronounced anxiety in 35.3±6.8% of patients (n=20). If we look at the level of depression, we can observe subclinical depression in 53.5±7.7% of patients (n=15) in group I, and pronounced depression in 34.9±7.4% of patients (n=23). The results of the analysis of depression after treatment showed a significant level of dynamics (p<0.05) in groups I and II (Table 8).Table 8. Dynamics in groups according to the HADS scale in patients
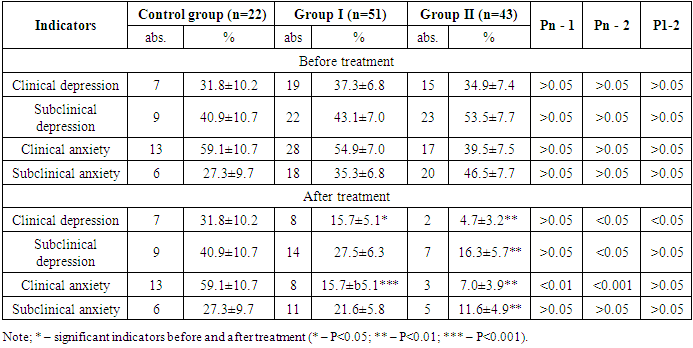 |
| |
|
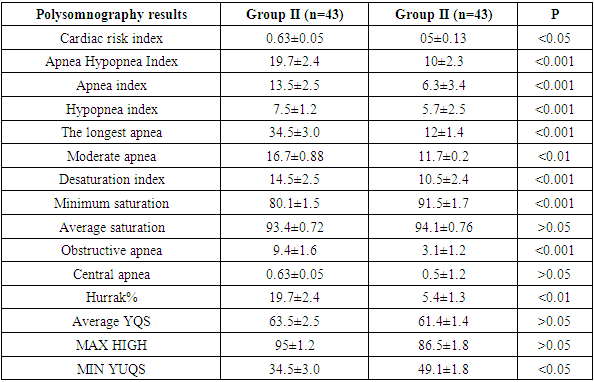
CPAP The elimination of snoring with the help of therapy, the increase in saturation, and the reduction of apnea/hypopnea as a result of the treatment were reflected in the subjective complaints of patients. When sleep complaints were used together with CPAP, all questionnaires showed that they were normal (p<0.05) (Table 9). When analyzing the “Sleep Disorders Screening Questionnaire”, positive dynamics were also revealed, as in the above questionnaires, we can see a significant improvement in psychoemotional state (p<0.001***), sleep quality (p<0.05*), sleep snoring (p<0.01**) and cognitive state (p<0.05*) compared to group I.Table 9. Dynamics of sleep scales in group II patients before and after treatment
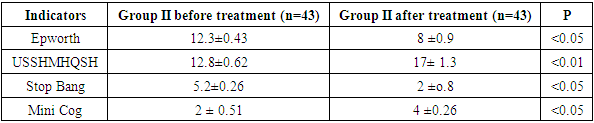 |
| |
|
In our study, among the polysomnography (PSG) parameters, apnea/hypopnea index, longest desaturation, desaturation index, minimum saturation, average saturation and UQS number are significant indicators, which allow us to know the effectiveness of treatment. We can also see a significant dynamic in sleep efficiency (p<0.001), slow wave sleep duration (p<0.01), REM sleep duration (p<0.05). In group II patients, when observed in dynamics, a statistically significant dynamic was recorded between AGI (p<0.001), apnea index (p<0.001), longest apnea (p<0.001), desaturation index (p<0.001), minimum saturation (p<0.001), obstructive apnea (p<0.001), snoring (p<0.01).Table 10. Dynamics of polysomnography indicators in group II
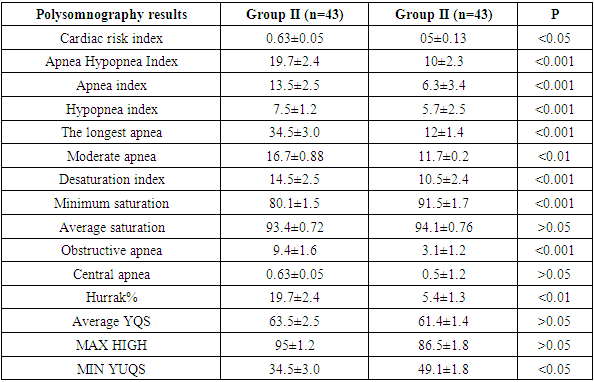 |
| |
|
5. Conclusions
The results of the study showed that CBT significantly improved the time to fall asleep, the degree of insomnia, and the overall quality of sleep. Subjective complaints of patients decreased, including insomnia, night awakenings, and positive dynamics in daytime sleepiness.The study found that patients who received CBT had significantly reduced levels of depression and anxiety, indicating that CBT is effective in improving not only sleep quality but also psychological factors.The results of the polysomnographic examination showed that CBT did not significantly affect the patients' snoring and apnea/hypopnea episodes, which suggests that the main effect of CBT therapy is focused on sleep quality and psychoemotional state.The study results showed that the combination of CPAP therapy and CBT significantly improved sleep quality and significantly reduced symptoms of obstructive sleep apnea syndrome, suggesting that the combination of CBT and CPAP therapy is one of the most effective approaches for patients with OSA and insomnia.
References
| [1] | McDermott M, Brown DL. Sleep apnea and stroke. Curr Opin Neurol. 2020 Feb; 33(1): 4-9. doi: 10.1097/WCO.0000000000000781. PMID: 31809332. |
| [2] | Menon T, Kalra DK. Sleep Apnea and Heart Failure-Current State-of-The-Art. Int J Mol Sci. 2024 May 11; 25(10): 5251. doi: 10.3390/ijms25105251. PMID: 38791288; PMCID: PMC11121476. |
| [3] | Straten A, van der Zweerde T, Kleiboer A, et al.. Cognitive and behavioral therapies in the treatment of insomnia: a meta-analysis. Sleep Med Rev 2018; 38: 3–16. doi: 10.1016/j.smrv.2017.02.001. |
| [4] | Sudden death in individuals with obstructive sleep apnea: a systematic review and meta-analysis. Heilbrunn ES, Ssentongo P, Chinchilli VM, Oh J, Ssentongo AE. BMJ Open Respir Res. 2021; 8:0. doi: 10.1136/bmjresp-2020-000656. |
| [5] | R otenberg BW Trends in CPAP adherence over twenty years of data collection: A flattened curve / BW Rotenberg, D. Murariu, KP Pang // Journal of Otolaryngology - Head and Neck Surgery. - 2016. - Vol. 45. - No. 1. - P. 1-9. |
| [6] | Lyons MM, Bhatt NY, Pack AI, Magalang UJ. Global burden of sleep-disordered breathing and its implications. Respirology. 2020 Jul; 25(7): 690-702. doi: 10.1111/resp.13838. Epub 2020 May 21. PMID: 32436658. |
| [7] | Linz B, Norup Hertel J, Hendriks J, Saljic A, Dobrev D, Baumert M, Jespersen T, Linz D. Sleep apnea and atrial fibrillation: challenges in clinical and translational research. Expert Rev Cardiovasc Ther. 2022 Feb; 20(2): 101-109. doi: 10.1080/14779072.2022.2036606. Epub 2022 Feb 14. PMID: 35094618. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML