Urinov Muso Boltayevich, Tulayev Mirzohid Jalolovich
Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Urinov Muso Boltayevich, Bukhara State Medical Institute, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
This study was devoted to the assessment of the neurological status of patients with chronic obstructive pulmonary disease (COPD). The study included 120 patients, and their cognitive functions and psycho-emotional state were analyzed. The results showed that with the progression of the disease, patients experience memory and attention disorders, irritability, fatigue, and psycho-emotional instability. Especially in severe stages of COPD, respiratory failure and hypoxia negatively affect the central nervous system, causing aggravation of neurological changes. The results of this study indicate the need for complex therapy of COPD and serve as the basis for developing measures aimed at improving the overall quality of life of patients.
Keywords:
Chronic obstructive pulmonary disease (COPD), Neurological disorders, Cognitive decline, Hypoxia, Psycho-emotional changes, Respiratory failure, Stages of COPD
Cite this paper: Urinov Muso Boltayevich, Tulayev Mirzohid Jalolovich, Clinical Indicators of Studying Patients with Chronic Obstructive Pulmonary Disease with Cerebral Circulation and Cognitive Function Disorders, American Journal of Medicine and Medical Sciences, Vol. 15 No. 2, 2025, pp. 443-446. doi: 10.5923/j.ajmms.20251502.36.
1. Introduction
Chronic obstructive pulmonary disease (COPD) is a disease characterized by a partial irreversible limitation of airflow, as defined by the WHO. The airflow limitation is usually progressive and is caused by an abnormal inflammatory response of the lung tissue to irritation by various pathogenic particles and gases. [1]COPD is currently a very urgent problem due to the steady increase in the number of cases. Thus, the prevalence of this pathology in our country is 16 people per 100,000 population. [6] At the same time, due to the unfavorable environmental situation and the prevalence of smoking, the number of people with COPD is increasing every year. A large number of patients are observed in developing countries. [2]Recently, COPD has been considered a systemic disease in which many organs and systems are involved in the pathological process, and the study of systemic effects in this pathology is actively developing. In patients with COPD, systemic reactions are formed under the influence of inflammatory activity of lung tissue cells and tissue hypoxia. [3] Among the risk factors in this case, tobacco smoking, industrial pollutants, as well as genetic factors predisposing to the development of systemic reactions, and a number of others are being studied. [4,5]The purpose of the study. The main goal of this study is to study the neurological changes associated with chronic obstructive pulmonary disease (COPD) and to determine the degree of their impact at different stages of the disease. In particular, the decline in cognitive functions of patients, nervous and psycho-emotional disorders, as well as the impact of respiratory failure on brain activity will be analyzed.
2. Material and Methods of the Study
The study involved 120 patients (52 women and 68 men) with a diagnosis of COPD at various stages. The average age of the patients was 56.3±12.4 years. The control group consisted of 78 people (43 men and 35 women) aged 40 to 70 years, without COPD, mental disorders and endocrine pathologies, and without signs of organic brain damage. The control group did not differ significantly from the experimental group in terms of gender and age composition. The study was conducted on the basis of the clinics of the Military Medical Academy No. 1 for advanced training of doctors, military field therapy and nervous diseases.
3. Research Result
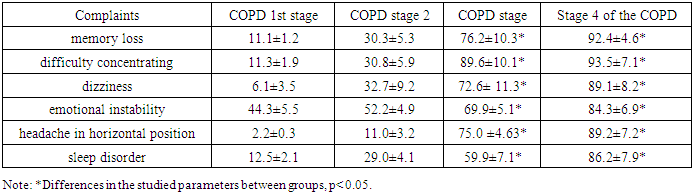
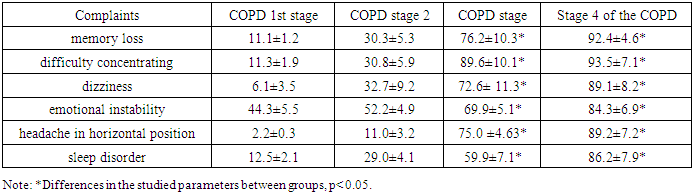
In chronic hypoxia in COPD, as a result of respiratory failure, venous congestion in the brain tissue occurs, weakness of the respiratory muscles, brain neurons are affected. As a result of the studies, data were obtained showing that the initial stages of the disease were characterized by complaints of irritability, fatigue, fatigue, especially in a stuffy room, occurring after psycho-emotional stress (Table 1). However, these phenomena were not permanent and, as a rule, passed spontaneously after rest. As the disease progressed, with increased respiratory failure and the formation of cerebral venous insufficiency, patients complained of headaches (75,0 ± 4.6 and 89.2 ± 7.2% of cases in COPD stages 3 and 4), bursting in nature, usually diffuse, occurring in the morning, with a long horizontal position, accompanied by dizziness, tinnitus, insomnia, decreased performance, sleep disorders. Patients reported increased irritability, and some of them experienced anxiety, irrational fears, hypothymia, memory impairment, inattention, and difficulty concentrating. Emotional instability was noted in 69.9 ± 5.1% of patients and in 84.3 ± 6.9% of patients with stages 3 and 4 of COPD.Table 1. Complaints of patients with COPD at different stages, including
 |
| |
|
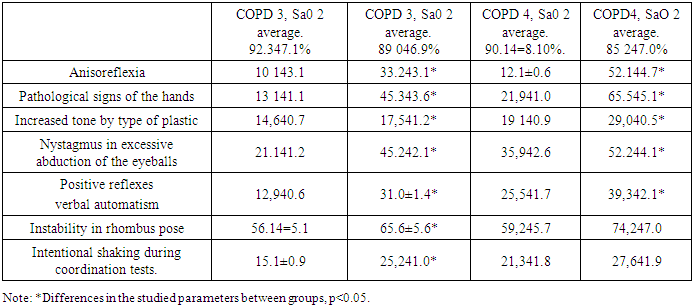
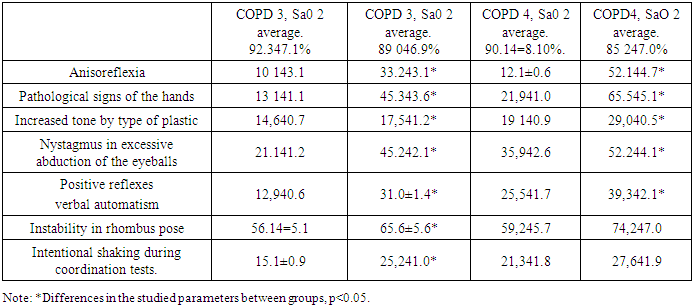
When assessing the neurological status of patients with COPD, the formation of syndromes of varying severity was observed, depending on the stage of the disease. Thus, in the early stages of COPD, the formation of permanent neurological deficit was not observed in the neurological status. In patients with COPD stage 3, neurological symptoms appeared with increasing respiratory failure. Thus, coordination disorders, anisoreflexia, expansion of reflexogenic zones were detected in 64% of people, pathological hand signs were detected in 22% of those examined, and an increase in muscle tone of a plastic type was observed in 23% of patients. It should be noted that in patients with a blood saturation level below 89.0 ± 6.9%, pathological changes were significantly more pronounced according to pulse oximetry. Neurological deficit in these patients was manifested as a combination of ataxic, pyramidal and extrapyramidal disorders. The most common complaints in this category of patients were headache, dizziness, confusion, inattention, decreased memory for recent events, and limitation of daily activities.Similar changes were observed in patients with stage IV of COPD, but their severity was higher. In people of this group, ataxic syndrome was manifested in the form of a decrease in the finger-nose test, finger-hammer test, finger test, Romberg position (arterial blood saturation below 90% - 74.2 + 7.0% of cases, above 90% - 59.2 + 5.7%). In 26% of patients with this syndrome, there was a slight intention tremor and nystagmus during excessive abduction of the eyeballs. In patients with stage IV of COPD with blood saturation below 90%, pathological signs of the hand, for example, Rossolimo and Zhukovsky symptoms, were observed in 65.5 + 5.1% of cases. Anisoreflexia was observed in 45% of patients with pyramidal insufficiency. Increased tone of the plastic type was observed in 31%, tests for brady-oligokinesia were negative. In the neurological status, a combination of pyramidal, extrapyramidal and ataxic syndromes was noted. In this sample, patients often complained of dizziness, morning headache, prolonged exposure to a horizontal position, mild swelling in the periorbital area and increased by injection of conjunctival vessels. Patients often complained of memory impairment, impaired attention, inattention, difficulty concentrating, difficulty walking due to episodes of dizziness, periodic falls, and one of the subjects experienced episodes of loss of consciousness during a coughing attack.Table 2. Frequency of neurological syndromes in patients with stage III and IV COPD depending on blood saturation level (%, mean ± SD)
 |
| |
|
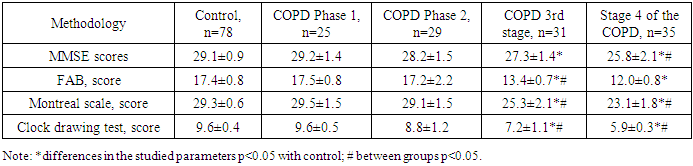
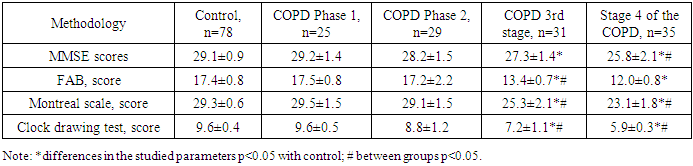
During the work, we diagnosed a state of higher cortical functions in all patients. At the same time, in the early stages of the disease, according to the results of FAB MMSE, no pathological changes were detected, but in the later stages of COPD, with the development of the disease, certain changes occurred in the central nervous system. These pathological changes were especially pronounced in patients with hypoxia. The main data obtained as a result of neuropsychological tests are presented in Table 3.Table 3. Dynamics of indicators characterizing cognitive functions of patients with COPD and the control group, mean ± SD
 |
| |
|
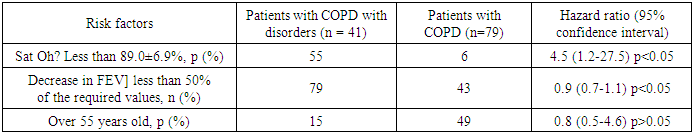
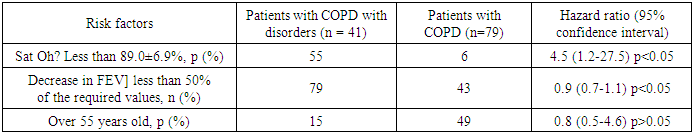
The results of neuropsychological examination of patients with stages 1 and 2 of COPD did not differ significantly from the data obtained in the control group. Among patients with stage 3 COPD, with a blood saturation level of 89.0±6.9% and a 1 SMNCHH level less than 50% of the predicted, the most common were apathy, difficulty concentrating, impaired conceptualization, simple and complex choice reactions. Thus, the average score on the MMSE scale was 27.3 ± 1.4 points, the greatest difficulty in functioning was the seven-point subtest. FAB results were 13.4±0.7 points, which indicated the presence of frontal dysfunction in such patients. Montreal scale scores averaged 25.3±2.1 (p<0.05) points. The results of the clock drawing test also differed significantly from those obtained in the control group and averaged 7.2±1.1. However, the results of these tests in patients with hypoxemia were significantly lower than in patients with normal blood saturation levels.In the fourth stage of COPD, when respiratory disorders reach maximum severity, moderate cognitive impairment is formed with weakness of the respiratory muscles, chronic hypoxia and cerebral venous insufficiency. The indicators on the MMSE scale were 25.8±2.1 points. As in patients with COPD stage 3, the greatest difficulty in performing was the subtest of reading sevens. The average results on the FAB scale were 12.0±0.8 points, which significantly differed from the data obtained in the control group.In patients with stage 4 of COPD, SaO 2 was below 85.2 ± 7.0%, in 94.2 ± 5.6% of cases, difficulties in forming concepts were observed, in 65.6 ± 3.4% of cases, speech fluency was impaired, in 62.4 ± 4.8% of patients, the correct execution of two movements (dynamic praxis) was observed., in 31.2 ± 6.9% they were able to correctly perform only a number of movements. The greatest difficulties were observed in the correct execution of the “complex choice reaction” subtest. The results of the Montreal scale also differed significantly from the data obtained in the control group and amounted to 23.1 ± 1.8 points. The clock drawing test also showed the presence of disorders in higher cortical functions. At the same time, there is a violation of independent drawing with the preservation of the ability to put the hands on the ready dial, which reflects the disorder in the planning processes. It should be noted that patients with low blood saturation performed the tasks worse A. Patient M. 55 years old, COPD stage 3, BaOg 89%. Clock drawing test 6 points. B. Patient N., 56 years old, COPD stage 3, BaOg 94%. Clock drawing test: 8 points. B. Patient K. 62 years old, COPD stage 4, BaOg 84%. Clock drawing test 4 points.We studied the possible risks of the onset and development of cognitive impairment in patients with COPD. Using the Winpepi technique, it was shown that patients with COPD have a higher risk of developing cognitive impairment. Thus, the risk ratio (Odds Ratio, OR) was 2.5 at p<0.05 (confidence interval (CI) 1.2 to 6.1). The risk of cognitive impairment increased by an average of 4.5 times with decreasing blood saturation (p<0.05, CI 1.2-27.5). The risk of developing cognitive impairment in patients with COPD did not change with decreasing FEV (OR 0.9; p<0.05; CI 0.7-1.1). A strong correlation was found between the degree of cognitive impairment and decreased blood oxygen saturation in patients with COPD (r = 0.6; p<0.001). A comparison of the severity of cognitive impairment and the age of patients with COPD did not reveal a correlation between these indicators (r = 0.18; p> 0.05) (Table 4).Table 4. Risk of cognitive impairment in the presence of various factors
 |
| |
|
Nocturnal episodes of apnea, hypopnea, and respiratory failure primarily affect the functions of the central nervous system. In this case, phylogenetically younger structures, such as the cerebral cortex, are primarily affected. The results of a survey of the severity of daytime sleepiness in patients with COPD are presented.In the early stages of the disease, the level of daytime sleepiness was 3.1±0.3 points, which did not differ significantly from the data obtained in the control group. In the 2nd stage of COPD, the level of daytime sleepiness was 4.5±0.5 points, which also did not differ significantly from the results obtained in the control group. However, with the exacerbation of COPD, in the presence of severe shortness of breath and hypoxemia, patients complain more of drowsiness, dizziness, frequent awakenings at night, and snoring. In patients with COPD stage 3, the test results were 8.9±1.0 points, and in patients with COPD stage 4, the level of daytime sleepiness was 10.9±0.9, respectively.Thus, stages 3 and 4 of COPD are characterized by the presence of moderate to severe daytime sleepiness, which, according to the literature, may indicate nocturnal episodes of hypoventilation. Also, when analyzing the relationship between the degree of arterial blood saturation and the severity of daytime sleepiness in patients with COPD, a strong correlation was found (r=0.45; p<0.05).Thus, in the later stages of the disease, more pronounced changes in the respiratory system occur, the development of compensatory mechanisms and ventilation-perfusion disorders, which can negatively affect the functions of the central nervous system. In patients with pulmonary pathology during REM sleep, breathing is usually deep and frequent, during this stage episodes of hypoxemia can develop due to a decrease in alveolar ventilation; The compensatory mechanism that can increase the degree of hypoxemia is the predominance of superficial stages, which leads to impaired sleep function. Thus, despite sufficient time for sleep, sleep does not fulfill its function, which is why daytime sleepiness is common in patients with OSOS.
4. Conclusions
The results of the study showed that with the development of COPD, neurological and cognitive disorders in patients significantly increase. In stages 3 and 4 of the disease, as a result of increased respiratory failure, impaired cerebral venous circulation, neurological symptoms, decreased memory and attention, irritability and psycho-emotional disorders were observed. Also, a decrease in the oxygen content in arterial blood directly affects the level of cognitive deficit, and cognitive disorders were more severe in patients with low blood oxygen saturation. The results of this study confirm that COPD has a serious impact not only on the respiratory system, but also on the central nervous system. Therefore, complex therapy is of great importance for early diagnosis of patients with COPD and to reduce the complications of the disease.
References
| [1] | Geltser B. I. et al. Chronic obstructive pulmonary disease and cerebrovascular diseases: functional and clinical aspect of comorbidity // Terapevticheskii arkhiv. – 2018. – Т. 90. – №. 3. – С. 81-88. |
| [2] | Lahousse L. et al. Chronic obstructive pulmonary disease and cerebrovascular disease: a comprehensive review // Respiratory medicine. – 2015. – Т. 109. – №. 11. – С. 1371-1380. |
| [3] | Yin M. et al. Patterns of brain structural alteration in COPD with different levels of pulmonary function impairment and its association with cognitive deficits //BMC pulmonary medicine. – 2019. – Т. 19. – С. 1-10. |
| [4] | Areza-Fegyveres R. et al. Cognition and chronic hypoxia in pulmonary diseases // Dementia & neuropsychologia. – 2010. – Т. 4. – №. 1. – С. 14-22. |
| [5] | Hjalmarsen A. et al. Effect of long-term oxygen therapy on cognitive and neurological dysfunction in chronic obstructive pulmonary disease // European neurology. – 1999. – Т. 42. – №. 1. – С. 27-35. |
| [6] | Antonelli Incalzi R. et al. Cognitive impairment in chronic obstructive pulmonary disease: a neuropsychological and spect study // Journal of neurology. – 2003. – Т. 250. – С. 325-332. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML