-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(2): 422-427
doi:10.5923/j.ajmms.20251502.32
Received: Jan. 26, 2025; Accepted: Feb. 20, 2025; Published: Feb. 28, 2025

Reconstruction of Jaw Bone Defects Caused by COVID 19 Complications: Literature Review
Boymuradov Shukhrat Abdujalilovich1, Ruziyeva Sitora Sapar Qizi2, Kurbanov Yoqubjon Xamdamovich3
1Professor, Head of Department of Maxillofacial Surgery and Dentistry, Tashkent Medical Academy, Tashkent, Uzbekistan
2PhD Student, Department of Maxillofacial Surgery and Dentistry, Tashkent Medical Academy, Tashkent, Uzbekistan
3PhD, Head of Department of Maxillofacial Surgery and Dentistry, Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Post-COVID complications continue worldwide. The manifestation of these complications in the maxillofacial region causes both mental and physical problems for many patients. When examining the medical records of most patients with osteonecrosis of the bones of the face and jaw, it is noted that they have been infected with coronavirus infection. The issue of restoring defects arising as a result of the removal of bones that have undergone necrosis remains one of the pressing issues for a number of medical professionals worldwide (maxillofacial surgeons, neuropathologists, ENT doctors, ophthalmologists). A number of researchers are using various methods to eliminate post-COVID defects. These methods have their own advantages and disadvantages. In this article, we will review the literature review of the methods used.
Keywords: Osteonecrosis, Dentofacial segment, Thrombotic effect, Temporomandibular joint, Zygoma implant, Pterygoid implant, Prosthesis, Pubmed, Researchgate
Cite this paper: Boymuradov Shukhrat Abdujalilovich, Ruziyeva Sitora Sapar Qizi, Kurbanov Yoqubjon Xamdamovich, Reconstruction of Jaw Bone Defects Caused by COVID 19 Complications: Literature Review, American Journal of Medicine and Medical Sciences, Vol. 15 No. 2, 2025, pp. 422-427. doi: 10.5923/j.ajmms.20251502.32.
1. Introduction
- Currently, the omicron variant of COVID-19 is also increasing rapidly. Omicron is a variant of the SARS-CoV-2 (COVID-19) virus, first identified in November 2021 in South Africa. This virus has the ability to spread faster than other variants and is also highly contagious due to numerous mutations. This virus can also cause coughing, choking, fever, or cold, rapid fatigue, and in some cases, loss of smell and taste. Since omicron subvariants have many mutations, it is difficult to correctly identify and control them. There are several sub variants of the virus. According to statistical data, the last wave originated from the KP.3 subvariant of the fast-spreading omicron variant. After the coronavirus infection, many people experienced various complications. Among them are physical, mental, and neurological problems, among others. These complications can manifest themselves to varying degrees depending on the individual. Problems related to the immune system from post-COVID-19 complications lead to prolonged inflammatory processes in patients and an increased risk of disease recurrence. As a result, complications in the maxillofacial region after COVID-19 infection are unfortunately observed in some patients. These complications are typically accompanied by general inflammation, a decrease in the immune system, or neurological changes. Among the complications affecting the structure of the maxillofacial region after the coronavirus, in particular, osteonecrosis and temporomandibular joint diseases cause serious concern today. According to several scientists, these complications are primarily related to the inflammatory and thrombotic effects of COVID-19, as well as the side effects of drugs such as corticosteroids.The most common complications affecting the structure of the maxillofacial region after coronavirus include COVID-19-associated jaw osteonecrosis (PC-RONC), characterized by spontaneous osteonecrosis of the upper jaw, movable dentofacial segments, purulent fistulas, nasal edema, and open bone necrosis [1,3].The purpose of the study. In reconstruction of post-COVID defects, orthopedic structures are used to restore the functions of chewing and pronunciation after surgery and surgery. Determination of the optimal option for restoring defects in the maxillofacial region caused by coronavirus complications. Study of orthopedic structures made for the elimination and rehabilitation of functional and aesthetic disorders in patients, identification of their advantages and disadvantages.
2. Material and Methods
- During the literature review, researchers read and studied about 100 articles on the elimination of facial bone defects caused by post-COVID complications through publications and applications from Pubmed and Researchgate, Springer. First, let's analyze the methods by which researchers studied the causes of post-COVID defects. Studies have shown that drug-induced jaw osteonecrosis (MDEC) is a serious condition associated with antiresorptive, immunomodulatory, and antiangiogenic drugs, which were previously thought to be related to bisphosphonates, but now includes many other types of drugs. A monoclonal antibody that inhibits the receptor of the immunosuppressant tosylizumab-interleukin-6 (IL-6), which is used to reduce IL-6 activity in conditions such as rheumatoid arthritis and coronavirus. This has raised concerns about the risk of developing MDR in patients after the coronavirus. Subjective examination revealed that a 36-year-old man, after receiving treatment with tocilizumab and dexamethasone, experienced tooth mobility and pain in the upper right cheek. Despite the fact that the patient received antibiotics, the necrotic process continued. This indicates the importance of studying and analyzing the risk of MRON in patients. [8] During the second wave of coronavirus infection, cases of rapid increase in naso-orbitocerebral mucormycosis were also observed, resulting in poor prognosis. Early diagnosis and treatment of mucormycosis are important, as the outcome is sometimes unfavorable (up to 70% of the overall mortality rate). For its diagnosis, some specialists often use computed tomography (CT) and magnetic resonance imaging (MRI). The use of modern methods of examination, such as cone beam computed tomography (CBCT), is also effective. CBCT results indicate indeterminable bone changes in the presence of mucosal thickening of the paranasal sinuses, loss of hard plaque of teeth, erosion, fracture or destruction of bone structures, the border of the cortical plate of the maxillary bone, the cheek, the lower edge of the orbit, the bones of the palate, the walls of the nasal cavity and maxillary sinuses, and sometimes the bone layers. X-ray data from CBCT can also indicate malignant and metastatic bone lesions, osteoradionecrosis, and bisphosphonate-associated osteonecrosis. An accurate diagnosis of mucormycosis can also be made by taking tissue biopsies. During biopsy examination, large-sized, non-septate, and thin-walled gifts in rectangular branching can be seen [14]. However, the cultivation of fungi is a long-lasting process that can lead to delayed start of treatment and consequently to the development of the disease [7]. In reconstruction of solid tissues, radial bone skin flap from the forearm bone (Osteocutaneous Radial Forearm (OCRF)) - horizontal for arch reconstruction, squinting to restore the cartilaginous muscles, or osteotomy to restore the lower orbital plate of the eyeball has been used in scientific research.In addition, the pelvic bone flap (Iliac crest free flap) is used for complete reconstruction of the upper jaw, restoration of the alveolus, cheek bones, restoration of bone loss in the infraorbital region and restoration of the sinus wall in this area, restoration of the external and internal parts of the nose.The subcapular flap is used for restoration in case of complete removal of the upper jaw. Fibulus flaps are used to repair defects arising from the removal of the lower part of the upper jaw along the midline without damaging the upper orbital edge of the upper jaw. In this case, osteointegrated dental implants are required for oral cavity rehabilitation [4,5].According to published data, flaps from the temporal muscle are used to eliminate small and medium-sized defects in the palatine region for soft tissue reconstruction. The radial free flap of the forearm is used to reconstruct small defects in the upper jaw. A flap from a straight abdominal muscle or a wide back muscle, for eliminating defects of large size; Microvascular restoration is used to restore defects where a large upper jaw has been removed but the eyeball has not been damaged [4,5].Several scientists have also proposed reconstruction methods by implanting facial bones. Examples include zygomatic and pterygoid implants. Zygoma implant reconstruction of extensive maxillary defects are a safe, predictable, and cost-effective treatment modality. Implant-supported prosthesis are necessary for loss of soft and hard tissue which often provides support to oral musculature and restore function [13]. For such a prosthesis, zygomatic and pterygoid implants for the rehabilitation of maxillary defects have been reported to be more successful than conventional implants [14,15]. With the introduction of the zygoma implant, prosthesis retention has significantly enhanced, translating into better stability overall [18,19]. In the present case, maxillary defect was reconstructed using zygomatic implants which are rehabilitated with titanium bar-supported prosthesis. A study by Schmidt et al. concluded that combination of zygomatic and standard endosseous implants can be used to reliably reconstruct patients after extensive resection of the maxilla which is in accordance with our case report in which zygomatic implants alone are used to reconstruct the maxillary defect [20].
3. Results
- According to researchers who conducted research in India, 62.5% of patients with these complications were under 50 years old. The majority of patients were men (75%). In relation to the total number of patients, the maxillary defect was observed in 62.5% of patients, while bilateral maxillary defects were observed in 50% of patients (p<0.0001). Eye defect was observed in 37.5% of cases. They used three types of flaps to reconstruct defects during surgical interventions on patients. The average size of the flaps used in the research was 64.75 ± 11.21 sm2, ranging from 48 to 84 cm2. The study included 8 patients, of whom 5 underwent surgical restoration with a free bone-skin flap (OFF), 2 patients with a free superficial skin flap (FF-ALT), and 1 patient with free muscle flaps (FVLM). The superficial skin flap was taken together with the recipient artery in this area, anastomosis was performed with the superficial temporal artery and the facial artery. The duration of the operation ranged from 5 to 8 hours. Patients who underwent reconstruction of the FF-ALT flap and FVLM flap underwent primary donor closure, while all patients who underwent reconstruction of the OFF flap underwent skin transplantation [1,2,3].Prosthetic rehabilitation is a crucial in restoring function and aesthetics, which are important for quality of life in general. The obturator, acting as a barrier, not only helps functionally, but also helps prevent complications such as oroantral contact. Such treatment emphasizes the importance of interdisciplinary assistance in resolving physical and psychosocial aspects, managing complex medical conditions such as mucormycosis. Obturators are prosthetic devices used to close defects caused by the removal of the upper jaw. There are three stages: the immediate (surgical) obturator, installed during surgery. The intermediate surgical obturator is manufactured to promote tissue healing, usually applied 3-4 weeks after surgery. For long-term rehabilitation, a final obturator is placed three months later. This comprehensive approach ensures the proper planning, implementation, and subsequent care of patients with maxillary maxillary resection. Obturators also play an important role in the postoperative care of patients with congenital cleft palate. A number of studies have focused on assessing the effectiveness of chewing and swallowing after prosthetic treatment, as well as the impact of maxillary obturators on the quality of speech. As soon as possible, restoration of chewing and speech functions, which are normal daily activities of the patient, is also important for maintaining the mental health of patients during treatment [12].
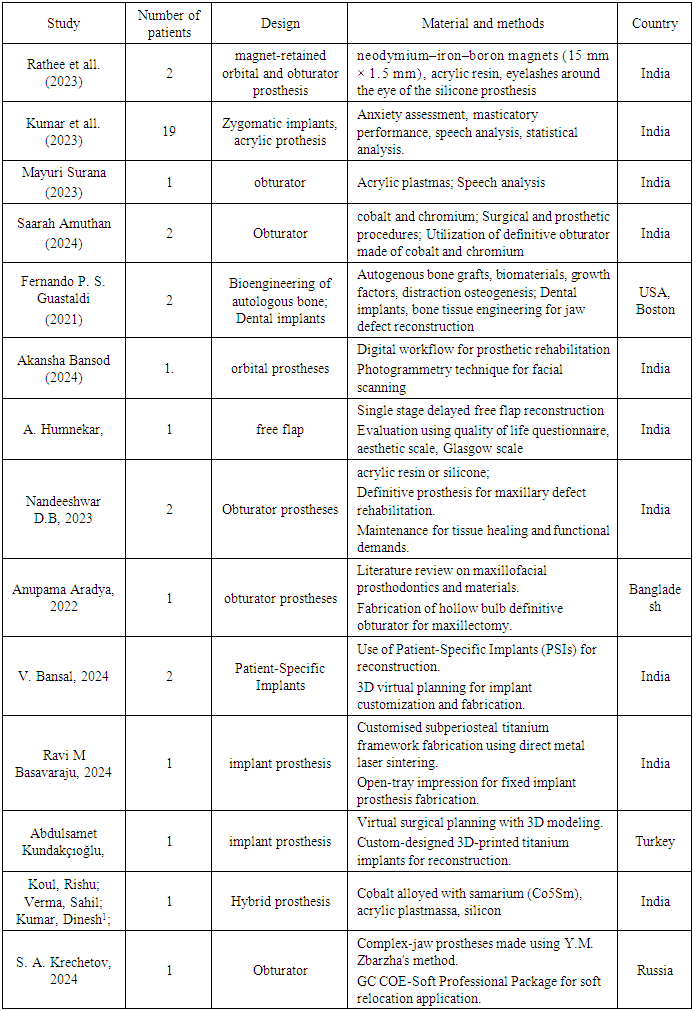
|
4. Discussion
- The COVID-19 pandemic has presented significant challenges to global healthcare systems, including issues in the oral and maxillofacial regions. These complications range from severe systemic effects to localized tissue damage, with some cases resulting in jaw bone defects. The process of reconstructing such defects is complex, influenced by factors such as the severity of the infection, long-term health consequences, and the techniques used for bone tissue reconstruction. While COVID-19 primarily affects the respiratory system, emerging research has shown that it can also cause a variety of oral and maxillofacial complications. Several studies have noted changes in the oral cavity and facial structures, such as osteonecrosis, worsening periodontal disease, and, in severe cases, jaw bone necrosis or defects.Here’s a statistical summary based on the complications caused by COVID-19 in oral and maxillofacial regions, specifically focusing on jaw bone defects, osteonecrosis, and related issues:Prevalence of Oral and Maxillofacial Complications Due to COVID-19: A study conducted by Chrcanovic et al. (2022) found that approximately 10-15% of COVID-19 patients exhibited oral and maxillofacial complications, including jaw bone defects, osteonecrosis, and other dental issues. Another study from the Journal of Clinical Medicine (2021) reported that 5-10% of COVID-19 patients with severe infection developed complications like osteonecrosis or tooth loss due to systemic effects. Osteonecrosis and Bone Resorption: A review by Chrcanovic et al. (2022) indicated that 15-20% of patients who received prolonged corticosteroid treatments during severe COVID-19 developed osteonecrosis or experienced significant bone resorption in the jaw area. In severe cases requiring intensive care, 7-8% of patients on mechanical ventilation for extended periods experienced osteonecrosis or bone necrosis in the oral and maxillofacial region.Systemic Effects Impacting Bone Health: 30-40% of COVID-19 patients suffered from vitamin D deficiency, which can exacerbate bone fragility and increase the risk of fractures, including in the jaw. The prolonged immobility due to severe illness in 40-50% of patients contributed to muscle atrophy and bone demineralization, further increasing the risk of jaw bone complications. Recovery and Reconstruction: In terms of recovery, 70-80% of patients who underwent surgical reconstruction or bone grafting after COVID-19-related jaw bone defects showed positive results. However, 15-20% of these patients required additional interventions due to delayed healing or complications related to the severity of their illness or treatment. These statistics reflect the growing body of evidence regarding the oral and maxillofacial complications caused by COVID-19, highlighting the need for effective management and treatment strategies in affected patients.
5. Conclusions
- Recent literature has highlighted various reconstruction techniques aimed at addressing jawbone defects resulting from post-COVID complications, which were observed in periods between 2020-2024yy. and analyzed n=82(100%) articles with “post-COVID dentistry complications” topic and n=61 (74,4%) articles are performed, contained our dissertation aims. “post-COVID facial and jaw bones complications” topic n=21 (25,6%) articles.These defects, often linked to post-viral osteonecrosis, secondary infections, or impaired vascularization, require tailored approaches depending on the severity and extent of the damage. The primary methods identified include: Autogenous Bone Grafting n=23 (28%): Recognized as the gold standard, autogenous grafts provide excellent biocompatibility and osteogenic potential, particularly when harvested from the iliac crest, fibula, or mandibular symphysis. Alloplastic Materials n=16 (19,5%): Advances in biocompatible materials such as titanium mesh, hydroxyapatite, and bioactive ceramics have enabled precise reconstruction with reduced donor site morbidity; Tissue Engineering n=7 (8,5%): Emerging techniques utilizing stem cells, growth factors, and scaffolds show promise for regenerating bone and soft tissue with minimal invasiveness; Vascularized Free Flaps n=18 (22%): For extensive defects, microvascular free flaps (e.g., fibula or scapula) remain the preferred choice, ensuring both structural integrity and functional restoration; 3D Printing and CAD/CAM Technology n=18 (22%): Integration of digital planning and custom prostheses offers enhanced precision and aesthetic outcomes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML