-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(2): 394-397
doi:10.5923/j.ajmms.20251502.26
Received: Jan. 2, 2025; Accepted: Feb. 1, 2025; Published: Feb. 25, 2025

The Influence of Non-Psychotic Mental and Personality Disorders on the Course of Epilepsy
Hayatov Rustam Batirbekovich, Velilyaeva Alie Sabrievna
Samarkand State Medical University, Samarkand, The Republic of Uzbekistan
Correspondence to: Hayatov Rustam Batirbekovich, Samarkand State Medical University, Samarkand, The Republic of Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The purpose of the study was to study the concomitant pathology of epilepsy and non-psychotic mental and personality disorders in young men and to study the effects of this disease on the patient's quality of life. Materials and methods. The study involved 60 men aged 18-44 years. Results and discussion. In the course of the study, the interpretation of the indicators of 60 patients (100%) according to QOLIE-31 showed that 11 patients (18.3%) rated their quality of life as very low. Low and average quality of life data were determined in 18 (30%) and 21 (35%) patients, respectively. In 10 (16.7%) patients, the levels were in the range of optimal quality of life. The overwhelming majority of patients who participated in this study were found to have non-psychotic mental disorders in the form of anxiety, concern about their health status, and underestimation of self-esteem. A common nonpsychotic disorder in patients with epilepsy is considered to be an organic personality disorder. Conclusions. 1. This study shows the polymorphism of nonpsychotic psychiatric disorders associated with the diagnosis of epilepsy. 2. It was determined that with an increase in the duration of the disease in young patients with focal seizures, negative affective and personal components become very acute. 3. Mild depressive disorders prevailed in young men.
Keywords: Epilepsy, Non-psychotic mental disorders, Personality disorders, Neuropsychological testing
Cite this paper: Hayatov Rustam Batirbekovich, Velilyaeva Alie Sabrievna, The Influence of Non-Psychotic Mental and Personality Disorders on the Course of Epilepsy, American Journal of Medicine and Medical Sciences, Vol. 15 No. 2, 2025, pp. 394-397. doi: 10.5923/j.ajmms.20251502.26.
Article Outline
1. Relevance of the Study
- Epilepsy is often accompanied by affective and behavioral disorders consisting of depression, anxiety, and psychotic disorders [2,3]. Personality spectrum disorders (HR) are more common in people who suffer from a long period (usually from early childhood) and do not have a positive clinical result from anticonvulsants [4,5]. This premorbid disorder has a bad effect on the quality of life of patients [6]. With correctly selected PSS in monotherapy or adequate polytherapy, remission of epilepsy is achieved only in 50-70% of patients. At the same time, 30-50% of patients begin to develop pharmacoresistant epilepsy (FE).It is generally believed that the difficulty of achieving remission of seizures is associated with two groups of causes or a combination of them. The existence of a gross morphological defect of the brain, genuine pharmacoresistance, a substandard course of the disease, including the existence of irreversible disorders of the mental spectrum are the determining factors and are relevant to the first group. The following group of factors has solvable causes: erroneous definition of the disease, an error in pharmacotherapy tactics or incorrect calculation of the PSS dose, irrational polytherapy, patient's ignorance of the possibilities of epileptology, insufficient patient's compliance with mutual cooperation with the doctor and/or the patient's likelihood of concealing the presence of epilepsy [7].However, when new groups of PSS appear, unpredictable side effects are still likely [8]. Thus, certain PSS are a risk of cognitive and affective disorders [1].The prevalence of this disease in developed countries is 5-10 cases per 1000 population. Based on demographic studies conducted in developed countries, the incidence of epilepsy varies from 0.28 to 0.53 per 1000 population. The prevalence of this pathology in the CIS ranges from 0.96 to 10 cases per 1000 population. The prevalence of epilepsy ranges from 15 to 50 cases per 100,000 populations in various regions of Uzbekistan (on average, 30 per 100,000). In addition, the average incidence in men (53.7 per 100,000) is slightly higher than in women (46.3 per 100,000) [3].Epilepsy is considered one of the most urgent clinical problems and at the same time an interdisciplinary problem directly related to psychiatry, neurosurgery, medical psychology and neurophysiology.This disease has a particular negative impact on all areas of the patient's life, reducing its quality. Quality of life (QOL) in patients with epilepsy, in particular young patients, implies a socially active lifestyle [2].In everyday life, men diagnosed with epilepsy are constantly experiencing discomfort. In general, this is a decline in social and personal ambitions, low self-esteem compared to healthy people, high levels of anxiety and depression. Depression in patients with epilepsy often occurs with symptoms that should be regarded as undesirable effects of antiepileptic drugs, including manifestations of epilepsy as such (sleep disorders, changes in appetite, behavioral disorders, lethargy or excessive irritability, etc.).Premorbid disorders in epilepsy are an extensive heterogeneous group of different conditions, most of which are mental illnesses (personality disorder, dementia, depression, anxiety disorders, psychoses).Affective disorders, anxiety disorders, psychoses, attention deficit hyperactivity disorder, and autism spectrum disorders are often diagnosed along with epilepsy as premorbid diseases. A number of specialists [6,7] consider mental and behavioral disorders to be complications of epilepsy, while other scientists [4] have demonstrated a two-way causal relationship between them.The purpose of the study was to study the concomitant pathology of epilepsy and non-psychotic mental disorders in young men and to study the effects of this disease on the patient's quality of life.
2. Materials and Methods
- The study involved 60 men aged 18-44 years. According to the WHO classification, all the subjects belonged to the group of young people. The average age of the patients was 33.90 ± 2.12 years.Men with significant somatic pathology, acute and chronic, including brain tumors, acute traumatic brain injuries and acute infectious diseases of various etiologies were not included in the study.The study included neuropsychological testing using the quality of life questionnaire for epilepsy-31 (QOLIE-31), the mini-examination of mental state (MMSE) and the International Survey of Personality Disorders (IPDE), based on the Diagnostic and Statistical Manual of Mental Disorders-5, the questionnaire of anxiety by signs of the condition (STAI), the scale of assessment of clinical Dementia (CDR) (Morris J.C., 1993), Hamilton Depression Assessment Scale (HDRS). Electroencephalography (EEG) and EEG video monitoring were used as screening methods.A general examination and determination of basic physical data to exclude actual somatic pathology, including neurological examination, were carried out in accordance with generally accepted methods.We analyzed the QOL of patients with epilepsy, the nature of epileptic seizures, their frequency, duration, including other complaints, medical history, and family history, in order to identify a genetic predisposition to epilepsy. The form of epilepsy and the type of epileptic seizures were determined in accordance with the International Classification of Epilepsy and Epileptic Seizures (International League against Epilepsy, 2017).Correlation analysis (Pearson correlation coefficient) was used to determine the degree and nature of the relationship between the studied parameters. All the differences and correlations mentioned in the article were considered statistically significant at p <0.05.
3. Results and Discussion
- In the course of the study, the interpretation of the indicators of 60 patients (100%) according to QOLIE-31 showed that 11 patients (18.3%) rated their quality of life as very low. Low and average quality of life data were determined in 18 (30%) and 21 (35%) patients, respectively. In 10 (16.7%) patients, the levels were in the range of optimal quality of life (Fig. 1). The results of high quality of life were not determined.
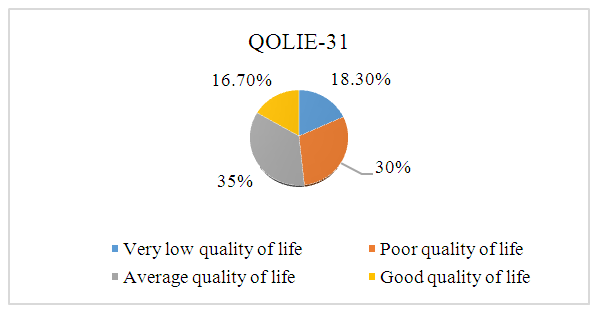 | Figure 1. Assessment of the quality of life of patients with epilepsy |
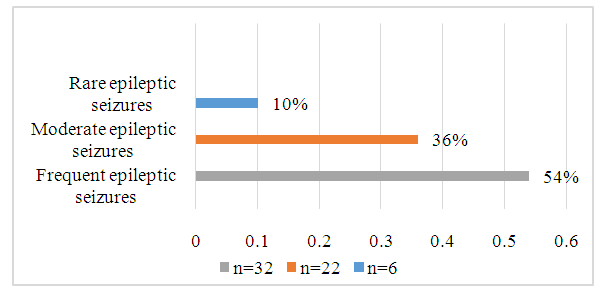 | Figure 2. Frequency of epileptic seizures in patients with epilepsy |
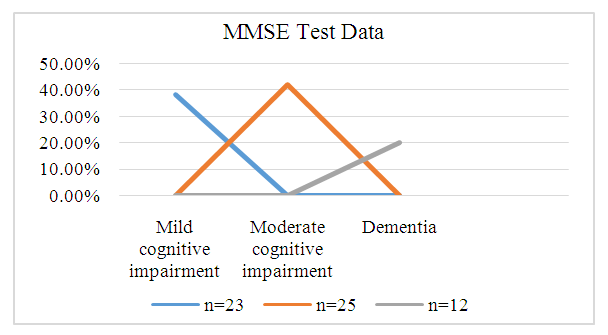 | Figure 3. MMSE test data analysis |
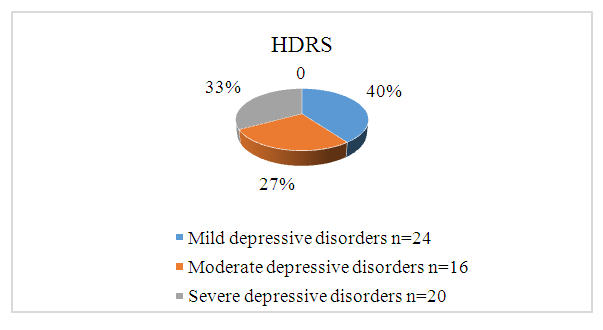 | Figure 4. HDRS scale data analysis |
4. Conclusions
- 1. This study shows the polymorphism of nonpsychotic psychiatric disorders associated with the diagnosis of epilepsy. Premorbid conditions often worsen, and their impact on the patient's health and quality of life becomes the most significant compared to epilepsy.2. It was determined that with an increase in the duration of the disease in young patients with focal seizures, the negative affective and personal components of the response to the disease in the form of neurasthenic, melancholic, apathetic and egocentric manifestations become very acute. Most of the patients had an organic personality disorder. There were also mild and moderate cognitive disorders, including dementia. The weakening of cognitive functions correlates with a decrease in the presence of fast-wave activity in the frontal and parietal regions of the brain (r = 0.45; p < 0.05).3. Mild depressive disorders prevailed in young men. The depth of depression correlated with the duration of the disease (r = 0.39; p < 0.05), introversion (r = 0.33; p < 0.05), age (r = 0.29; p < 0.05) and polytherapy (r = 0.53; p < 0.05).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML