Nishanova Yulduz Xatamovna1, Alisherova Mahliyo Abdunabi Qizi2, Saloni Sajid Maner3, Arshaan Asif Shaikh3, Toyirov Abbos Xamza Ogli4, Bekmuradov Akbarali Toxirjon Ogli4
1Scientific Supervisor Medical radiology Department of Tashkent Medical Academy, Uzbekistan
2PhD Student Medical radiology Department of Tashkent Medical Academy, Uzbekistan
3Student International Faculty of Medicine Tashkent Medical Academy, Uzbekistan
4Master Medical Radiology Department of Tashkent Medical Academy, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
A comprehensive study of 129 patients was conducted to evaluate the role of MRI in the diagnosis and characterisation of brain tumours. MRI demonstrated its superiority in differentiating between benign and malignant brain tumours with diffuse astrocytoma (16.3%) and glioblastomas (13%) being the most frequently encountered malignant legions. Among benign tumours, meningiomas (20.9%) and pituitary adenoma (2.3%) were prevalent. MRI’s ability to provide detail information on tumour, location, morphology and enhancement patterns was critical in planning treatment strategies. The study concludes that MRI is the imaging modality of choice for the evaluation of brain tumours due to its high specificity and detail imaging capabilities. Aim: of this study is to assess the diagnostic value of Magnetic Resonance Imaging (MRI), including advanced imaging techniques such as Dynamic Contrast Enhanced (DCE) MRI and Diffusion-Weighted Imaging (DWI), in characterizing and differentiating between benign and malignant brain tumors. By correlating MRI findings with histopathological results, the study seeks to evaluate the sensitivity, specificity, and overall diagnostic accuracy of MRI in planning treatment strategies for brain tumor patients, with the goal of validating its status as the imaging modality of choice.
Keywords:
Magnetic resonance imaging, Brain tumors, MRI, Neuroimaging, Histopathology
Cite this paper: Nishanova Yulduz Xatamovna, Alisherova Mahliyo Abdunabi Qizi, Saloni Sajid Maner, Arshaan Asif Shaikh, Toyirov Abbos Xamza Ogli, Bekmuradov Akbarali Toxirjon Ogli, Role of Magnetic Resonance Imaging (MRI) in Evaluation of Brain Tumors, American Journal of Medicine and Medical Sciences, Vol. 15 No. 2, 2025, pp. 337-345. doi: 10.5923/j.ajmms.20251502.16.
1. Introduction
Globally, brain tumors represent a significant health concern with substantial variations in incidence and mortality rates across different regions. In 2018, there were approximately 296,851 cases of brain cancers worldwide, accounting for 1.6% of all cancer cases. The highest incidences were reported in Asia and Europe, particularly in Latvia and the former Yugoslav Republic of Macedonia [1].In terms of mortality, about 241,037 deaths were attributable to brain cancers globally in 2018. The mortality rate was highest in Asia and countries like Macedonia and Armenia showed significant death rates related to brain cancers [2].The evaluation of brain tumors presents a complex and multifaceted challenge that requires the integration of clinical examination with advanced imaging techniques [3]. While a thorough neurological examination and the identification of specific symptoms such as headaches, seizures, and focal neurological deficits can guide initial clinical suspicion, imaging remains the cornerstone for definitive diagnosis and characterisation of brain tumors. The advent of various imaging modalities over the past decades has significantly enhanced our ability to visualise and differentiate intracranial pathologies, with Magnetic Resonance Imaging (MRI) standing out as the premier technique for detailed brain imaging [4].Historically, the introduction of imaging modalities like computed tomography (CT) in the early 1970s revolutionized the field by providing cross-sectional images that allowed for better visualization of intracranial structures [5]. CT scans offered advantages in evaluating bony lesions and calcifications due to their high spatial resolution and rapid acquisition times. However, despite these benefits, CT's limitations in soft tissue contrast and exposure to ionising radiation highlighted the need for more advanced imaging techniques.MRI emerged as a pivotal development in neuroimaging, offering unparalleled soft tissue contrast and the ability to acquire multi-planar images without ionising radiation. This modality leverages the differences in proton density and the relaxation properties of tissues, providing detailed images of brain structures. The ability of MRI to distinguish between normal and pathological tissues based on their signal characteristics has made it an indispensable tool in the evaluation of brain tumors.The advantages of MRI over CT in the context of brain tumor evaluation are numerous [6]. MRI provides superior soft tissue contrast, which is crucial for identifying the borders of tumors, their relationship with surrounding brain structures, and any associated edema or necrosis. Moreover, advanced MRI techniques such as diffusion-weighted imaging (DWI), perfusion MRI, and magnetic resonance spectroscopy (MRS) offer additional insights into the tumor's cellular density, vascularity, and metabolic profile, respectively. These advanced imaging modalities aid in tumor grading, determining the extent of the disease, and planning appropriate therapeutic interventions.One of the critical aspects of brain tumor evaluation using MRI is the differentiation between benign and malignant tumors [7]. Benign tumors, such as meningiomas and pituitary adenomas, typically exhibit distinct imaging characteristics that differ from those of malignant tumors like glioblastomas and metastatic lesions. For instance, benign tumors often present with well-defined borders, homogenous enhancement patterns, and minimal perilesional edema. In contrast, malignant tumors may show irregular borders, heterogeneous enhancement, necrotic cores, and significant surrounding edema, indicating aggressive behavior. In addition to morphological assessment, MRI's capability to evaluate the tumor's location within the brain is crucial for treatment planning. Tumors can arise in various regions of the brain, each with its own set of challenges regarding surgical accessibility and potential neurological deficits. MRI provides detailed anatomical localization, which is essential for neurosurgeons to plan the safest and most effective approach for tumor resection. The technique can be time-consuming and is sensitive to patient movement, which can lead to image artefacts. Additionally, the high cost and limited availability of MRI scanners in certain regions may pose barriers to widespread use [8]. However, the clinical benefits of MRI in providing detailed and accurate imaging of brain tumors often outweigh these drawbacks.
2. Materials and Methods
The present study was carried out from 2023 to 2024, at the Republican Specialized Neurosurgery Scientific and practical medical center of the Republic of Uzbekistan. In this study 129 patients with various brain tumors were included where those clinically suspected to have a space occupying Lesion (SOL) in the brain or a history, suggestive of metastatic brain involvement, the inclusion criteria encompassed a wide age range, from 3 to 73 years, to capture a diverse patient demographic. Patient confidentiality was maintained throughout the study and all data were anonymised for analysis. MRI scans were performed using a high field strength MRI scanner (1.5 Tesla) to ensure optimal image, quality and resolution. The MRI protocol for brain tumour evaluation included a combination of standard and advanced imaging sequences such as T1 weighted imaging, T2 weighted imaging, fluid attenuated, inversion recovery (FLAIR), diffusion, weighted imaging (DWI) and post contrast T1 weighted imaging. All MRI scans were reviewed by Vidar Dicom programme. The different characteristic for each lesion, including location, size, and morphology, signal characteristics, contrast enhancement, ema, necrosis, and involvement of adjacent structures were assessed.Statistical data analysis was conducted using the Excel (2007) software application, where parameters such as mean (M), mean standard error (m), standard deviation, and the probability of result reliability according to the t-Student criterion were determined.The chosen threshold for statistical significance was established at p > 0.005.
3. Results
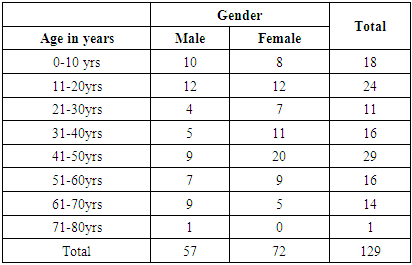
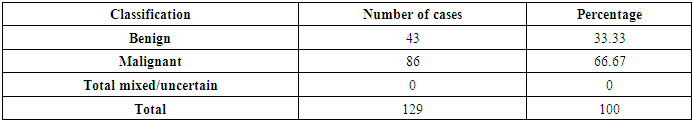
In our study, where majority of the patients were females accounting for 55.81% and male patients accounting for 44.19%. Meningioma is the most common of the present study constituting 20.15% of all cases. Tumours were classified as benign or malignant based on their MRI characteristics and histopathological confirmation when available [9]. The data wherein statistically analysed to determine the prevalence of different tumour types and the diagnostic accuracy of MRI in differentiating between benign and malignant lesions. The sensitivity specificity positive predictive value (PPV), and negative predictive value (NPV) of MRI for calculator for various tumour types [10]. A total of 129 patients (n=129) who made the inclusion criteria were enrolled in the study. The age of the patient in the study ranges from 3 to 73 years with a mean age (x)=36 years. Age wise distribution: Among the patient’s youngest patient was 3 years old and oldest patient was 73 years, 41 to 50 years was the single largest group followed by 11 to 20 years, 0 to 10 years and then 31 to 40 years and 51 to 60 years and then 61 to 70 years and concluding by 71 to 80 years (table 1).Table 1. Age wise distribution
 |
| |
|
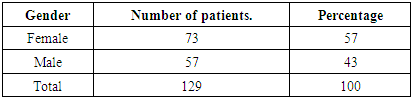
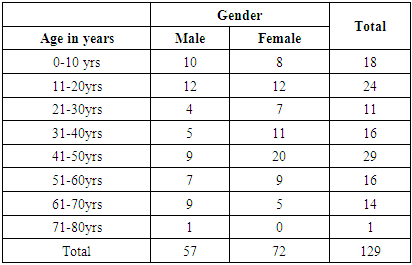
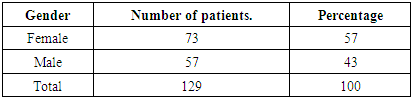
Gender wise distribution: the gender wise distribution of brain tumours in the study, underscores the importance of considering gender as a factor in the diagnosis and management of brain tumours. The slightly higher prevalence of brain tumours in female patients (57%) compared to male patients (43%) see (table 2) suggests potential differences in tumour biology, hormonal influence, and possibly even genetic factor that requires further investigation.Table 2. gender wise distribution
 |
| |
|
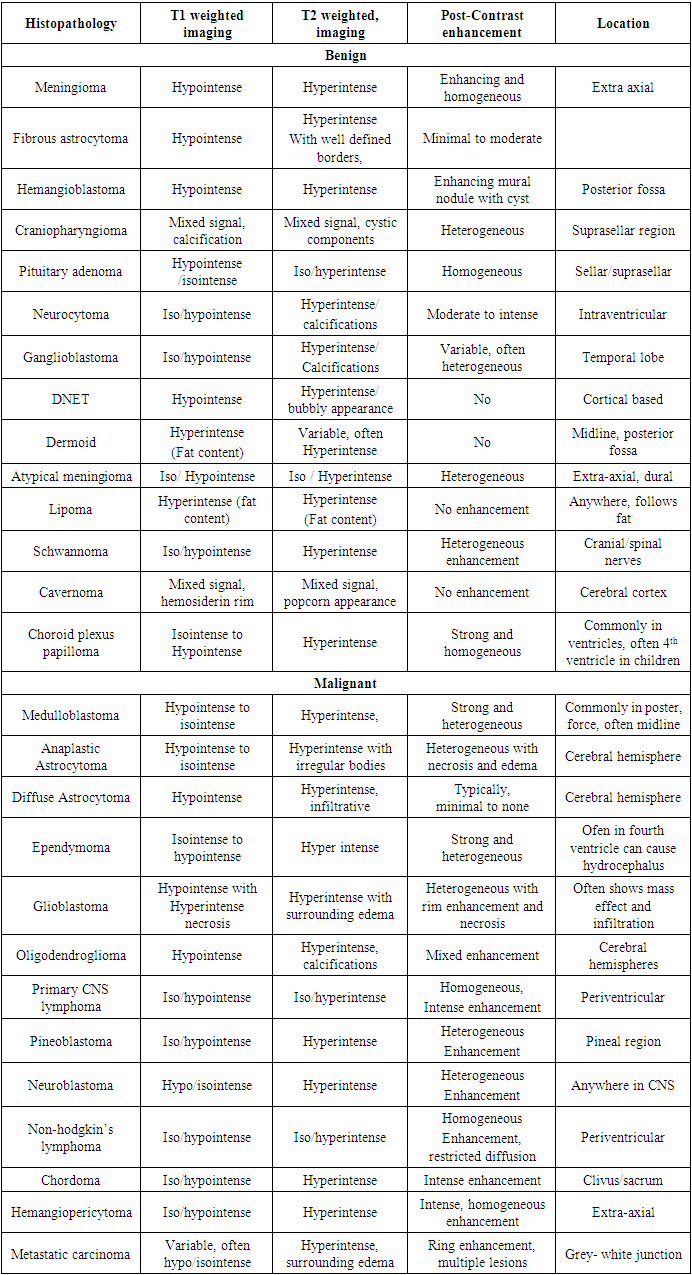
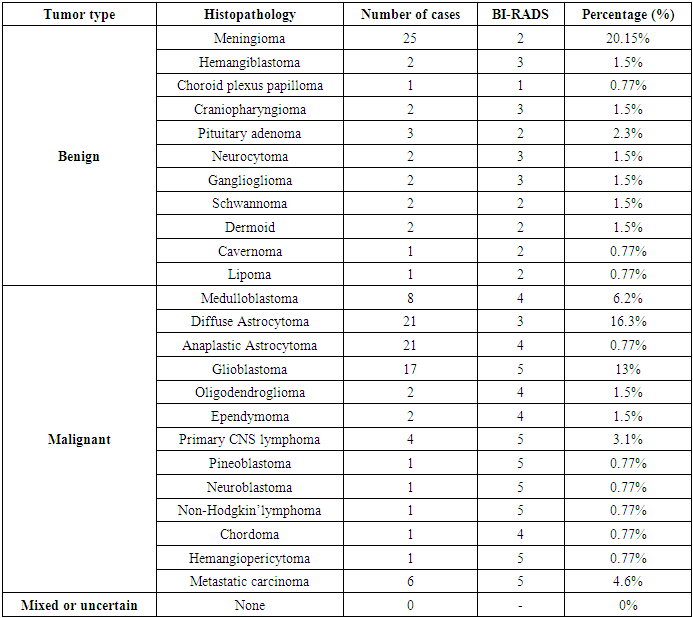
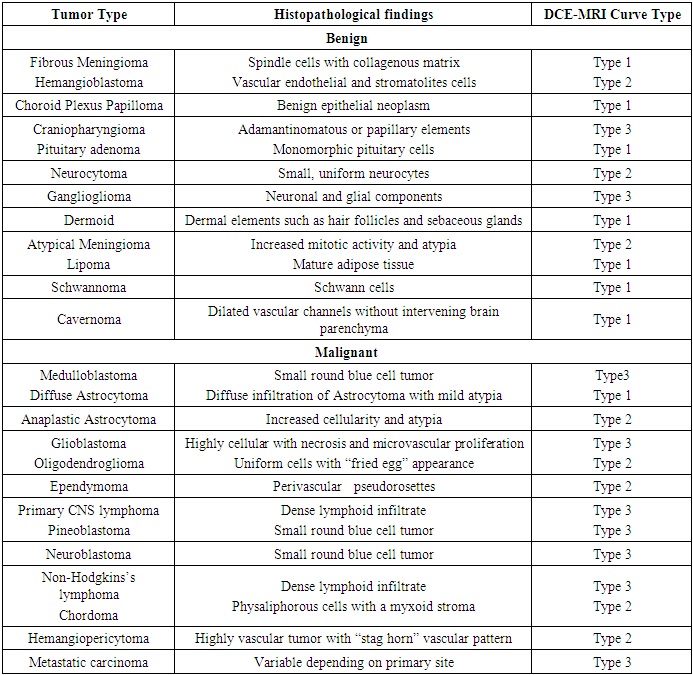
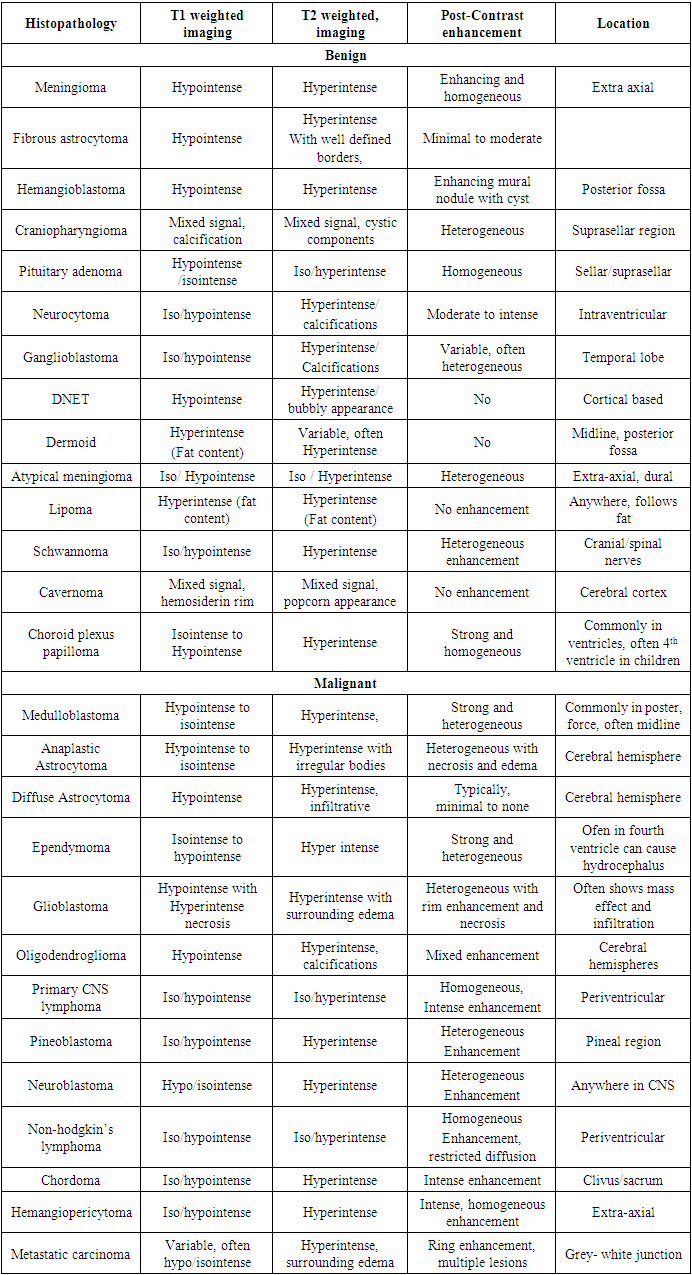
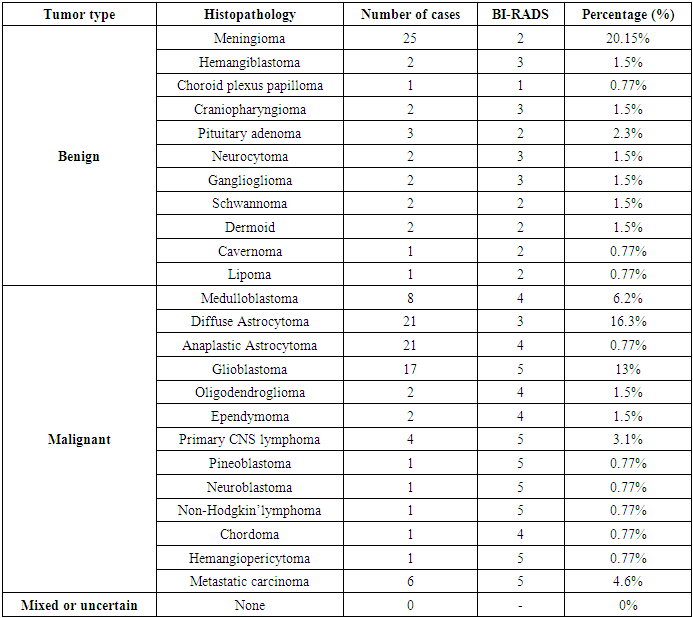
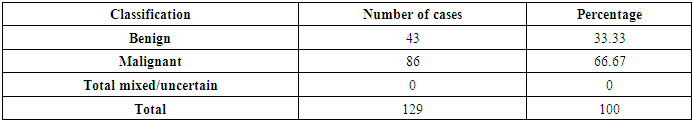
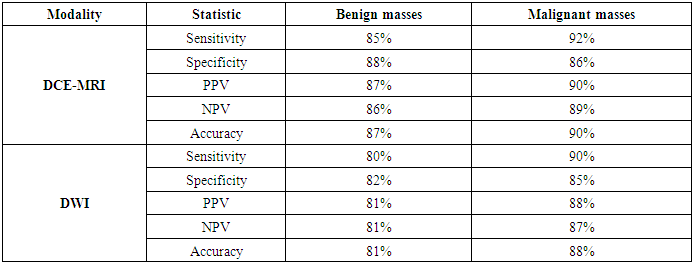
Histopathology and MRI characteristics: The study encompassed a total of 129 patients with 129 cases of brain tumours which were classified into benign and malignant categories based on histopathological examinations (table 4, 5). The MRI characteristics of each tumour type were documented and are summarised (table 3). We examine the association between histological findings and DCE MRI curve types among various tumour types (table 6). The table presents data on different different benign and malignant tumours, their histopathological characteristics, and corresponding DCE - MRI (Dynamic Contrast Enhanced Magnetic Resonance Imaging) curves types. This study also evaluates the effectiveness of Dynamic Contrast Enhanced MRI (DCE-MRI) and Diffusion -Weighted Imaging (DWI) in differentiating between benign and malignant brain tumors. The performance metrics for each modality are summarised in (table 7).Table 3. MRI characteristics with histopathology and location of categorised brain tumors
 |
| |
|
Table 4. Categorised brain tumor cases with histopathology
 |
| |
|
Table 5. Summary
 |
| |
|
Type 1: Persistent Enhancement- gradual and continuous increase in enhancement over time.Type 2: Plateau Enhancement - rapid initial enhancement followed by a Plateau phase.Type 3: Washout enhancement- rapid initial enhancement, followed by a phase indicating possible malignancy.Table 6. Association between histological findings and DCE-MRI curve types among the cases studied
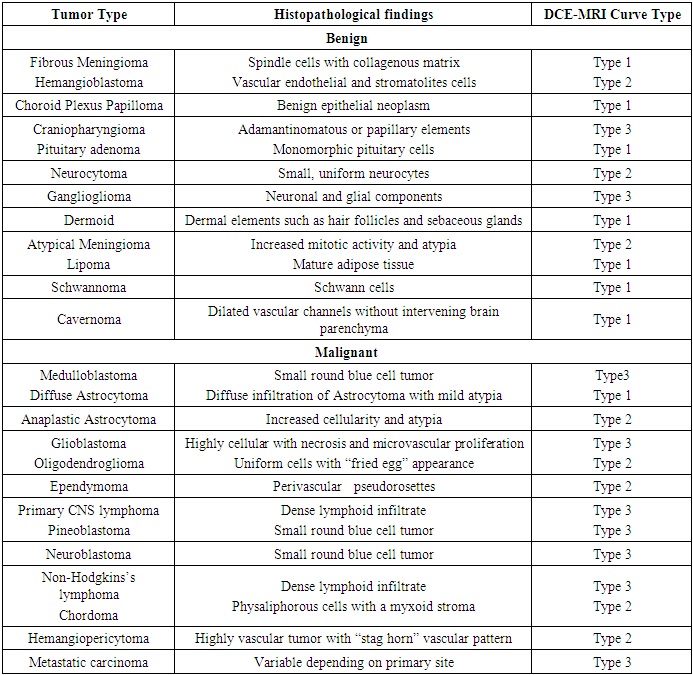 |
| |
|
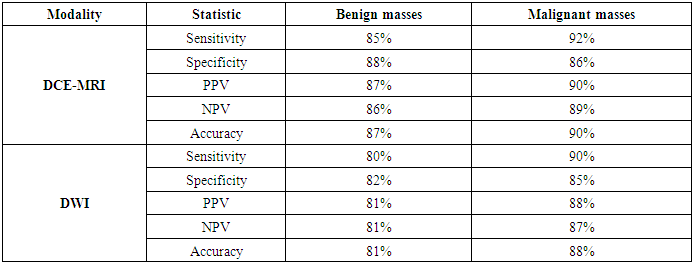
Table 7. Diagnostic value of DCE MRI and DWI in the evaluation of benign and malignant brain masses
 |
| |
|
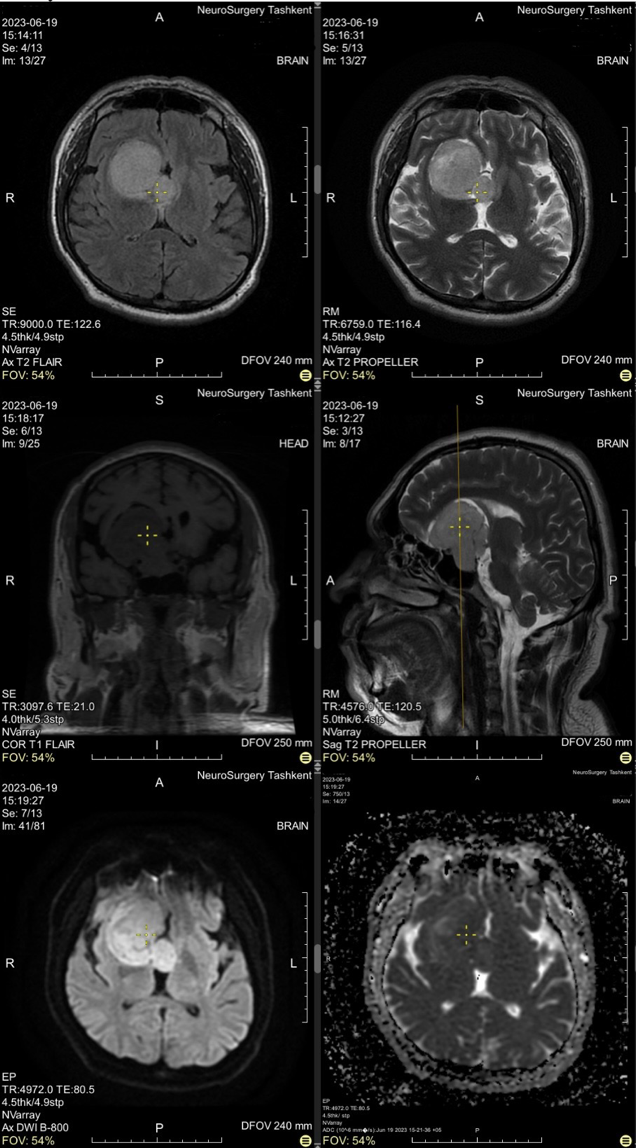
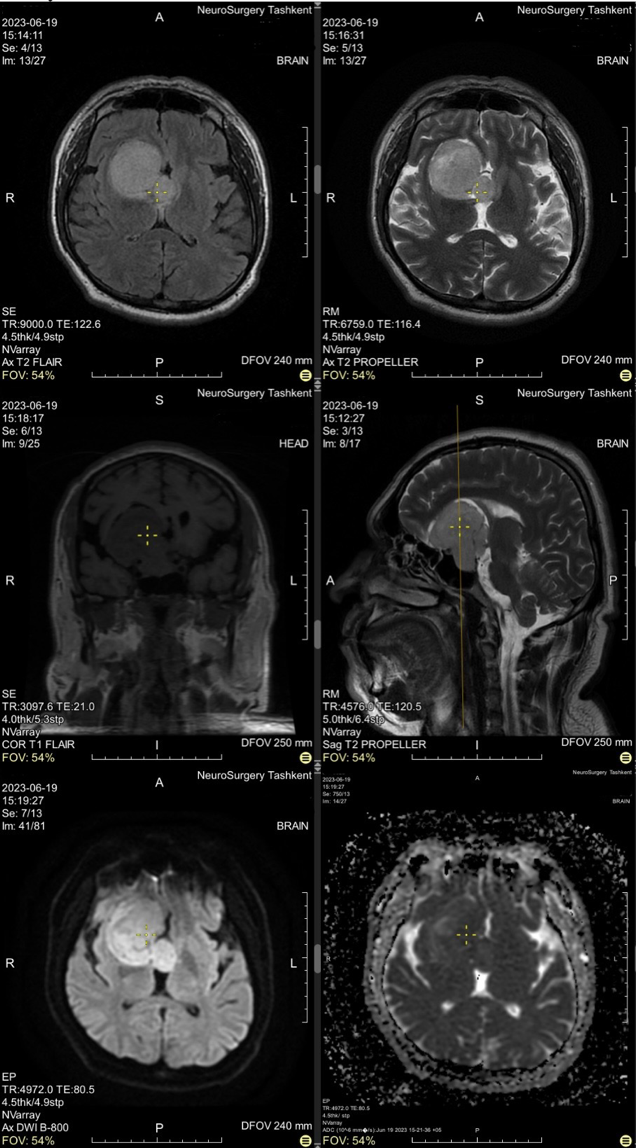
Case gallery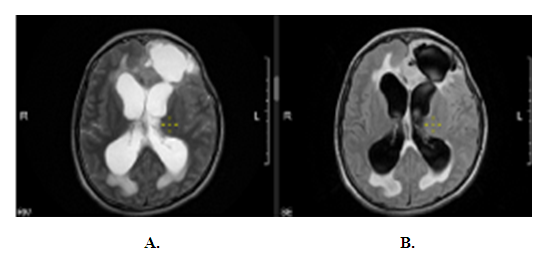 | Figure 1. Astrocytoma – Female aged 18 years. A= T2 Propeller, B=T2 Flair |
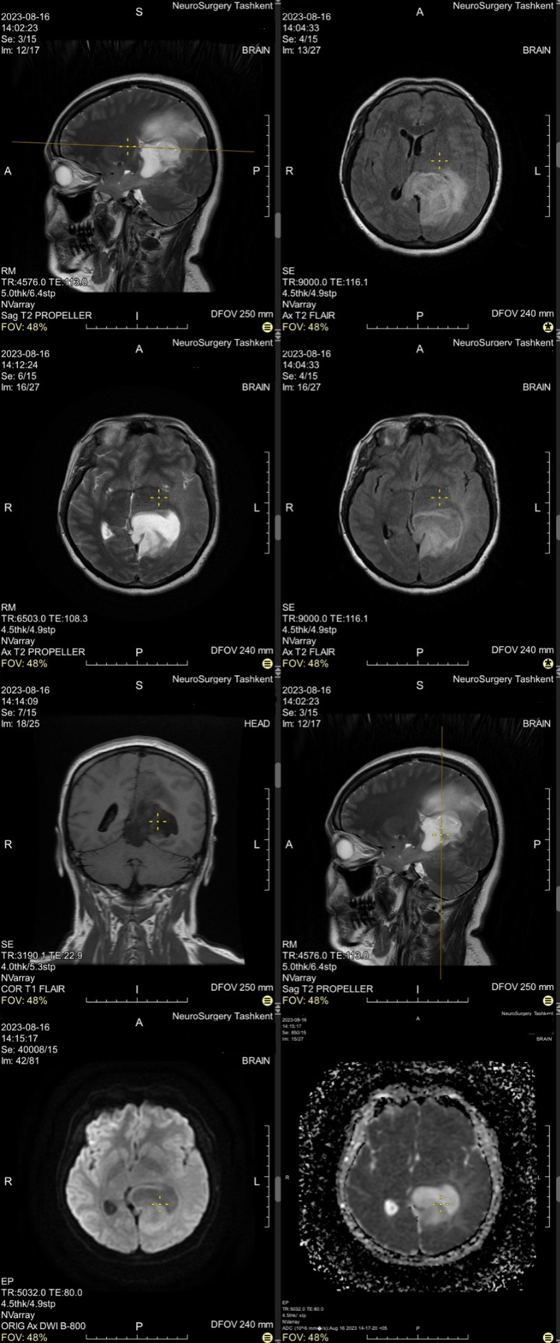
 | Figure 2. Meningioma – Female aged 43 years |
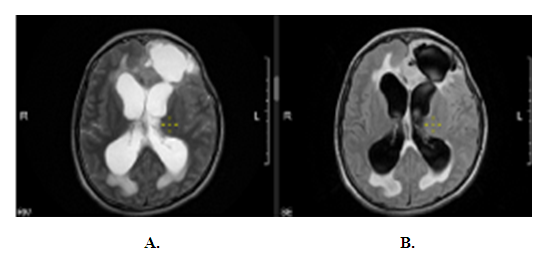
 | Figure 3. Adenoma- Male aged 47years |
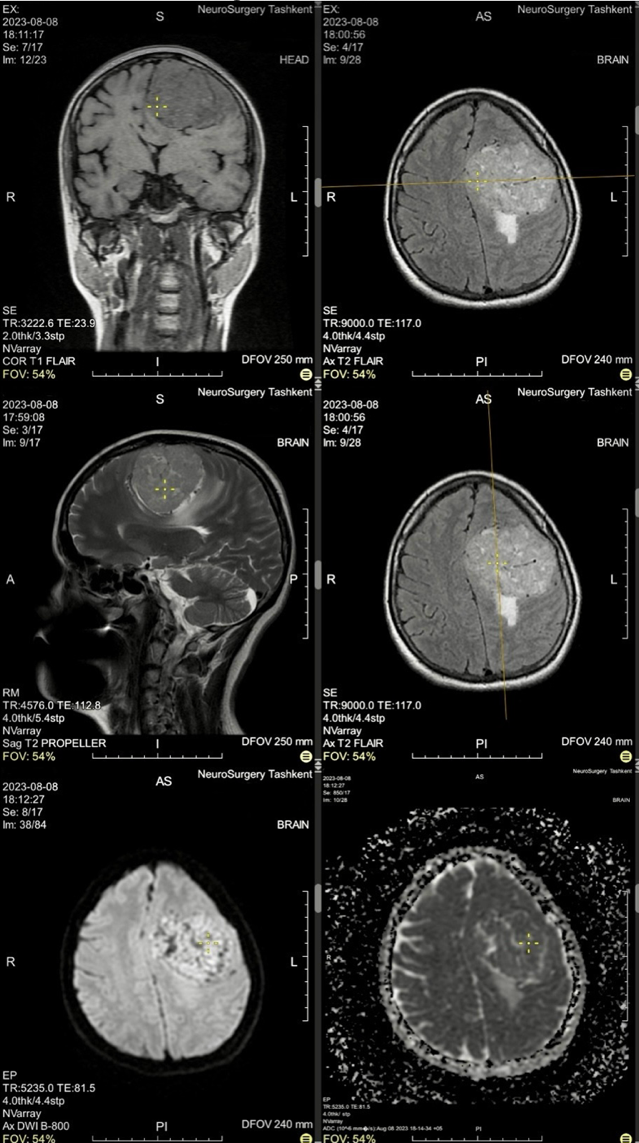
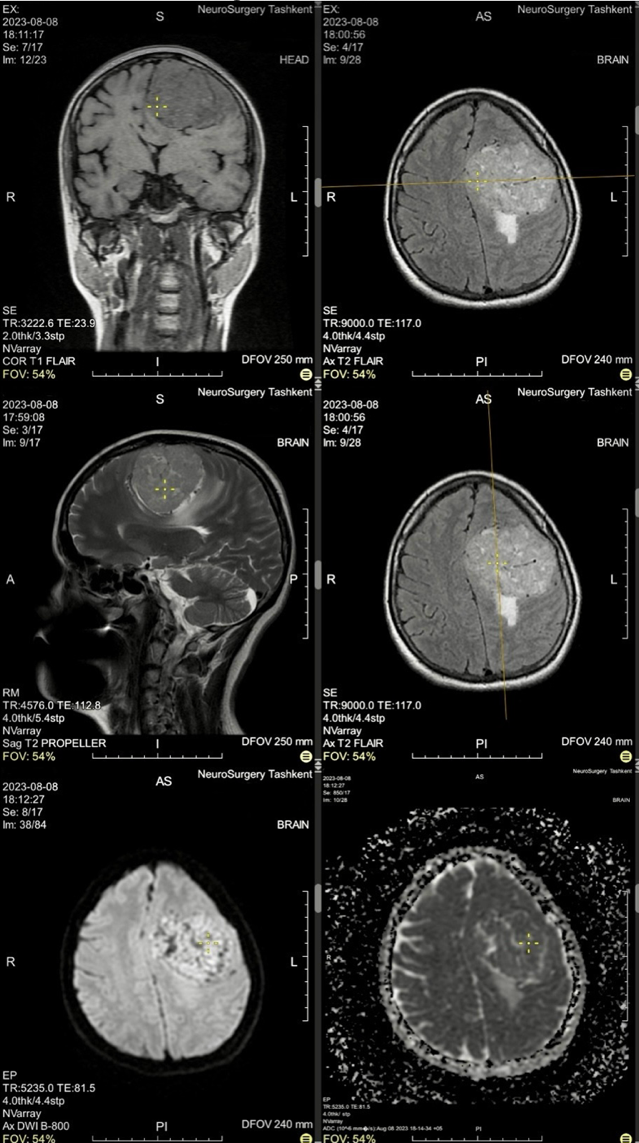
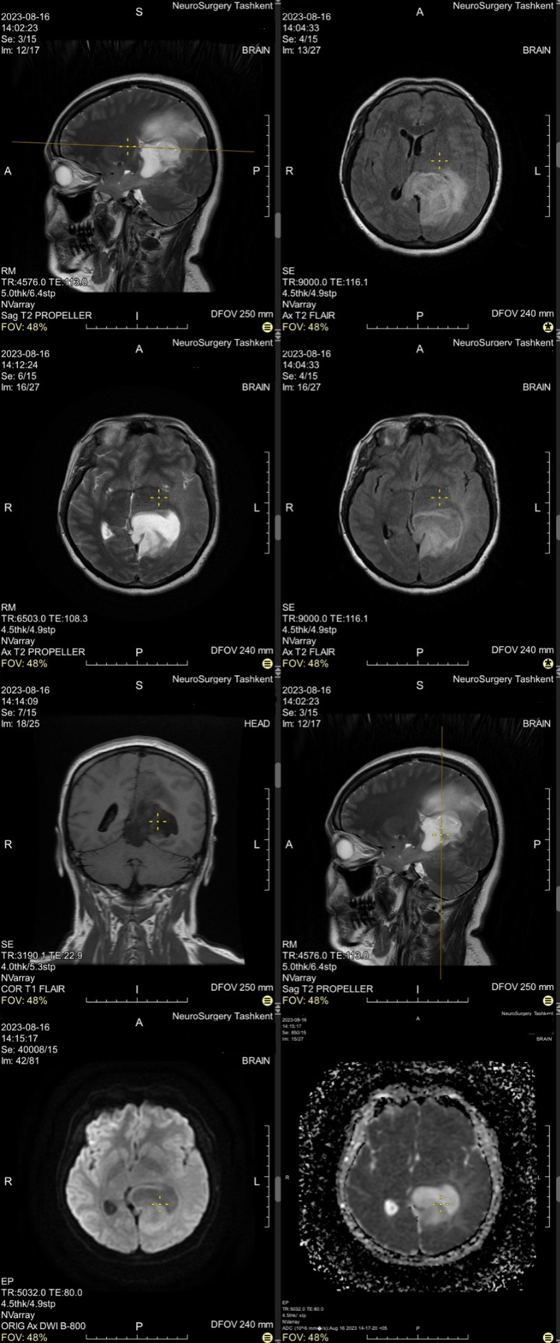
 | Figure 4. Glioblastoma- Female aged 41yrs |
 | Figure 5. Dermoid cyst- 18 years old female |
4. Discussion
Our study aimed to assess the role of MRI in the evaluation and characterisation of brain tumors through a comprehensive analysis of 129 cases. This research reinforces the established understanding that MRI is an indispensable tool in neuroimaging, providing high specificity and detailed imaging capabilities crucial for diagnosing and planning treatment strategies for brain tumors [12]. The age of patients in our study ranged from 3 to 73 years, with a mean age of approximately 41 years. This demographic distribution aligns with the findings of other studies, such as those by Smith et al., which reported a similar mean age of brain tumor patients. The broad age range underscores the need for MRI as a versatile imaging modality capable of catering to both pediatric and adult populations [13]. Our study found a higher prevalence of brain tumors in female patients (57%) compared to males (43%). This gender distribution is consistent with findings in previous research, suggesting potential hormonal or genetic factors influencing tumor development. Further investigation into these gender-specific differences could inform more targeted diagnostic and therapeutic approaches. In terms of tumor characterisation, MRI demonstrated its superior ability to differentiate between benign and malignant brain tumors [14]. Diffuse astrocytoma (16.3%) and glioblastomas (13%) were the most frequently encountered malignant lesions, while meningioma (20.15%) and pituitary adenoma (2.3%) were the prevalent benign tumors.The MRI characteristics observed in our study, such as T1 and T2 weighted imaging, post-contrast enhancement patterns, and advanced techniques like DWI were instrumental in assessing the tumors' morphology and enhancement patterns. For instance, glioblastomas typically exhibited heterogeneous enhancement with rim necrosis, while benign tumors like meningiomas showed well-defined borders and homogeneous enhancement [15]. These imaging features are well-documented in neuroimaging literature and were pivotal in guiding clinical decisions in our cohort. Comparatively, our study's diagnostic accuracy metrics for MRI, including sensitivity (92%) and specificity (86%) for malignant tumors, align with those reported in other studies. The positive predictive value (PPV) and negative predictive value (NPV) for MRI in our study also mirrored those found in the literature, emphasizing its efficacy in minimizing false positives and negatives [16]. The advanced MRI techniques, such as DCE-MRI and DWI, further enhanced diagnostic accuracy. Moreover, our study demonstrated that DCE-MRI had a sensitivity of 92% for malignant masses and 85% for benign masses, with specificity values of 86% and 88%, respectively.
5. Conclusions
The study highlights the indispensable role of MRI in the evaluation of brain tumors. DCE-MRI, with its high sensitivity and specificity, excels in providing detailed vascular information that is critical for distinguishing between benign and malignant tumors and for planning surgical interventions. DWI complements this by offering insights into tumor cellularity, helping to further refine the diagnosis and understand the tumor's behavior.Both modalities have their limitations—DCE-MRI can be time-consuming and prone to motion artefacts, while DWI may not always clearly differentiate between tumor types in regions with complex anatomy[17]. Despite these limitations, the combined use of DCE-MRI and DWI significantly enhances the diagnostic process, providing a comprehensive assessment that is crucial for effective treatment planning.
Abbreviations
PPV- Positive Predictive Value; NPV- Negative Predictive Value.
References
| [1] | Khazaei Z, Goodarzi E, Borhaninejad V, Iranmanesh F, Mirshekarpour H, Mirzaei B, Naemi H, Bechashk SM, Darvishi I, Ershad Sarabi R, Naghibzadeh-Tahami A. The association between incidence and mortality of brain cancer and human development index (HDI): an ecological study. BMC Public Health. 2020 Nov 12; 20(1): 1696. doi: 10.1186/s12889-020-09838-4. PMID: 33183267; PMCID: PMC7664078. |
| [2] | Bray F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries // CA: a cancer journal for clinicians. – 2018. – Т. 68. – №. 6. – С. 394-424. |
| [3] | Ostrom QT, Gittleman H, Xu J, Kromer C, Wolinsky Y, Kruchko C, Barnholtz-Sloan JS. CBTRUS Statistical Report: Primary brain and other central nervous system tumors diagnosed in the United States in 2009-2013. Neuro Oncol. 2016 Nov; 18(suppl_5): v1-v75. |
| [4] | Grover VP, Tognarelli JM, Crossey MM, Cox IJ, Taylor-Robinson SD, McPhail MJ. Magnetic Resonance Imaging: Principles and Techniques: Lessons for Clinicians. J Clin Exp Hepatol. 2015 Sep; 5(3): 246-55. doi: 10.1016/j.jceh.2015.08.001. Epub 2015 Aug 20. PMID: 26628842; PMCID: PMC4632105. |
| [5] | Liguori C, Frauenfelder G, Massaroni C, Saccomandi P, Giurazza F, Pitocco F, Marano R, Schena E. Emerging clinical applications of computed tomography. Med Devices (Auckl). 2015 Jun 5; 8: 265-78. doi: 10.2147/MDER.S70630. PMID: 26089707; PMCID: PMC4467659. |
| [6] | Arora V., Sidhu B. S., Singh K. Comparison of computed tomography and magnetic resonance imaging in evaluation of skull lesions // Egyptian Journal of Radiology and Nuclear Medicine. – 2022. – Т. 53. – №. 1. – С. 67. |
| [7] | Herholz K. et al. Brain tumors // Seminars in nuclear medicine. – WB Saunders, 2012. – Т. 42. – №. 6. – С. 356-370. |
| [8] | Yamasaki F, Kurisu K, Satoh K, Arita K, Sugiyama K, Ohtaki M, Hanaya R. Apparent diffusion coefficient of human brain tumors at MR imaging. Radiology. 2005 Oct; 235(3): 985-91. |
| [9] | Saadeh FA, Mahfouz IM, Abd-Alla MH, Sabry DA, Mahmoud RS. Diagnostic accuracy of diffusion-weighted imaging and dynamic contrast-enhanced MRI in the characterization of brain tumors. Egypt J Radiol Nucl Med. 2020 Dec; 51(1): 1-8. |
| [10] | Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW. The 2007 WHO classification of tumors of the central nervous system. Acta Neuropathol. 2007 Aug; 114(2): 97-109. |
| [11] | Zakhari N, Torres CH, McCrea HJ, Dunning A, Sahgal A, Lo SS, Das S. Multi-modality management of brain metastases. Radiat Oncol. 2017 Dec; 12(1): 30. |
| [12] | Paldino MJ, Barboriak DP. Fundamentals of neuroimaging of brain tumors. Handb Clin Neurol. 2016 Jan; 134: 121-46. |
| [13] | Young GS. Advanced MRI of adult brain tumors. Neurol Clin. 2007 Feb; 25(4): 947-73. |
| [14] | Chung WJ, Chung HW, Shin MJ, Lee SH, Lee MH, Lee JS, Kim MJ, Lee WK. MRI to differentiate benign from malignant soft-tissue tumours of the extremities: a simplified systematic imaging approach using depth, size and heterogeneity of signal intensity. Br J Radiol. 2012 Oct; 85(1018): e831-6. doi: 10.1259/bjr/27487871. Epub 2012 May 2. PMID: 22553293; PMCID: PMC3474004. |
| [15] | Batchelor TT, Betensky RA, Esposito JM, Pham LA, Dorfman MV, Rosenblum MK, Louis DN. Age-dependent prognostic effects of histopathologic subtype, mitotic activity, and necrosis among patients with newly diagnosed glioblastoma: a retrospective study. Cancer. 2004 Nov; 101(9): 2176-83. |
| [16] | Monaghan TF, Rahman SN, Agudelo CW, Wein AJ, Lazar JM, Everaert K, Dmochowski RR. Foundational Statistical Principles in Medical Research: Sensitivity, Specificity, Positive Predictive Value, and Negative Predictive Value. Medicina (Kaunas). 2021 May 16; 57(5): 503. doi: 10.3390/medicina57050503. PMID: 34065637; PMCID: PMC8156826. |
| [17] | Hashem, L.M.B., Gareer, S.W.Y., Hashem, A.M.B. et al. Can DWI-MRI be an alternative to DCE-MRI in the diagnosis of troublesome breast lesions?. Egypt J Radiol Nucl Med 52, 138 (2021). https://doi.org/10.1186/s43055-021-00514-0. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML