-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(2): 302-306
doi:10.5923/j.ajmms.20251502.07
Received: Jan. 15, 2025; Accepted: Feb. 6, 2025; Published: Feb. 8, 2025

The Effect of Varicocele on Semen Parameters in Infertile Men
Mahdi M. A. Shamad1, Lamiaa Osman Ahmed2
1College of Medicine, University of Bahri, Sudan
2Dongola Specialized Hospital, Dongola, Sudan
Correspondence to: Mahdi M. A. Shamad, College of Medicine, University of Bahri, Sudan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Varicocele is a condition involving spermatogenesis and considered among causes of male infertility. Prevalence of varicocele varied considerably between general population and infertile men. Infertility in a male factors such as azoospermia, oligozoospermia, asthenozoospermia and/or teratozoospermia. One of the common causes of male infertility is varicocele. The adverse effect of varicocele on spermatogenesis can be attributed to many factors such as an increased testicular temperature, increased intratesticular pressure and hypoxia due to attenuation of blood flow. Varicocele can be categorized according to severity as first, second, and third grades. Objective of this study was to explore the effect of varicocele on semen parameters in infertile men. This is a descriptive, retrospective study, conducted in the period February to July 2022. It included 54 patients whose detailed records were noted from data available in their files. Data included detailed medical history, clinical examination and testicular Doppler Ultra sound results, and seminal fluid analyses results. Results were analysed using SPSS programme. Results showed that varicocele was confirmed by Doppler U/S in 83.3% of patients, and only 16.7% of patients showed no evidence of varicocele. Left sided varicocele was present in 66.7%, right sided varicocele in only 6.7% and bilateral varicocele was present in 26.7%. Concerning type of infertility, 39 (72.2%) patients have primary infertility and 15 (27.8%) patients have secondary infertility. Of the 39 patients with primary infertility, 31 (79.5%) have varicocele, and 14 of the 15 patients with secondary infertility have varicocele. Seminal fluid analysis showed that sperm count is commonly affected in infertile men. Normal sperm count, shape and motility was seen in 13 (24.1%) patients, apart from one patient all presented with evidence of varicocele. In seminal fluid analysis, the count of sperms 20.4% have oligozoospermia, and 38.9% have azoospermia. Of the 21 patients with azoospermia, 17 have primary infertility and 4 have secondary infertility. Concerning the shape of the sperms, 16.7% have teratozoospermia, 8 of them have primary infertility and one have secondary infertility. Azoospermia was found in 21 (38.9%) patients, of them 13 had severe varicocele, 3 mild varicocele and only 5 had no varicocele. Oligozoospermia was found in 11 (20.4%) patients, of them 5 had severe varicocele, other 5 mild varicocele and only one had no varicocele. Other findings include: teratozoospermia in 16.7%, asthenozoospermia in 20.4%. In conclusion, the study's findings indicate that varicocele is highly prevalent in infertile men and that it is significantly correlated with reduced semen parameters, especially in cases of severe varicocele.
Keywords: Varicocele, Semen, Infertility, Seminal fluid, Infertile men, Semen parameters
Cite this paper: Mahdi M. A. Shamad, Lamiaa Osman Ahmed, The Effect of Varicocele on Semen Parameters in Infertile Men, American Journal of Medicine and Medical Sciences, Vol. 15 No. 2, 2025, pp. 302-306. doi: 10.5923/j.ajmms.20251502.07.
Article Outline
1. Introduction
1.1. Background
- Varicocele is a condition involving spermatogenesis and considered among causes of male infertility. Prevalence of varicocele varied considerably between general population and infertile men. It is important to note that not all men who have varicocele are infertile, but varicocele is identified among infertile males [1]. Infertility rates differ significantly between nations and regions, reflecting the prevalence of avoidable illnesses that might cause infertility. In some areas, particularly in sub-Saharan Africa, up to one-third of couples are infertile and of them approximately 52% suffer from acquired infertility [2]. On the contrary, the percentage of secondary infertility is lowest in Asia and in developed countries; 23% and 29%, respectively [3].Infertility in a couple could be caused by male factors such as azoospermia, oligozoospermia, asthenozoospermia and/or teratozoospermia, or female factors such as tubal occlusion, ovulatory dysfunction, uterine abnormality, peritoneal factors and/or endometriosis [4]. However, the problem could be from the side of the male or the female partner alone or from both partners. Unfortunately, in many societies, especially in the third world countries, culturally only the woman is blamed for childlessness. This explains why the wife is usually left on her own to find the solution to this problem from any source, ranging from spiritual to religious treatment [5].
1.2. Infertility in Males
- The term "infertility" itself means "not fertile," which is the same as sterility, and male infertility is a reproductive system issue. A man who is sterile is completely incapable of becoming a parent. The World Health Organization (WHO) and the American Society for Reproduction Medicine Practice Committee defines infertility as no conception after at least 12 months of regular unprotected sexual intercourse [6]. Permanent (irreversible) infertility or sub-fertility, which lowers the likelihood of a spontaneous conception, are two types of infertility. All sterile males would be regarded as infertile, but not all infertile men are sterile, as an infertile man can father a child with medical assistance or a simple lifestyle modification [7].
1.3. Varicocele in Infertile Men
- One of the common causes of male infertility is varicocele [7]. Tulloch in 1952 first reported that bilateral surgical repair of varicocele in a man with azoospermia resulted in an increase in sperm concentration and a spontaneous pregnancy [8]. The adverse effect of varicocele on spermatogenesis can be attributed to many factors such as an increased testicular temperature, increased intratesticular pressure and hypoxia due to attenuation of blood flow [9]. Varicocele can be categorized as first, second, and third grades [10]. First grade varicocele is considered when enlargement of the venous plexus of spermatic tone is evident only by palpation during the Valsalva manoeuvre. Second grade varicocele is when enlargement of the venous plexus of spermatic tone is evident only by palpation at upright position. In Third grade varicocele the enlargement of the venous plexus of spermatic tone is visually evident. The non-palpable enlargement of the venous plexus of the spermatic tone, may be identified by Doppler Ultra sound, angiography or any other imaging method [11].This paper explores the effect of varicocele on semen parameters in infertile men.
2. Methodology
- This is a descriptive, retrospective study, conducted in a-six-month period, at Khartoum Dermatology and Venereology Teaching Hospital – andrology department, in the period February to July 2022. Ethical clearance was obtained from the relevant bodies. The study included 54 patients whose detailed records were noted from data available in their files. Data included detailed medical history, clinical examination and testicular Doppler Ultra sound results, and seminal fluid analyses results. Results were noted for each individual and the obtained data were put in a spreadsheet and then analysed using SPSS programme. The result was presented, discussed in relation to objectives and compared with previous researches.
3. Results
3.1. General Findings
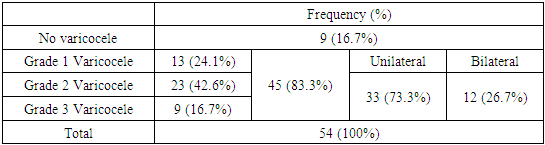
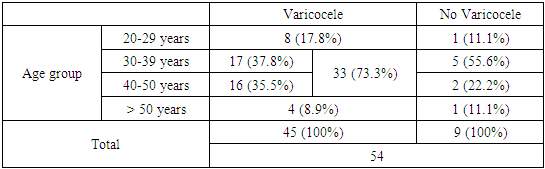
- In the 54 fertile men who are included in this study, the main age was 38.02 (±8.7) years and the most common age group was 30-39 years (22, 40.7%). Varicocele was confirmed by Doppler U/S in 45 (83.3%) infertile patients, and only 9 (16.7%) patients showed no evidence of varicocele. Left sided varicocele was present in 30 (66.7%) patients, right sided varicocele in only 3 (6.7%) patients and bilateral varicocele was present in 12 (26.7%) patients. Most of varicocele patients (23, 42.6%) presented with grade II, 13 (24.1%) with grade I, and only 9 (16.7%) presented with grade III varicocele, grade II and III were considered as severe form of varicocele. Of the 45 patients with varicocele, 33 (73.3%) individuals have unilateral varicocele and 12 (26.7%) have varicocele in both testicles (Table 1).
|
|
|
3.2. The Effect of Varicocele on the Type of Infertility
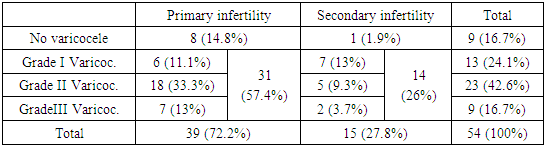
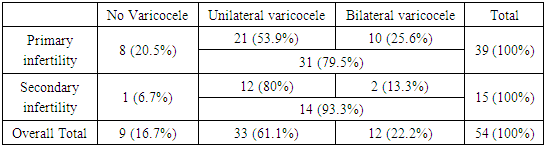
- Of the 45 patients (from the total population of 54) varicocele was seen mainly (33, 73.3%) in the age group of 30 - 50 years. In other hand varicocele was less common in young ages of less than 30 years age (8, 17.8%) which is expected finding. In this age group all have mild varicocele (grade I or II), and none presented with grade III. Varicocele was also seen in infertile patients aged above, from the total of 5 patients, 4 presented with varicocele (2 with grade I, 2 with grade II) and the remaining patient had no varicocele. The few numbers of patients in this age group is explained by that all the study population are infertile men searching for infertility treatment, and seeking of treatment is less common after the age of 50 years (Table 4).
|
3.3. The Effect of Varicocele on Seminal Fluid Parameters
- Seminal fluid analysis showed that sperm count is commonly affected in infertile men. Normal sperm count, shape and motility was seen in 13 (24.1%) patients, apart from one patient all presented with evidence of varicocele. Concerning sperm count, Azoospermia was found in 21 (38.9%) patients, of them 13 had severe varicocele, 3 mild varicocele and only 5 had no varicocele. Oligozoospermia was found in 11 (20.4%) patients, of them 5 had severe varicocele, other 5 mild varicocele and only one had no varicocele. Concerning sperm shape, teratozoospermia was found in 9 (16.7%) patients, of them 6 had severe varicocele, one mild varicocele and 2 patients had no varicocele. Regarding sperm motility, asthenozoospermia was found in 11 (20.4%) patients, of them 6 had severe varicocele, 4 mild varicocele and one patient had no varicocele.
4. Discussion
- This study aimed to explore how the condition affected the semen parameters of infertile men, in order to shed light on the frequency, severity, and influence of varicocele on male infertility. The results add to the literature significant amount of data regarding the role of varicocele in male infertility and show correlations between varicocele and abnormalities of semen, especially in cases of severe varicocele.According to results of the current study, 83.3% of the patients had varicocele, indicating that it was quite common among infertile men. This result is in line with other research that found varicocele is highly prevalent in infertile populations, with prevalence ranging from 35% to 81%. [12]. Varicocele may be associated with infertility because it is 2-3 times more common in men who attend infertility clinics than in men in the general population or with established fertility [13]. The findings of several studies, however, are very debatable. Between 4% and 30% of people in the general population have varicocele [14]. Additionally, the prevalence among infertile men varies from 17% to 41% depending on the study [15]. Having longer course and right-angled insertion into the renal vein, the left testicular vein is more prone to venous reflux, which explains the prevalence of left-sided varicocele (66.7%). Although less frequent (26.7%), bilateral varicocele was also noted, highlighting the necessity of a thorough examination of both testicles in infertile males. According to reports, male factor secondary infertility has a significantly greater prevalence of varicocele than primary infertility, indicating that varicocele leads to a progressive decline in fertility [16]. In the current study, 78.1% of patients with severe varicocele (grades II and III) presented with primary infertility, indicating a substantial link between the two conditions. This implies that because severe varicocele affects spermatogenesis and testicular function, it may have a more noticeable influence on fertility. However, there was no significant correlation found between the type of infertility and mild varicocele (grade I), suggesting that the severity of varicocele is a key factor in determining its clinical consequences. Sperm motility, shape, and count were shown to be often impacted in infertile males with varicocele, according to seminal fluid study. Of the study sample, 38.9% of patients had azoospermia, while the majority (61.9%) had severe varicocele. Similarly, patients with severe varicocele had higher rates of oligozoospermia and teratozoospermia. These results are in line with previous studies that connected varicocele to altered semen characteristics, such as decreased motility, abnormal morphology, and lower sperm count [17]. Varicocele may affect spermatogenesis and the testicular microenvironment, as evidenced by the correlation found between severe varicocele and low semen quality. Some researchers relate the poor sperm concentration to the high rate of germ cell death that is typically seen in those men, while others ascribe the low motility to either the elevated levels of reactive oxygen or to the presence of anti-sperm antibodies [18].Findings of the current study are consistent with the theory that varicocele, especially in its severe form, negatively impacts semen parameters and plays a role in male infertility. This is consistent with the hypothesised mechanisms of infertility caused by varicocele, which include hormonal abnormalities, oxidative stress, and elevated testicular temperature [19]. The findings also emphasise the importance of grading the severity of varicocele, because higher grades were linked to more severe semen abnormalities and primary infertility, the results again highlight the significance of assessing varicocele severity. These results highlight the importance of early detection and treatment of varicocele in infertile males from a clinical point of view. In this study, Doppler ultrasonography was found to be a useful diagnostic and grading technique for varicocele.Varicocelectomy, which has been demonstrated in certain trials to enhance semen parameters and pregnancy rates, should be considered for men who present with infertility, particularly those who have severe varicocele [20]. Furthermore, given the elevated rate of varicocele in this population, routine varicocele screening needs to be incorporated into the assessment of male infertility.
5. Conclusions
- In conclusion, the study's findings indicate that varicocele is highly prevalent in infertile men and that it is significantly correlated with reduced semen parameters, especially in cases of severe varicocele. These results highlight how crucial it is to identify and treat varicocele when it comes to male infertility.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML