-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(2): 295-301
doi:10.5923/j.ajmms.20251502.06
Received: Jan. 13, 2025; Accepted: Feb. 5, 2025; Published: Feb. 8, 2025

Evaluation of Speckle-Tracking Echocardiography in Coronary Heart Disease Patients with Type 2 Diabetes after Revascularization
Sh. M. Ubaydullaeva
Republican Specialized Scientific and Practical Medical Center of Therapy and Medical Rehabilitation, Tashkent, Uzbekistan
Correspondence to: Sh. M. Ubaydullaeva, Republican Specialized Scientific and Practical Medical Center of Therapy and Medical Rehabilitation, Tashkent, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

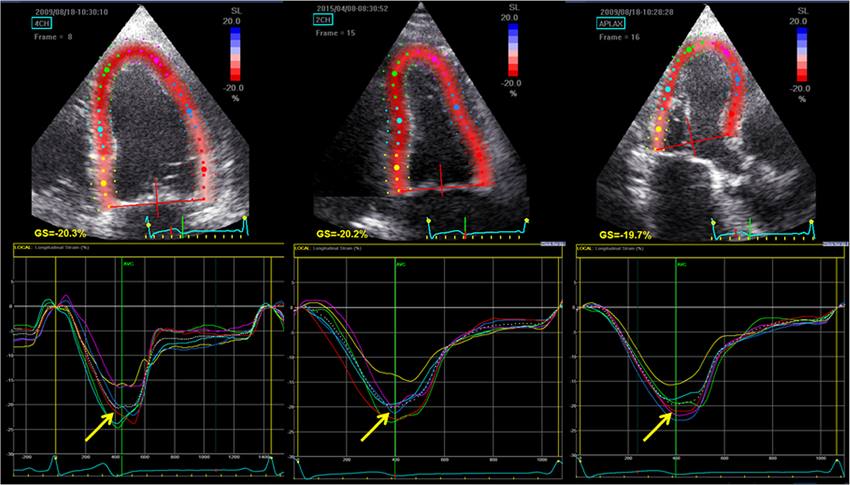
The aim of this study was to evaluate changes in left ventricular contractility and speckle-tracking echocardiography in patients with coronary heart disease and type 2 diabetes before and after percutaneous coronary intervention. Background. According to the World Health Organization, cardiovascular diseases remains the leading cause of death worldwide, with coronary heart disease ranking first among the causes of cardiovascular disease deaths. Around 17.9 million people die annually from cardiovascular diseases, accounting for about 31% of all deaths worldwide. Type 2 diabetes significantly increases the risk of coronary heart disease and other cardiovascular diseases. Our study aims to investigate in detail the left ventricular contractility and changes observed using 2D speckle-tracking echocardiography in patients with coronary heart disease and type 2 diabetes. Material and methods. 132 patients with coronary heart disease were selected for the study. The age of patients ranged from 35 to 68 years, the mean age was 54.8±15.5 years. Results. The groups were randomized according to baseline clinical, anamnestic data and therapy received. On day 1, there was a significant increase in prothrombin time and INR. Inversely, a decrease in PTI and fibrinogen was recorded on the first day and after one month. Such a shift of coagulation hemostasis parameters may be associated with vascular wall damage due to percutaneous coronary intervention. Conclusions. The study of deformation properties indices in patients with coronary heart disease and in patients with type 2 diabetes before and after percutaneous coronary intervention provides an opportunity to assess early efficiency of the performed revascularization, especially in patients with preserved systolic function. The use of myocardial deformation properties before and after percutaneous coronary intervention is a noninvasive predictor of detection and chronic coronary insufficiency and assessment of the efficiency of percutaneous coronary intervention.
Keywords: Coronary heart disease, Type 2 diabetes, Revascularization, Speckle-tracking echocardiography, Percutaneous coronary intervention
Cite this paper: Sh. M. Ubaydullaeva, Evaluation of Speckle-Tracking Echocardiography in Coronary Heart Disease Patients with Type 2 Diabetes after Revascularization, American Journal of Medicine and Medical Sciences, Vol. 15 No. 2, 2025, pp. 295-301. doi: 10.5923/j.ajmms.20251502.06.
Article Outline
1. Introduction
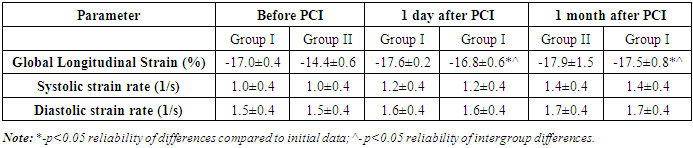
- Coronary heart disease (CHD) and type 2 diabetes (T2D) represent one of the most significant medical and social problems of our time. According to the World Health Organization, cardiovascular diseases remains the leading cause of death worldwide, with coronary heart disease ranking first among the causes of cardiovascular disease deaths. A 2021 WHO report indicates that about 17.9 million people die each year from cardiovascular diseases, which is about 31% of all deaths worldwide [1]. Type 2 diabetes significantly increases the risk of developing CHD and other cardiovascular diseases. The International Diabetes Federation (IDF) predicts in its 2019 report that the number of people with diabetes will reach 700 million by 2045 [2].Patients with CHD and T2D have a higher risk of developing complications such as myocardial infarction, heart failure, stroke and peripheral arterial disease. According to a study published in the journal Diabetes Care in 2020, patients with T2D have two to three times the risk of developing cardiovascular diseases compared to those without diabetes [3]. The combination of CHD and T2D worsens the prognosis and patients' life quality, increases the frequency of hospital admissions and requires high costs for treatment and rehabilitation. Taking into account the high prevalence and severity of consequences of CHD and T2D, especially in their combination, the need for early detection and prevention of cardiovascular events becomes obvious.Echocardiography (EchoCG) is a key tool in modern cardiology for the diagnosis, evaluation and monitoring of various cardiovascular diseases. This ultrasound exam allows to visualize the structure and function of the heart, evaluating chamber size, wall thickness, valve movement and blood flow. The main advantages of EchoCG include non-invasiveness, wide range of applications, accessibility and rapidity, and high informativity. EchoCG plays an important role in early detection of diseases, assessment of disease severity, treatment monitoring and prediction of outcomes [4].It is particularly important to note the relevance of two-dimensional speckle-tracking echocardiography (2D STE) as a more advanced method of assessing myocardial function. This method is based on the tracking of natural ultrasound marks (speckles) in myocardial tissue, which allows to measure and evaluate myocardial deformation in longitudinal, transverse and radial directions. Studies show that the use of 2D STE can detect subclinical changes in myocardial function that are not seen with standard EchoCG. Decreased Global Longitudinal Strain (GLS) may precede clinical manifestations of cardiovascular diseases and may be an early marker of deteriorating myocardial function [5]. 2D STE provides the ability to analyze both global and regional myocardial deformation in detail, which is important for understanding the mechanics of cardiac function and identifying regional abnormalities. Myocardial deformation parameters such as GLS are powerful prognostic markers that correlate with the risk of cardiovascular events and overall patient survival. As stated in the European Society of Cardiology (ESC) 2022 guidelines, the use of STE to evaluate myocardial function is becoming a standard in cardiology because of its high sensitivity and specificity [6].The need for 2D STE also stems from its ability to estimate various myocardial deformation parameters, including global longitudinal strain (GLS), radial strain and circular strain. GLS is one of the most studied and widely used parameters, as its reduction is often associated with worse prognosis in patients with cardiovascular diseases. Studies show that a 1% decrease in GLS is associated with a 5% increase in the risk of cardiovascular events [7].Coronary heart disease and type 2 diabetes lead to significant changes in left ventricular (LV) structure and function. LV remodeling is an adaptive process that can lead to changes in geometry and deterioration of the functional state of the heart. The importance of timely diagnostics and monitoring of these changes cannot be overestimated, as LV remodeling is associated with a high risk of heart failure and other cardiovascular complications.Percutaneous coronary intervention (PCI) is an efficient treatment for CHD that can restore blood flow in the coronary arteries and improve myocardial function. Changes in 2D STE indices before and after PCI may provide important information about LV function recovery and myocardial remodeling. Prior to PCI, patients with CHD and T2D often have worsened global longitudinal strain (GLS) scores, which indicates a decline in myocardial function. These changes are due to myocardial ischemia and the presence of damage caused by chronic hyperglycemia characteristic of T2D. Decreased GLS is an important prognostic marker indicating a high risk of cardiovascular events.One day after PCI, there are often initial signs of improvement in myocardial blood flow and function, which may be manifested by an increase in GLS scores. However, significant changes in LV remodeling and functional status may require more time. Studies show that there are more pronounced improvements in GLS scores1 month after PCI, indicating positive remodeling and recovery of myocardial function. One day after PCI, patients may demonstrate initial improvements in GLS scores. A study published in the journal “Circulation: Cardiovascular Interventions” in 2020 showed that patients who underwent PCI had a significant improvement in GLS 24 hours after the procedure. These changes are associated with immediate restoration of blood flow and reduced myocardial ischemia [8].More significant changes in GLS scores were observed 1 month after PCI. A study from the European Society of Cardiology (ESC) showed that 1 month after PCI, GLS scores improved significantly from initial values. It is associated with the processes of myocardial remodeling, improvement of its structural and functional characteristics. These data indicate long-term efficiency of PCI in restoring LV function and improving prognosis of patients with CHD and T2D [9].Taking into account the growing importance of CHD and T2D as global health problems, our research work focuses on detecting changes in left ventricular contractility and evaluating changes in two-dimensional speckle-tracking echocardiography (2D STE) parameters in patients with CHD and T2D before and after percutaneous coronary intervention.The aim of this study was to evaluate changes in left ventricular contractility and speckle-tracking echocardiography in patients with coronary heart disease and type 2 diabetes before and after percutaneous coronary intervention.
2. Material and Methods
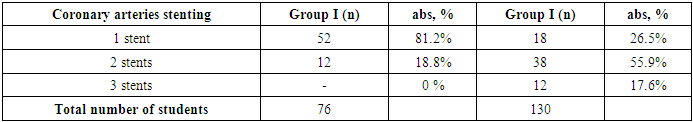
- Clinical trials aimed at analyzing the changes occurring in the myocardium in patients undergoing PCI were conducted at the “NeoMedCardio” private clinic from 2023 to 2024. We selected 132 patients with CHD undergoing inpatient treatment for the study. The age of patients ranged from 35 to 68 years, the mean age was 54.8±15.5 years. All patients were divided into 2 groups: Group I – patients with coronary heart disease without type 2 diabetes (n=64); Group II (n=68) – patients with coronary heart disease against the background of type 2 diabetes.Inclusion criteria were: age from 35 to 68 years, hospitalization, presence of CHD on the background of T2D. Exclusion criteria were as follows: acute myocardial infarction, acute cerebral circulatory failure, heart defects, severe diabetes, acute infectious diseases, hemostasis disorders, severe comorbidities (e.g., cancer or chronic liver/kidney disease), severe allergic reactions to drugs, pregnancy and lactation, severe left ventricular dysfunction (EF below 50%).The research methods included the following components: - Laboratory data: lipid profile, coagulogram study; - Echocardiography: including standard modes (B-mode, M-mode, Doppler echocardiography) was used to evaluate structural and functional changes of the heart. The parameters of LV and other heart chambers were estimated, including size, wall thickness, ejection fraction (EF) and heart valve function; - Two-dimensional speckle-tracking echocardiography (2D STE) was used for more accurate evaluation of left ventricular contractility. Such parameters as global and segmental myocardial strain and its change before and after PCI were measured (Figure 1).
 | Figure 1. Two-dimensional speckle-tracking echocardiography in three positions |
3. Results
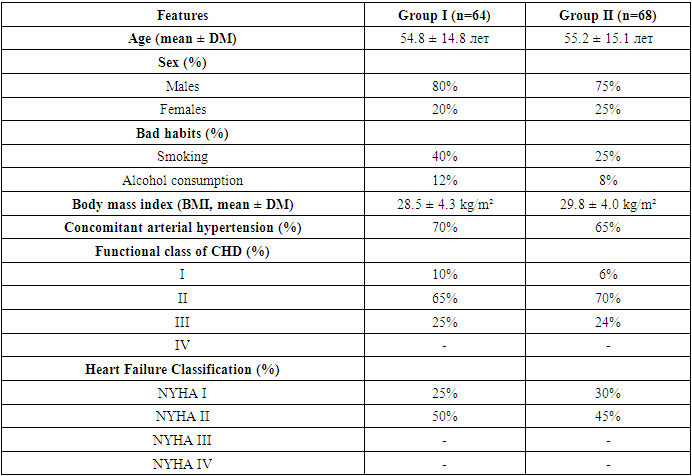
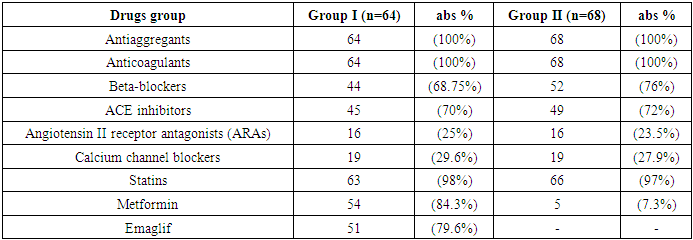
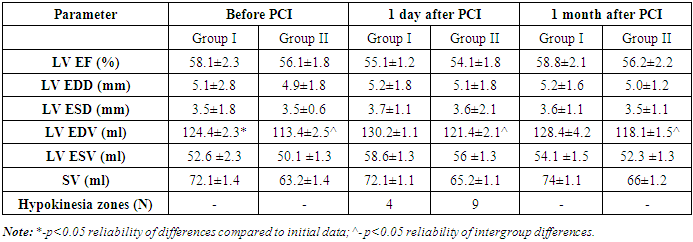
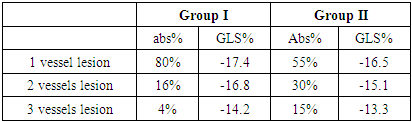
- The groups were randomized according to basic clinical, anamnestic data and therapy received (Table 1).
|
|
 | Figure 2. The blood coagulation indices in both groups |
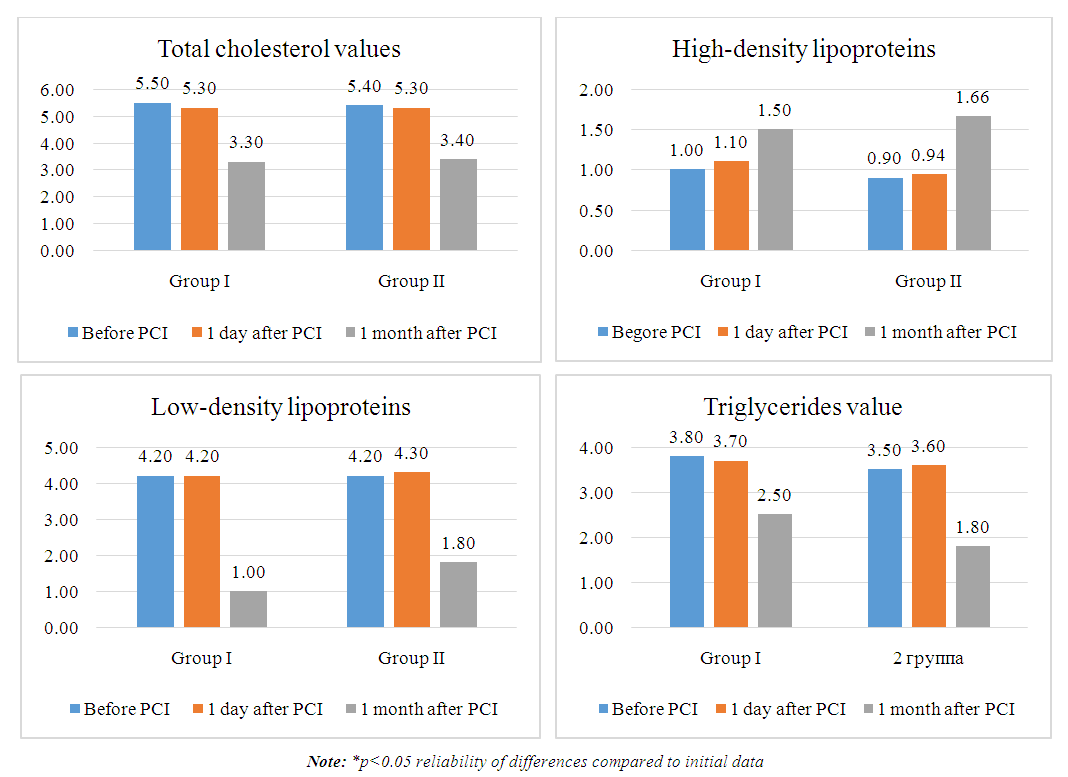 | Figure 3. Lipid spectrum indices |
|
|
|
|
4. Conclusions
- The clinical trial data helped to improve the clinical course of the disease and quality of life, as well as to reduce mortality by implementing methods developed to optimize the treatment of this group of patients; reduce the frequency of hospitalizations, the duration of treatment and improve the quality of life of patients with coronary heart disease. The study of deformation properties in CHD and T2D patients before and after PCI provides an opportunity to evaluate the early efficiency of revascularization, especially in patients with preserved systolic function. A direct negative correlation between GLS and number of affected arteries and a negative correlation between EDV and GLS were found. The use of myocardial deformation properties before and after PCI is a noninvasive predictor of detection both chronic coronary artery disease and efficiency of PCI.
5. Practical Recommendations
- All patients with CHD and type T2D are recommended to undergo routine examinations, including speckle-tracking echocardiography for evaluation of changes in myocardial contractility.Patients who underwent PCI are recommended regular monitoring of coagulogram and lipid spectrum to evaluate the risk of ischemic myocardial remodeling.
Conflict of Interests
- The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
ACKNOWLEDGEMENTS
- The authors express their gratitude to the management of “NeoMedCardio” private clinic for the material provided for our study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML