Gafur-Akhunova Kamola Mirza-Aliyevna1, Polatova Jamila Shagayratovna1, Gafur-Akhunov Mirza-Ali2, Yigitaliev Alisher Bakhodir Ogli3, Tukhtabaeva Mukaddas Tukhtabaevna4, N. I. Tirkasheva4, I. Kh. Tokhtamatov4
1Tashkent State Dental Institute, Tashkent, Uzbekistan
2Center for the Development of Professional Qualifications of Medical Workers, Tashkent, Uzbekistan
3Fergana Medical Institute of Public Health, Fergana, Uzbekistan
4Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology, Tashkent Regional Branch, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The article presents the results of an analysis of the effectiveness of various radiological methods in diagnosing bone metastases in 128 patients with primary-disseminated breast cancer. Among the 128 patients, bone metastases were identified in 28 during the period of neoadjuvant chemotherapy and in 100 (78.1%) before the start of specialized treatment. All patients were treated according to standard protocols with a diagnosis of primary-disseminated breast cancer involving bone metastases (T1-4 N1-2 M1). Following treatment (chemotherapy and hormone therapy), considering the effectiveness of the treatment, palliative surgeries on the primary lesion site were performed in 64 patients (50%). To evaluate the effectiveness of radiological methods in identifying bone metastases, the following were utilized: bone scintigraphy (12 patients), MSCT (65 patients), MRI (100 patients), whole-body imaging (33 patients), and PET/CT (27 patients). The results of the study demonstrated that the diagnostic informativeness of scintigraphy for detecting bone metastases in primary-disseminated breast cancer was high, with a sensitivity of 94.6%, specificity of 90%, and accuracy of 94.9%. MSCT showed sensitivity, specificity, and accuracy of 90.1%, 75%, and 93.8%, respectively. Whole-body MRI yielded sensitivity, specificity, and accuracy of 94.5%, 66.7%, and 88.8%. Whole-body MRI imaging sensitivity was 88.9%, specificity 66.6%, and accuracy 90.9%. The highest diagnostic performance was achieved with PET/CT, showing sensitivity of 96.0%, specificity of 90%, and accuracy of 96.5%. The results of the radiological study indicate that the most effective methods for diagnosing bone metastases in primary-disseminated breast cancer are PET/CT and bone scintigraphy.
Keywords:
Primary-disseminated breast cancer, Bone scintigraphy, MSCT, MRI, Whole-body imaging, PET/CT, Diagnostic informativeness, Sensitivity, Specificity, Accuracy
Cite this paper: Gafur-Akhunova Kamola Mirza-Aliyevna, Polatova Jamila Shagayratovna, Gafur-Akhunov Mirza-Ali, Yigitaliev Alisher Bakhodir Ogli, Tukhtabaeva Mukaddas Tukhtabaevna, N. I. Tirkasheva, I. Kh. Tokhtamatov, The Role of Radiation Methods in the Diagnosis of Bone Metastases in Primary-Disseminated Breast Cancer, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 236-241. doi: 10.5923/j.ajmms.20251501.46.
1. Introduction
Breast cancer is one of the most common pathologies in the structure of oncological diseases. According to "GLOBOCAN" (2022) and Global Oncology Statistics (2012), there is a growing trend in breast cancer incidence [1,2]. In 2022, 2.308 million cases of breast cancer were recorded worldwide, accounting for over 11% of all cancer cases globally. Mortality reached 665,000 cases, ranking fourth among cancer-related deaths after lung, liver, and colorectal cancers [3].In the Russian Federation, 60,717 breast cancer cases were registered in 2013, increasing to 82,499 cases in 2023. The incidence is 57 per 100,000 women, with 24 per 100,000 among women under 40 years old [4].In Uzbekistan, over the last 20 years, breast cancer has occupied the leading position in the structure of oncological diseases, accounting for 11.9% of all cancer cases. Mortality is 11% of all deaths caused by malignant tumors [5,6]. In 2009, stage IV breast cancer was diagnosed in 9% of patients in Uzbekistan; by 2018, this figure had increased to 11% [6].According to Hernandez R.K. et al. (2018), 70% of patients with metastatic prostate and breast cancers have bone metastases [7]. Bone metastases are the most frequent and early localization in breast cancer. One-third of patients with advanced breast cancer present with metastases not only in bones but also in other organs. In 25% of cases, the discovery of metastases is incidental, while in others, it results from targeted diagnostic efforts prompted by clinical manifestations. The average life expectancy of patients with bone metastases is 2–2.5 years with therapy, while the 5-year survival rate ranges from 20% to 40% [8,9].In diagnosing bone metastases, PET/CT has proven to be the most informative method, demonstrating higher sensitivity and accuracy (98.0% and 93.83%) than bone scanning (95.61% and 81.48%) for detecting bone diseases [10,11]. PET/CT has shown the highest sensitivity and accuracy for most skeletal segments, surpassed only by bone scanning in skull lesions. Specificity was 99.09% for both methods [12].The advantage of bone scintigraphy lies in its ability to examine the entire body in a short time, with low radiation exposure and high sensitivity to osteoblastic activity [13,14]. However, its main disadvantages are a lack of specificity and low sensitivity in detecting bone lesions with predominantly osteolytic characteristics. Despite advances in PET/CT and MRI, biopsy remains essential in oncology, particularly for examining patients with metastatic breast cancer, as recommended by the European Society for Medical Oncology (ESMO) in 2021 [15].Purpose of the studyThe aim of this study is to analyze and compare the effectiveness of various radiological methods for diagnosing bone metastases in patients with primary-disseminated breast cancer. The study evaluates the informativeness of scintigraphy, MSCT, MRI, Whole-body MRI, and PET/CT in terms of sensitivity, specificity, and accuracy. Additionally, it aims to identify the most effective method for the early detection and assessment of the extent of bone metastases.
2. Materials and Methods
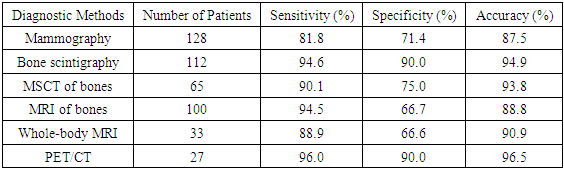
The study observed 128 patients with primary-disseminated breast cancer (PDBC) and skeletal metastases from 2010 to 2023 at the Tashkent City and Regional branches of the Republican Specialized Scientific-Practical Medical Center of Oncology and Radiology of the Ministry of Health of the Republic of Uzbekistan.The patients' ages ranged from 21 to 76 years. The majority were in the age groups of 41–50 years (37 patients, 28.9%) and 51–60 years (41 patients, 32.0%), with fewer cases in the under-30 age group (3 patients, 2.3%) and the over-70 age group (9 patients, 7.0%) (Figure 1).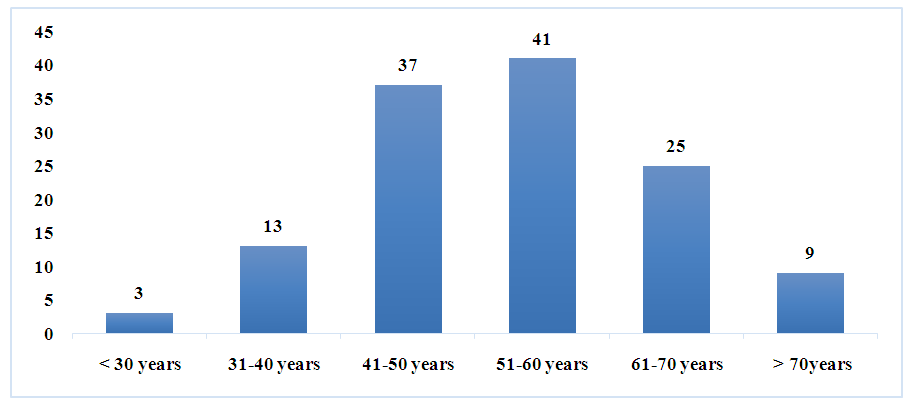 | Figure 1. Distribution of patients by age group |
The duration of the medical history from the first signs of the disease to the doctor's appointment ranged from 1 month to 5 years. Of the 128 patients, 46 (35.9%) sought medical attention for up to 6 months, 29 (22.6%) for 6 to 12 months, and 53 (41.4%) for 5 years. Of the 128 patients examined, 26 (20.3%) had a history of hereditary impairment.Of the 128 patients admitted to the clinic, 14 (10.9%) had breast cancer, 1 (0.7%) had breast cancer, 9 (7.0%) had breast cancer and pain, 7 (5.4%) had breast cancer, increased limbs, decreased appetite, and general weakness, 74 (57.8%) had breast cancer and pain in the bones of the skeleton, 2 (1.5%) had breast cancer and headache, 10 (7.8%) had breast cancer, cough, and pain in the bones of the skeleton. 11 (8.5%) patients had no complaints upon admission.Of the 128 patients, 59 (46%) had the tumor localized in the right breast, 63 (49.2%) in the left breast, and 6 (4.6%) in both breasts.In 56 (43.7%) cases, the upper-external quadrant was affected, in 29 (22.6%) - the upper-inner quadrant of the breast, in 4 (3.1%) - the lower-inner quadrant, in 12 (9.3) - the lower-external quadrant, in 22 (17.1%) - the central section and in 5 (3.9%) - all quadrants of the breast.During visual examination of the mammary glands in the affected area, 14 (10.9%) patients exhibited hyperemia, 25 (19.5%) - infiltration in the affected area, 3 (2.3%) - edema, 5 (3.9%) - skin ulceration, 15 (11.7%) - lemon peel symptom, 1 (0.7%) - area symptom, 18 (14.0%) - nipple syndrome, 11 (8.5%) - tumor decay, 19 (1.5%) - infiltration and ulceration of the mammary gland, and 15 (11.6%) - changes in the mammary glands.Clinically, nodular form was found in 22 (17.1%), rosette-like form in 2 (1.5%), edematous-infiltrative form in 77 (60.1%), pancreatic form in 1 (0.7%), diffuse form in 13 (10.1%), and Pejet cancer in 2 (1.5%).The prevalence of the primary tumor in the breast was assessed as T1 in 5 (3.9%), T2 in 35 (27.3%), T3 in 11 (8.5%), and T4 in 77 (60.1%). Metastatic lesions of regional lymph nodes were assessed as N1 in 79 (61.7%), N2 in 16 (12.5%), and N3 in 17 (13.2%) patients. No regional lymph node involvement was observed in the remaining patients.Gistological examination revealed in situ cancer in 16 (12.5%), infiltrative cancer in 89 (69.5%), infiltrative lobular cancer in 13 (10.1%), tubular cancer in 4 (3.1%), papillary cancer in 4 (3.1%), adenokistotic cancer in 1 (0.7%), and Pejet cancer in 1 (0.7%).The extent of tumor spread according to the TNM system showed a high frequency of primary-disseminated breast cancer in the presence of T3 - T4 and N1-3 among the patients we examined. Of the 128 patients, 12 (9.3%) had T1N1M1 with metastatic bone lesions, 2 (1.5%) had T2N1M1, 6 (4.6%) had T3N1M1, 2 had T3N2M1, 3 (2.3%) had T13N3M1, 50 (39.0%) had T4N1M1, 12 (9.3%) had T4N3M1, and 10 (7.8%) had T4N2M1.As can be seen from the presented data, the extent of tumor spread increased after damage to regional lymph nodes, indicating that the "natural development" of breast cancer gradually increases from local tumor spread to tumor spread (98.5% of patients).The diagnosis of breast cancer was confirmed in 125 (97.7%) patients during cytological examination by breast tumor puncture biopsy, and in all 128 patients during histological examination (trepan biopsy, open biopsy).
3. Results
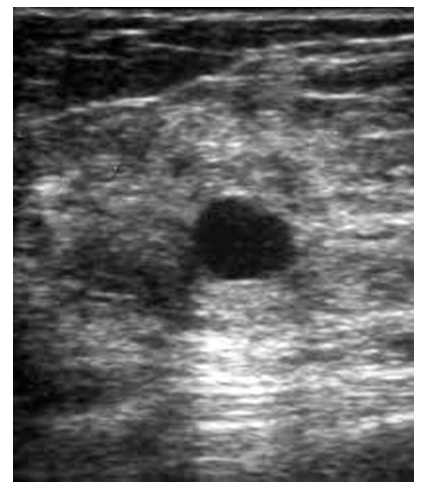
The use of radiation diagnostics in primary-disseminated breast cancer was carried out using ultrasound, radiological, MSCT, MRT, MRT WHOLE BODY, radioisotopic studies and PET/CT of both primary tumor and metastatic lesions. Ultrasound examination was performed in 125 (97.5%) patients to determine the primary focus of the lesion, metastases in the internal organs of the abdominal cavity and regional lymph nodes. Ultrasound examination revealed a nodular formation in 11 (8.6%), a breast tumor in 36 (28.1%), a focial formation in 30 (23.5%), and a breast cancer in 51 (39.8%) (Fig. 2).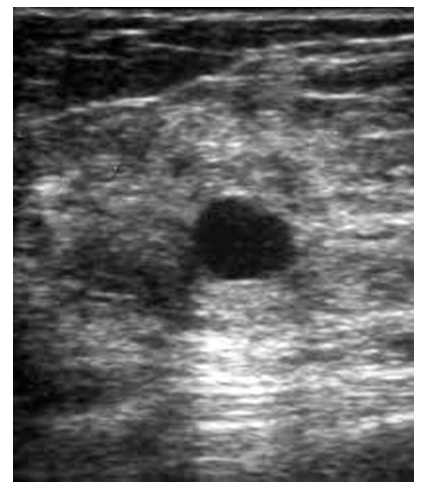 | Figure 2. Ultrasound Imaging of the Right Breast: Nodular Form of Breast Cancer |
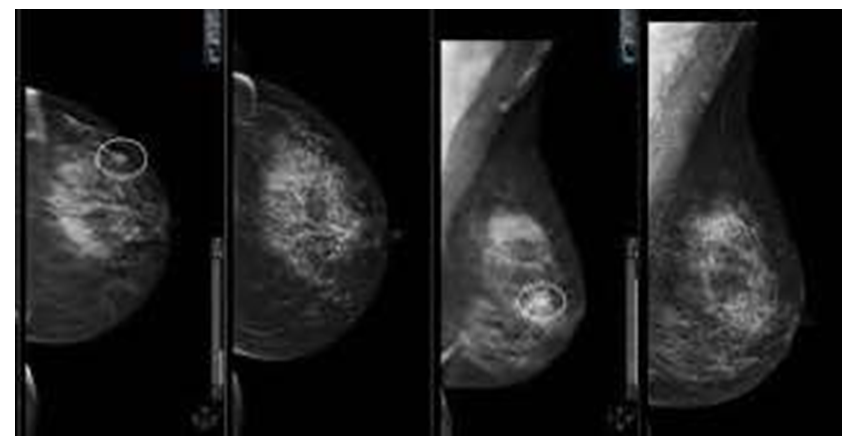
Mammographic examination of the mammary glands was performed on all 128 patients with primary-disseminated breast cancer.Mammographic examination of 128 patients revealed that 1 (0.7%) had Birads 0, 15 (11.7%) had Birads 3, 40 (31.25%) had Birads 4 and 72 (56.25%) had Birads 5 (Fig. 3).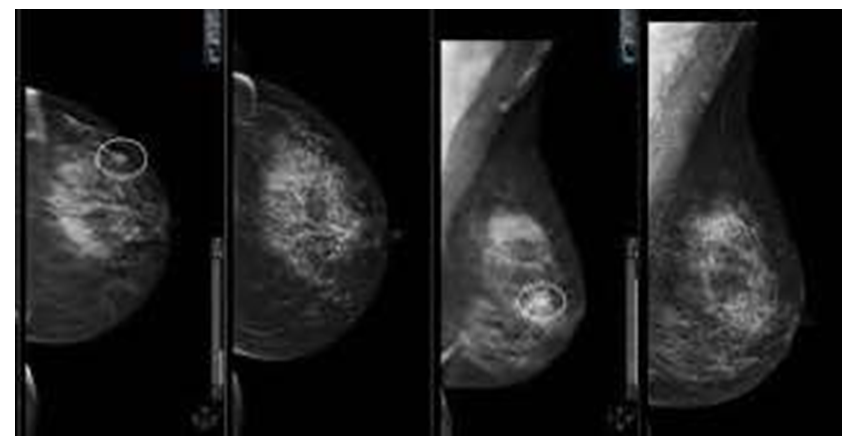 | Figure 3. Mammographic picture of breast cancer (Birads 4 с, Birads 5) |
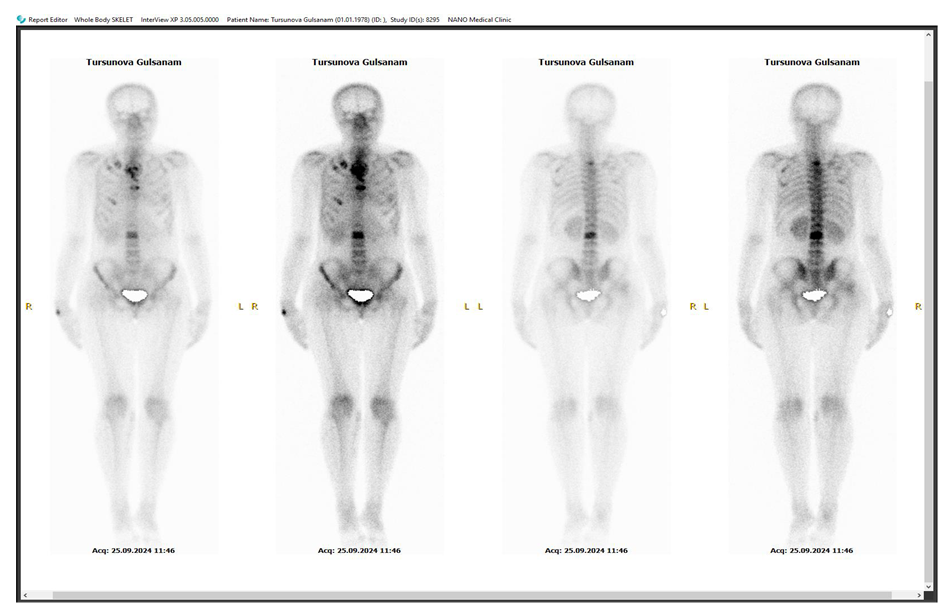
However, despite the conclusion of the mammographic study, the histological conclusion confirmed the presence of breast cancer. After the diagnosis of primary disseminated breast cancer with bone metastases and morphological confirmation of the diagnosis at the primary lesion site, immunohistochemical studies were conducted in 75 (58.5%) of 128 patients. According to the results of the study, the luminal A subtype was identified in 25 (19.5%), the luminal B subtype in 43 (33.5%), and the triple-negative subtype in 7 (5.4%) patients. Among patients with the luminal B subtype, the HER2/neu-negative variant of the tumor was found in 46 (35.9%), and the HER2/neu-positive variant in 29 (22.6%).An analysis of treatment methods showed that chemotherapy was administered to 60 (46.8%) of the 128 patients, chemotherapy and radiation therapy to 3 (2.3%), combined treatment to 26 (20.3%), comprehensive treatment to 31 (22.6%), and symptomatic treatment to 8 (6.2%).In the group of patients receiving combined and comprehensive treatment, surgical treatment of the primary lesion was performed in 47 (36.6%) patients as palliative radical mastectomy according to Madden, in 3 (2.3%) as radical mastectomy according to Patey, and in 9 (7.0%) as palliative mastectomy. Radical resection according to Blokhin was performed in 3 (2.3%) patients, and Veronesi procedures in 2 (1.5%) patients. Radiological examination of the skeleton bones to detect metastatic lesions was performed in 106 patients. Metastases in the skeleton bones were suspected in all 106 patients. To confirm bone metastases, the following radiological diagnostic methods were additionally used: radionuclide bone scans were conducted in 112 (87.5%) patients, magnetic resonance imaging (MRI) in 100 (78.1%), multislice computed tomography (MSCT) in 65 (50.9%), whole-body MRI in 33 (25.8%), and PET/CT in 27 (21.1%). A comprehensive assessment of the results of various radiological methods provided full information about the presence of skeletal metastases and allowed monitoring of the effectiveness of treatment for primary disseminated breast cancer, not only in the primary lesion but also in metastatic bone lesions. Among 128 patients, skeletal metastases were solitary in 11 (8.6%), single in 36 (28.1%), and multiple in 81 (63.3%) patients (Fig. 4).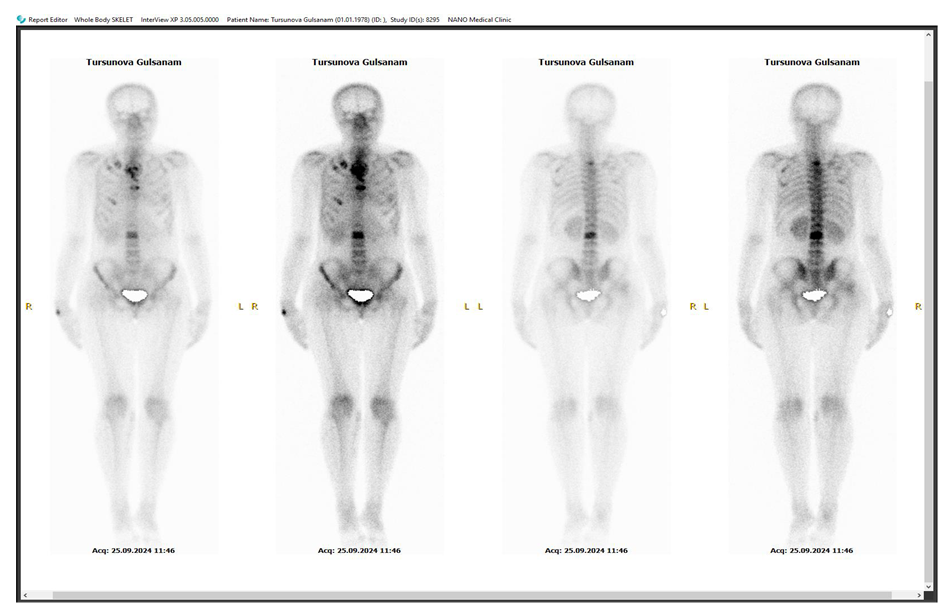 | Figure 4. Bone scan showing multiple metastatic lesions in the skeleton |
Bone metastases in the skeleton were localized as follows: in the vertebral column in 31 patients (24.2%), in the skull bones in 3 (2.3%), in the humerus in 1 (0.7%), in the tibia in 4 (3.1%), in the fibula in 1 (0.7%), in the sternum in 1 (0.7%), in the pelvic bones in 6 (4.7%), and multiple lesions throughout the skeleton in 81 (63.2%) patients. Among the 128 patients with primary disseminated breast cancer, bone metastases appeared during chemotherapy and hormone therapy in 34 (26.6%) patients. After the onset of clinical symptoms of metastatic bone lesions, radionuclide bone scanning was performed, and based on the findings from diagnostic methods (MRI, MSCT, whole-body MRI, and PET/CT), the diagnosis of breast cancer was revised, and the extent of tumor spread was assessed as M1 (Fig. 5). | Figure 5. MSCT of the spine showing metastases and a pathological fracture of the Th12 vertebra |
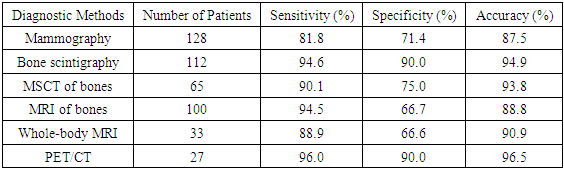
Out of 128 patients with primary disseminated breast cancer and skeletal metastases, radionuclide bone scans (scintigraphy) were performed on 112 patients (87.5%). Among these, 8 patients (7.8%) underwent bone scintigraphy alone, while 105 (93.8%) underwent scintigraphy in combination with MRI and MSCT. An evaluation of the informativeness of each radiological method was conducted. Analysis of radionuclide studies for detecting skeletal metastases revealed a sensitivity of 94.6%, a specificity of 90%, and an accuracy of 94.9%. The high informativeness of the method was especially noted in cases of multiple skeletal metastases, particularly involving the spine and pelvic bones.Table 1. Informativeness of radiological diagnostic methods in primary disseminated breast cancer with skeletal bone involvement
 |
| |
|
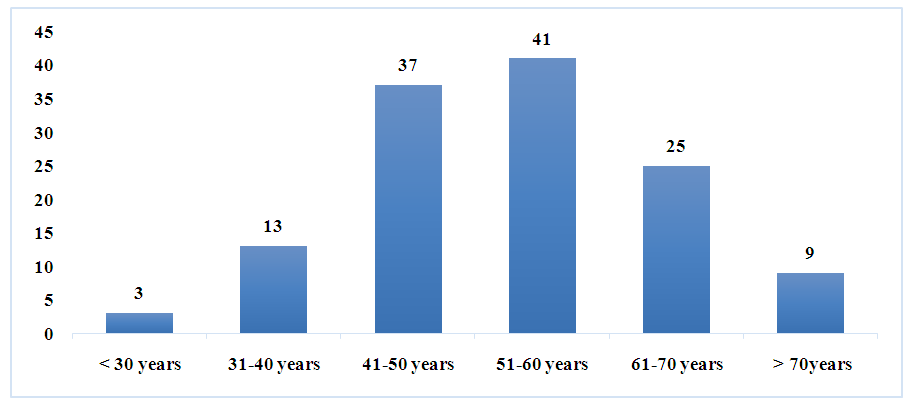
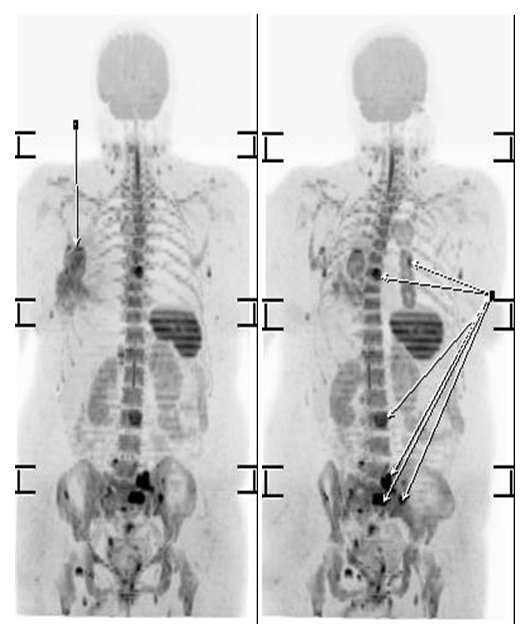
As shown in the table, the informativeness of various radiological diagnostic methods for detecting skeletal metastases in patients with primary disseminated breast cancer varied significantly.Overall, bone scintigraphy and PET/CT demonstrated the highest sensitivity, specificity, and accuracy compared to other methods. At the same time, methods such as MRI and whole-body scanning showed lower specificity and accuracy (Fig. 6).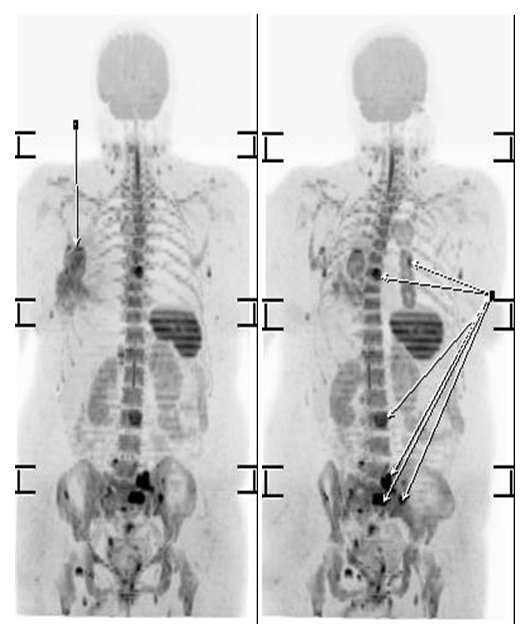 | Figure 6. Whole-body imaging showing skeletal bone involvement |
For mammography, the sensitivity was 81.8%, specificity was 71.4%, and accuracy was 87.5%, while the results of bone scintigraphy were significantly higher. The sensitivity for scintigraphy was 94.6%, specificity 90.0%, and accuracy 94.9%.Analyzing the informativeness of MSCT for detecting skeletal metastases showed that, among the 65 patients examined, the sensitivity of the method was 90.1%, specificity 75%, and accuracy 93.8%. The highest informativeness of MSCT was observed when detecting metastases in long bones, pelvic bones, and the spine.Magnetic resonance imaging (MRI) of the skeletal bones was performed in 100 patients. The analysis revealed that the sensitivity of the method was 94.5%, specificity was 66.7%, and accuracy was 88.8%. High informativeness in detecting skeletal metastases was achieved when metastases were located in various parts of the spine and pelvic bones.Whole-body imaging was conducted in 33 patients to detect metastases in the skeleton and other organs. The informativeness of this method was relatively low compared to other radiological methods for identifying skeletal metastases. The sensitivity was 88.9%, specificity was 66.6%, and accuracy was 90.9%.Positron emission tomography/computed tomography (PET/CT) was performed in 27 patients. The informativeness of this method was relatively high, with sensitivity reaching 96%, specificity 90%, and accuracy 96.5%. The metabolic activity values in skeletal bones ranged from SUV MAX = 3.25 to 13.56.The highest informativeness was observed when metastases were localized in the spine and pelvic bones, particularly in cases of multiple lesions.
4. Conclusions
Thus, the results of the study demonstrated that radiological methods, when used in combination, complemented each other in detecting skeletal metastases, and metastatic bone involvement was identified in all cases. Among the methods, bone scintigraphy and PET/CT using F18-deoxyglucose proved to be the most informative compared to other techniques.
References
| [1] | Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024 May- Jun; 74(3): 229-263, p. doi: 10.3322/caac.21834. Epub 2024 Apr 4. PMID: 38572751. |
| [2] | Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Ticulent J. Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015 Mar; 65(2): 87-108. doi: 10.3322/caac.21262. Epub 2015 Feb 4. PMID: 25651787. |
| [3] | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018 Jan; 68(1): 7-30. doi: 10.3322/caac.21442. Epub 2018 Jan 4. PMID: 29313949. |
| [4] | Malignant neoplasms in Russia in 2023 (incidence and mortality). Edited by Kaprin AD, Starinsky VV, Shakhzadova AO. Moscow, 2024. |
| [5] | Rim CH, Lee WJ, Musaev B, Volichevich TY, Pazlitdinovich ZY, Lee HY, Nigmatovich TM, Rim JS, «Consortium of Republican Specialized Scientific Practical-Medical Center of Oncology and Radiology and South Korean Oncology Advisory Group. Comparison of Breast Cancer and Cervical Cancer in Uzbekistan and Korea: The First Report of The Uzbekistan-Korea,» Medicina (Kaunas), p. 2022 Oct 10; 58(10): 1428. doi: 10.3390/medicina58101428. PMID: 36295588; PMCID: PMC9610191. |
| [6] | Cardoso F, Paluch-Shimon S, Senkus E, et al.. 5th ESO-ESMO International Consensus Guidelines for Advanced Breast Cancer (ABC 5). Ann Oncol. 2020; 31(12): 1623-1649. https://doi.org/10.1016/j.annonc.2020.09.010. |
| [7] | Hernandez RK, Wade SW, Reich A, Pirolli M, Liede A, Lyman GH. Incidence of bone metastases in patients with solid tumors: analysis of oncology electronic medical records in the United States. BMC Cancer. 2018 Jan 6; 18(1): 44. doi: 10.1186/s12885-017-3922-0. |
| [8] | Kim HG, Kim JH, Kim KH, Yoo BC, Kang SU, Kim YB, Kim S, Paik HJ, Lee JE, Nam SJ, Parameswaran N, Han JW, Manavalan B, Cho JY. METTL18 functions as a Phenotypic Regulator in Sre-Dependent Oncogenic Responses of HER2-Negative Breast Cancer. Int J Biol Sci, pp. 2024 Sep 3: 20(12): 4731-4749. doi: 10.7150/ijbs.96487. PMID: 39309445; PMCID: PMC11414398. |
| [9] | Scuiba DM, Gokaslan ZL, Suk I et al. Positive and negative prognostic variables for pts undergoing spine surgery for metastatic breast disease. Eur Spine J 2007, 16(10): 1659-67. |
| [10] | Joana Cristo Santos, Miguel Henriques Abreu, Miriam Seoane Santos, Hugo Duarte, Tiago Alpoim, Inês Próspero, Susana Sousa, Pedro Henriques Abreu, «Bone Metastases Detection in Patients with Breast Cancer: Does Bone Scintigraphy Add Information to PET/CT?,» The Oncologist, Т. %1 из %2Volume 28, Issue 8, p. e600–e605. https://doi.org/10.1093/oncolo/oyad087, August 2023. |
| [11] | Sohaib SA, Cook G, Allen SD, Hughes M, Eisen T, Gore M. Comparison of whole-body MRI and bone scintigraphy in the detection of bone metastases in renal cancer. Br J Radiol. (2009) 82:632–9. doi: 10.1259/bjr/52773262. |
| [12] | Shie P, Cardarelli R, Brandon D, Erdman W, Abdulrahim N, «Meta-analysis: comparison of F-18 fluorodeoxyglucose-positron emission tomography and bone scintigraphy in the detection of bone metastases in patients with breast cancer,» Clin Nucl Med, т. 33, p. 97–101, 2008. |
| [13] | Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ. Radionuclide bone imaging: an illustrative review. Radiogr Rev Publ Radiol Soc N Am Inc. (2003) 23: 341–58. doi: 10.1148/rg.232025103. |
| [14] | Shie P, Cardarelli R, Brandon D, Erdman W, Abdulrahim N. Meta-analysis: comparison of F-18 fluorodeoxyglucose-positron emission tomography and bone scintigraphy in the detection of bone metastases in patients with breast cancer. Clin Nucl Med, p. (2008) 33: 97–101. doi: 10.1097/RLU.0b013e31815f23b7. |
| [15] | Gennari A, André F, Barrios CH, Cortés J, de Azambuja E, DeMichele A. ESMO clinical practice guideline for the diagnosis, staging and treatment of patients with metastatic breast cancer. Ann Oncol Off J Eur Soc Med Oncol. (2021) 32: 1475–95, p. doi: 10.1016/j.annonc.2021.09.019. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML