-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 207-210
doi:10.5923/j.ajmms.20251501.40
Received: Dec. 28, 2024; Accepted: Jan. 22, 2025; Published: Jan. 27, 2025

The Significance of Procalcitonin Determination in the Prognosis and Early Diagnosis of Obstetric Sepsis
Negmatullayeva M. N., Kenjaeva Z. O., Tuksanova D. I.
Bukhara State Medical Institute, Bukhara, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study was to optimize the diagnosis and treatment of sepsis based on the study of the parameters for determining PCT. Materials and research methods. In-depth studies were conducted on a contingent of 96 women, including 30 patients with a physiological course of pregnancy and childbirth (1-st control group). The main prospective group consisted of 66 patients, 31 of whom will undergo a comprehensive study with presepsin biomarker and receive appropriate complex therapy (2-nd group) and 3-rd group they will be 35-patients who were not predicted to develop sepsis by studying biomarkers and, accordingly, did not receive timely therapy aimed at preventing sepsis complications. The results of the study. The comparative indicators of PCT and PSP obtained in this study in different groups showed that they were statistically significantly lower in the control group than in patients with PE and sepsis (p<0.05, respectively). The PCT concentration at admission in the control group of patients was in the range of 0.05-0.50 ng/ml, in group 2 women who were diagnosed with the initial stages of the infectious process 0.50-2.00 ng/ml, in 25 patients (83.3%), and in 5 women (16.7%) 2.00-7 ng/ml. In 23 (76.6%) patients belonging to group 3, this indicator reached 2.00-8.00 ng/ml, in 7 (13.4%) patients with septic shock, the marker levels exceeded 10.00 ng/ml. it was statistically significantly higher than in the second group (p<0.05). The concentration of PSP at the admission of maternity hospitals Postpartum infection with clinical symptoms was increased in 25 (41.6%) women in labor and was on average 4 times higher than the reference values (1120.54±183.63 pg/ml, with a norm of up to 320 pg/ml). In 10 (16.6%) patients, the values were in the range of 300-500 pg/ml, in (43.7%) in the range of 500-1000 pg/ml, in 5 (8.3%) of the most severe patients, the marker levels exceeded 1000 pg/ml. In group 3 patients, the level of the marker was 1.5 times higher than the average in group 2 maternity patients (1382.21±317.04 and 817.00±132.94 pg/ml, respectively). PSP levels were associated with the severity of the clinical course of sepsis and the activity of toxic and infectious manifestations (fever, etc.). The maximum levels of PSP were noted in mixed infection, and the levels of PCT and PSP were statistically significantly higher in patients with severe obstetric sepsis (p<0.05). After 2 weeks. There is a tendency to decrease both indicators in patients with sepsis after antibiotic therapy. The PCT level decreased an average of 8 times in 45 (75%) patients and returned to normal in 15 (25%) patients with an improvement in the clinical condition and disappearance of systemic manifestations of infection. The PSP values remained high in 53 (88.3%) patients, and in (11.7%) cases they tended to increase.
Keywords: Sepsis, Septic shock, Presepsin, Hyperthermia
Cite this paper: Negmatullayeva M. N., Kenjaeva Z. O., Tuksanova D. I., The Significance of Procalcitonin Determination in the Prognosis and Early Diagnosis of Obstetric Sepsis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 207-210. doi: 10.5923/j.ajmms.20251501.40.
Article Outline
1. Introduction
- Sepsis has been a significant medical problem in the global obstetric practice in recent years. Despite the impressive achievements of modern medicine, sepsis and severe infections are still serious problems, and the most threatening thing about this is that with the development of medicine, these problems are only getting worse. Every year, 18-19 million cases of sepsis are registered in the world, and it is very sad that 30% of them end in death [1,4,10].Postpartum purulent-septic disease is one of the urgent problems of modern obstetrics due to its high prevalence and lack of a downward trend. It is known that severe forms of septic complications are one of the main causes of maternal mortality, which is a criterion for timely and qualified care. That is why timely and adequate diagnosis, treatment and prevention of sepsis is one of the top priorities of modern obstetrics [2,3,9].Obstetric sepsis, according to WHO, is the third direct cause of maternal mortality. Successful treatment of sepsis is possible only with simultaneous and effective action on three main links: determining the source of infection, rational antimicrobial therapy, maintaining life in the body and reducing the excessive reaction of the patient's body to infection. It is necessary to pay attention to the fact that when determining the criteria for purulent-septic complications, there are no uniform approaches, and the existing ones are poorly informative. The analysis of the causes of maternal mortality dictates that women's mortality is often observed as a result of irrational management of pregnancy and childbirth, unjustified surgical delivery, late diagnosis of the septic process stage and, accordingly, a delayed solution to the issue of surgical correction-removal of the infection focus [5,6,8]. In this regard, scientists and researchers are interested in finding specific and highly sensitive tests for predicting and early diagnosis of the septic process [7]. Monitoring of plasma procalcitonin may be useful for detecting an invasive or potentially invasive viral infection as an etiological factor of sepsis and assessing its severity, as well as evaluating the effectiveness of antimicrobial therapy and predicting the outcome of the infectious process.The aim of the study was to optimize the diagnosis and treatment of sepsis based on the study of the parameters for determining PCT.
2. Materials and Methods of Research
- 96 women were examined, and the scientific research program was carried out on the basis of the Bukhara Perinatal Center and the maternity complex of the Bukhara region, together with the Department of Obstetrics and Gynecology No. 2 of the Bukhara State Medical Institute. The generally accepted laboratory and instrumental methods of diagnosis and hemocoagulation system, clinical and biochemical and new biomarkers (procalcitonin, presepsin) were carried out. Ultrasound of the uterus was used as a functional diagnostic method. In-depth studies were conducted on a contingent of 96 women, including 30 patients with a physiological course of pregnancy and childbirth (1st control group). The main prospective group consisted of 66 patients, 31 of whom will undergo a comprehensive study with presepsin biomarker and receive appropriate complex therapy (2nd group) and 3-rd group will be 35- Patients who were not predicted to develop sepsis by studying biomarkers and, accordingly, did not receive timely therapy aimed at preventing sepsis complications. Samples of maternal blood serum were used to study the main biochemical, immunological and hemostatic parameters.Statistical processing of the obtained data was carried out with the calculation of the following parameters: arithmetic mean (M), error of the arithmetic mean (t), mean square deviation, confidence interval. The Student's criterion was used to compare the averages and the degree of reliability of the differences between the samples. The differences between the indicators were considered significant if the degree of probability was p<0.05. The principle of evidence-based medicine was used in the organization and conduct of research.
3. The Results of the Study
- The comparative indicators of PCT and PSP obtained in this study in different groups showed that they were statistically significantly lower in the control group than in patients with PE and sepsis (p<0.05, respectively). The PCT concentration at admission in the control group of patients was in the range of 0.05—0.50 ng/ml, in group 2 women who were diagnosed with the initial stages of the infectious process — 0.50—2.0 ng/ml, in 25 patients (83.3%), and in 5 women (16.7%) 2.0-7 ng/ml. In 23 (76.6%) patients belonging to group 3, this indicator reached 2.0—8.0 ng/ml, in 7 (13.4%) patients with septic shock, the marker levels exceeded 10.00 ng/ml. it was statistically significantly higher than in the second group (p<0.05).The concentration of PSP at the admission of women in labor with clinical symptoms of postpartum infection was increased in 25 (41.6%) of women in labor and was on average 4 times higher than the reference values (1120.54±183.63 pg/ml, with a norm of up to 320 pg/ml). In 10 (16.6%) patients, the values were in the range of 300-500 pg/ml, in (43.7%) — in the range of 500-1000 pg/ml, in 5 (8.3%) of the most severe patients, the marker levels exceeded 1000 pg/ml. In group 3 patients, the level of the marker was 1.5 times higher than the average in group 2 maternity patients (1382.21±317.04 and 317.00±132.94 pg/ml, respectively). The levels of PSP were combined with the severity of the clinical course of sepsis and the activity of toxic and infectious manifestations (fever, etc.). The data are shown in Figure 1.
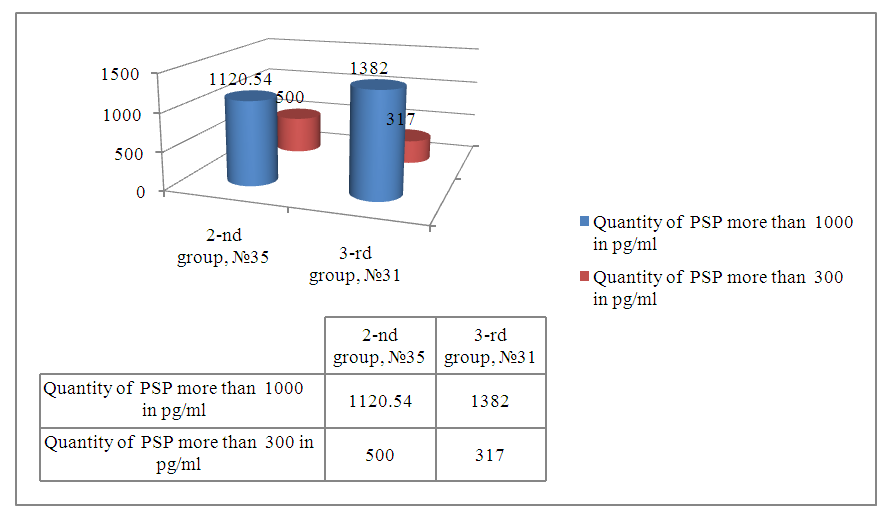 | Figure 1. Comparative data of PSP in two main groups |
4. Conclusions
- Analysis of the diagnostic characteristics of PCT and as a promising biomarker for the early diagnosis of obstetric sepsis, especially in cases of high clinical suspicion and negative results of a hemoculture study. Our results showed that if the PSP values remain high despite normalization of PCT and resolution of clinical symptoms of postpartum infection, the possibility of recurrence of the disease and the need to continue antibacterial therapy with careful monitoring of patients should be considered. Only the combined normalization of PCT and PSP indicates the effectiveness of the treatment and the possibility of its termination and reducing the risk of sepsis progression, its recurrence, and maternal mortality.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML