Dilbar Rasulova
PhD., Associate Professor, Department of Neurology and Medical Psychology, Tashkent Medical Academy, Tashkent, Uzbeksitan
Correspondence to: Dilbar Rasulova, PhD., Associate Professor, Department of Neurology and Medical Psychology, Tashkent Medical Academy, Tashkent, Uzbeksitan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Stroke represents the culmination of comorbid diseases. With age, an accumulation of diseases occurs, some of which reach the stage of decompensation, especially in older people, causing brain catastrophe. In the multidisciplinary clinic of the Tashkent Medical Academy at the Department of Neurology with Medical Psychology, in the Intensive Neurology Department during 2021-24, 214 patients with a diagnosis of Cerebrovascular disease were examined. Acute ischemic cerebrovascular accident in the middle cerebral artery. The distribution of patients by age category revealed a concentration of severe forms of stroke among people aged 60-69 years, which emphasizes the importance of age as a risk factor. Hypertension (Htn), coronary artery disease (CAD) and diabetes mellitus (DM), being key comorbidity factors, increase with age, most pronounced in older age categories. The combination of hypertension + coronary artery disease + diabetes is associated with an increase in the severity of stroke in older age groups. The findings highlight the need for early diagnosis and control of comorbid conditions to prevent the development of severe forms of stroke, especially in middle-aged and older patients.
Keywords:
Stroke, Cerebrovascular disease, Comorbid diseases, Hypertension, Coronary artery disease, Diabetes mellitus
Cite this paper: Dilbar Rasulova, Comorbidity of Cardiovascular Pathology in Ischemic Stroke, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 197-200. doi: 10.5923/j.ajmms.20251501.38.
1. Introduction
The problem of cerebrovascular diseases [4] and stroke [6] has become more and more urgent in recent years. Every year in the world cerebral catastrophe catches up with more than 15 million people [13]. In Russia every year more than 500 thousand cases of acute cerebral circulatory disorders are registered, and in Uzbekistan according to statistical studies lethality from circulatory diseases in 2021 amounted to more than 60% [12]. Stroke has been getting younger in recent years: at least 20% of circulatory disorders occur in patients under 50 years of age [11]. Strokes are the most frequent cause of mortality after myocardial infarctions and malignant neoplasms and are the leading cause of disability among the able-bodied population [1,2].Stroke represents the culmination of comorbid diseases [5]. If we consider comorbidity in terms of age, with age there is an accumulation of diseases, some of which reach the stage of decompensation, especially in older people, in particular, at the age of 60-69 years [3,7].The influence of comorbid pathology on clinical manifestations, diagnosis, prognosis and treatment of many diseases is multifaceted and individual. The interaction of diseases, age and drug therapy significantly changes the clinical picture and course of the underlying disease, the nature and severity of complications, reduces the quality of life of the patient, limits the effectiveness of the therapeutic and diagnostic process [8,9]. Background disease contributes to the emergence or unfavorable course of the underlying disease, increases its severity, contributes to the development of complications. Thus, background disease, as well as the main disease, requires urgent treatment [10]. The aim of the study was to investigate the comorbidity of cardiovascular pathology (hypertension-Htn, coronary artery disease-CAD, diabetes mellitus-DM) in ischemic stroke.
2. Materials and Methods
During 2021-2024 on the basis of the Department of Neurology and Medical Psychology, in the Intensive Neurology Department of the Tashkent Medical Academy. 214 patients with the diagnosis of "Cerebrovascular disease. Acute cerebrovascular circulation disorder of ischemic type in the middle cerebral artery basin". Depending on the degree of motor impairment in stroke in the acute period of stroke, all patients were divided into the following 4 groups: Group 1 - 66 patients with mild degree of stroke. In the neurologic status: muscle strength was 4-5 points; group 2 - 48 patients with a moderate degree of stroke. In the neurologic status, muscle strength amounted to - 3 points; group 3 - 49 patients, with moderately severe degree of stroke. In patients in neurologic status muscle strength was 2-3 points or irregular deep hemiparesis; group 4 - 51 patients with severe stroke degree. In the neurologic status, the patients' muscle strength was 0 points- hemiplegia. All patients underwent clinical and neurological, laboratory studies, ECG, neuroimaging methods (brain CT or MRI), and clinical neuropsychological studies. Statistical analysis of data was performed using STATISTICA 6.0 program on a personal computer.
3. Results and Discussions
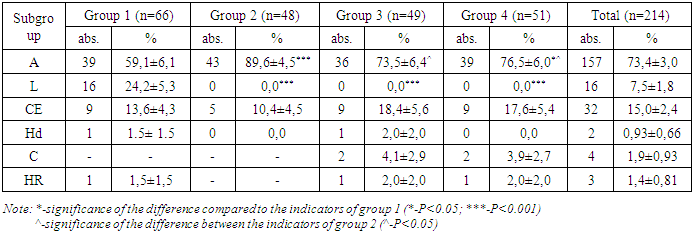
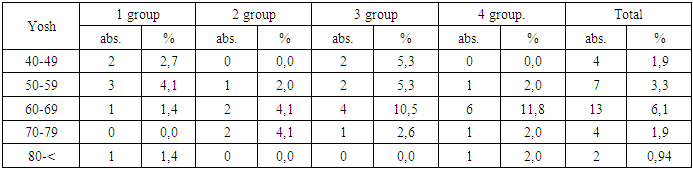
In the conducted study by stroke subtype (Table 1) in the examined patients, the atherothrombotic subtype was found in 157-73.4% of patients, cardioembolic in 32-15.0%, lacunar in 16-7.5%, hemodynamic in 2-0.93%, hemorheologic in 3-1.4%, and cryptogenic stroke in 4-1.9% of patients. Of these, women were 55-25.7% and men were found to be 159-74.3%. Left cerebral hemisphere lesions were in 128-59.8%, and right hemisphere lesions were in 86-40.2% of patients. When stroke patients were divided by age, the most common age range was 60-69 years with a mean age of 64.5 years.Table 1. Distribution of patients in the main group by stroke subtypes
 |
| |
|
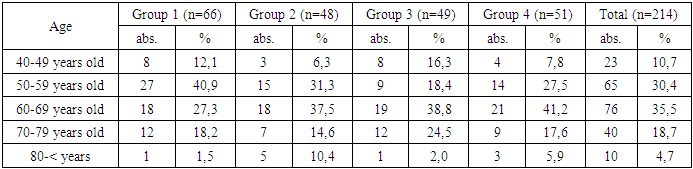
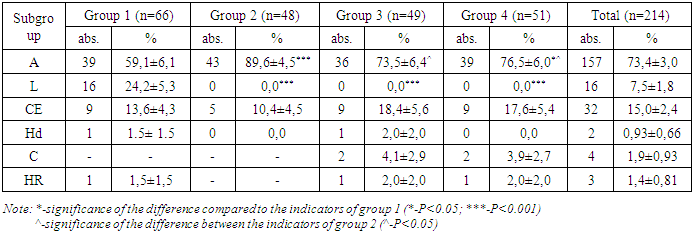
In terms of age, the age categories of patients are presented in five age groups: 40-49, 50-59, 60-69, 70-79 and 80 years and above. (Table 2)Table 2. Patients in the study by age
 |
| |
|
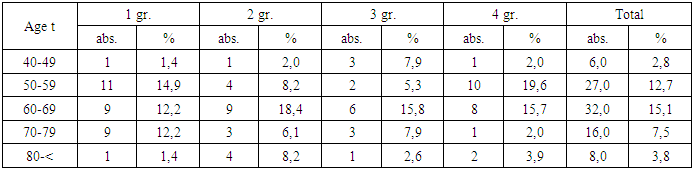
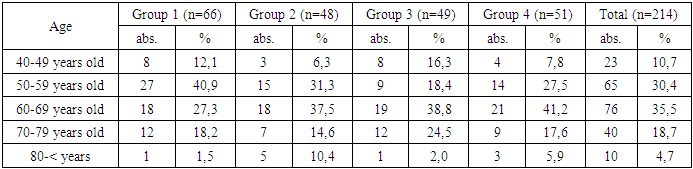
The largest number of patients was in the age groups 60-69 years (35.5%) and 50-59 years (30.4%), emphasizing the significant representation of middle-aged and older individuals in the sample. In terms of stroke severity by age: in the 40-49 age group, patients were distributed predominantly between the first (mild stroke), second (moderate stroke), and third (moderate-severe stroke) groups, confirming the lower severity of stroke at younger ages. In the 50-59 and 60-69 age groups, there was an even distribution of patients between stroke severity groups, with an increasing proportion of severe cases (group 4) at older ages. In the age group 70-79 years and older, patients with severe stroke account for a smaller proportion, but age-related comorbidity increases significantly.Among 201 comorbid conditions in 214 stroke patients, stage III hypertension was the most frequent comorbid condition, which was present in 93.9% of patients. Diabetes mellitus was diagnosed in 53-24.8% of patients, diabetic macro- and microangiopathy in 36-16.8%, and impaired glucose tolerance in 11-5.1%.Analysis and conclusion on the age distribution of comorbidity of hypertension and coronary artery disease in patients with stroke of different severity:The analysis and conclusion on the age distribution of comorbidity of hypertension and coronary artery disease in patients with stroke of different severity (Table 3) revealed the following: patients are represented in five age groups: 40-49, 50-59, 60-69, 70-79, and 80 years and older; the highest number of patients was in the age groups 60-69 years (32%) and 50-59 years (27%), emphasizing the significant representation of middle-aged and older individuals in the sample. Age-specific stroke severity: in the 40-49 age group, patients were distributed predominantly between the first (mild stroke), second (moderate stroke), and third (moderate-severe stroke) groups, confirming the lower severity of stroke at younger ages.Table 3. Rates of hypertension and coronary artery disease (Htn+CAD) in the age aspect in groups
 |
| |
|
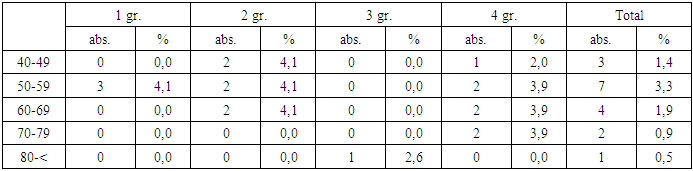
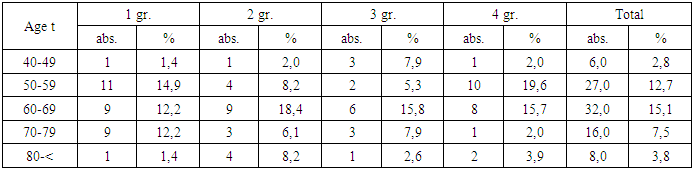
In the age categories 50-59 and 60-69 years, there is an even distribution of patients between stroke severity groups, with an increase in the proportion of severe cases (group 4) at older ages; in the age group 70-79 years and older, patients with severe strokes constitute a smaller proportion, but age-related comorbidity increases significantly. Analysis of the relationship between age and comorbidity revealed: the prevalence of hypertension and coronary artery disease is observed in older age groups (50 years and older), which is consistent with known epidemiologic data, and patients with severe stroke (group 4) more often have a high level of comorbidity in the age group 60-69 years. The next comorbidity under consideration is hypertension (Htn) and diabetes mellitus (DM).Analysis of data on comorbidity of hypertension and diabetes mellitus (Table 4) in the age aspect among patients with stroke revealed the following: the greatest number of patients with a combination of hypertension and diabetes mellitus falls on the age category 50-59 years (7 cases) and 60-69 years (5 cases); in group 1, there are more patients from the category 50-59 years, which is probably associated with earlier diagnosis and control of diseases against the background of mild stroke severity; in group 2, there is an even distribution of cases among the age groups. Thus, the analysis showed that the frequency of comorbidity of hypertension and diabetes mellitus differs depending on age and stroke severity. Patients of age groups 50-59 years and 60-69 years most often have these comorbid conditions, which may be associated with the progressive course of chronic diseases in this age category. On the background of mild stroke, comorbidity is more pronounced, which suggests better detection and treatment of diseases. On the contrary, in severe groups there are fewer cases, which is probably related to the deterioration of the general condition of patients and less effective management of comorbidities. Table 4. Rates of hypertension and diabetes mellitus (Htn+DM) in the age aspect in groups
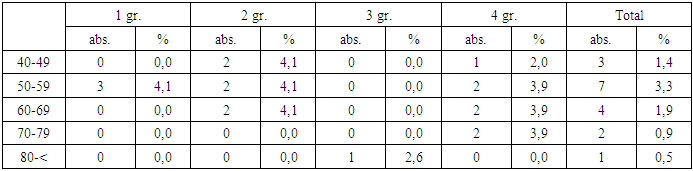 |
| |
|
In the next comorbidity considered, we took the combinations of hypertension (Htn), coronary artery disease (CAD) and diabetes mellitus (DM).Analysis of Table 5 of comorbidity of hypertension (Htn), diabetes mellitus (DM) and coronary artery disease (CAD) among patients divided into groups according to stroke severity revealed certain age and clinical patterns: 1. Younger age group (40-49 years): The proportion of patients with comorbidity in this category was minimal, regardless of stroke severity. This confirms the low prevalence of this combination of diseases among younger patients.2. Group 50-59 years: There was a relatively even distribution of cases between stroke severity groups. However, a decrease in the number of patients with this comorbidity was observed in group 4 (severe stroke), which may be related to the limited number of older patients with severe stroke.3. Group 60-69 years: The highest concentration of patients with Htn+ DM + CAD was recorded in groups with moderate-severe (group 3) and severe stroke (group 4). This may indicate an association of stroke severity with age-related changes and duration of comorbid diseases.4. Patients of older age categories (70 years and older): Comorbid conditions in this category were predominantly noted in stroke severity groups 3 and 4, indicating a significant impact of comorbidity on clinical outcomes and stroke severity in this age group. Table 5. Rates of hypertension, coronary artery disease and diabetes mellitus (Htn+CAD+DM) in age-specific groups
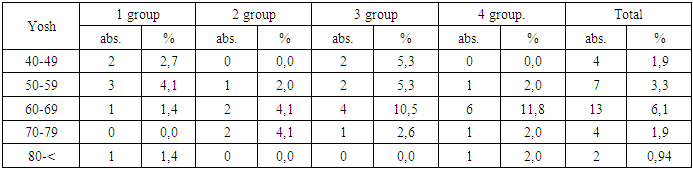 |
| |
|
Thus, significant age and clinical differences were found in the distribution of patients with comorbidity (Htn + DM + CAD). The data emphasize that the combination of these diseases is more associated with increased stroke severity in older age groups. The results suggest the need for increased cardiovascular monitoring in patients with these comorbidities, especially in the age group of 60 years and older.
4. Conclusions
Distribution of patients by age categories revealed a concentration of severe forms of stroke among those aged 60-69 years, which emphasizes the significance of age as a risk factor. Hypertension and coronary artery disease, being key comorbidity factors, increase with age, most pronounced in older age categories. In younger age groups (40-49 years), mild and moderate forms of stroke predominate, whereas in the age group 50-69 years there is a more even distribution of stroke severity. The combination of Htn+CAD+DM is associated with increased stroke severity in older age groups. The findings emphasize the need for early diagnosis and control of comorbid conditions to prevent the development of severe forms of stroke, especially in middle-aged and elderly patients.
References
| [1] | Larkin V.I., Bort A.A., Lisina T.A., Potasheva A.D., Khvostov V.A. Ischemic stroke in patients with comorbid pathology. Journal of Neurology and Psychiatry named after S.S. Korsakov. S.S. Korsakov. Special Issues. 2018; 118(3-2): 15-19. |
| [2] | Ekusheva, E.V. Post-stroke rehabilitation: prognostic criteria of motor function recovery. Educational and methodological manual / E.V. Ekusheva, E.S. Kiparisova. - М., 2017. - 88с. |
| [3] | Epifanov V.A., Epifanov A.V., Glazkova I.I. et al. Medico-social rehabilitation of patients after stroke. Moscow: GEOTAR-Media, 2021. 352 с. DOI: 10.33029/9704-6033-7- 2021-MRI-1-352. |
| [4] | Rasulova, Munisa et al. “LOGOS” in the rehabilitation of post-stroke aphasia Journal of the Neurological Sciences, Volume 429, 119644. |
| [5] | Rasulova D.K. Comorbidity as a predictor of stroke outcome. Journal of neurology and neurosurgery research // (2024) impact factor 5.7. Volume 5 Issue 3. |
| [6] | Rasulova D.K., Rasulova M.B., Kuranbaeva S.R. The Influence of varios factors on the recovery dynamics of post stroke aphasia. // Abstracts Journal of the neurological Sciences // (2019) doi:10.1016/j.jns.2019.10.72. |
| [7] | Stroke. Manual for physicians. Edited by Stakhovskaya L.V., Kotov S.V. Moscow: Medical Information Agency; 2014. |
| [8] | Kadykov A.S., Chernikova L.A., Shakhparonova N.V. Rehabilitation of neurological patients. 4th ed. Moscow: MEDpress-Inform, 2021. 560 с. |
| [9] | Kadykov, A.S. Rehabilitation of neurological patients / A.S. Kadykov, L.A. Chernikova, N.V. Shakhparonova. - Moscow: MEDpress-Inform, 2014. - 560 с. |
| [10] | Kovalchuk, V.V. Rehabilitation of patients after stroke / V.V. Kovalchuk, A.O. Gusev // Journal of Neurology and Psychiatry. Kovalchuk, A.O. Gusev // S.S. Korsakov Journal of Neurology and Psychiatry. - 2016. - Т. 116, № 12-2. - С. 59-64. |
| [11] | Myakotnykh V. S. Stroke in the elderly and senile age: proceedings of the twenty-second international scientific-practical conference "Elderly Patient. Quality of Life" (October 2-3, 2017 / V. S. Myakotnykh // Clinical Gerontology. Quality of life" (October 2-3, 2017) / V. S. Myakotnykh // Clinical Gerontology. - 2017. - Vol. 23, N9-10. - С. |
| [12] | Nazarova Zh. A. Clinical and statistical characteristics of patients with cerebral stroke: scientific edition / J. A. Nazarova, S. N. Rakhmatova, N. A. Hodjaeva // Bulletin of the Tashkent Medical Academy. - 2021. - N 3. - С. 120-123. - Bibliogr: 11 names. |
| [13] | Heart rhythm disturbance in the acute stage of ischemic stroke: scientific edition / A. K. Koyirov [et al] // Proceedings of the V Congress of the Association of Emergency Medicine Doctors of Uzbekistan and the I Congress of the Euro-Asian Community of Emergency Medicine, dedicated to the 20th anniversary of the emergency medical care system of the Republic of Uzbekistan (Tashkent, November 11-12, 2021). - Tashkent, 2021. - С. 231-232. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML