-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 193-196
doi:10.5923/j.ajmms.20251501.37
Received: Dec. 22, 2024; Accepted: Jan. 17, 2025; Published: Jan. 27, 2025

High-Protein Parenteral Nutritional Support in the Postoperative Period of Cervical Cancer
Raximov Nodir Maxammatkulovich, Khudayberdieva Shokhista Amirkul Qizi
Samarkand State Medical University, Samarkand, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The study explores the efficacy of high-protein parenteral nutritional support in the postoperative management of cervical cancer patients. Conducted at the Samarkand branch of the Republican Specialized Scientific-Practical Medical Center Of Oncology And Radiology, the research involved 67 patients divided into control and experimental groups. The results demonstrated that high-protein nutritional intervention, compared to standard nutritional support, significantly improved nutritional parameters, quality of life, and functional recovery of patients post-surgery. Statistically significant improvements in albumin, total protein, hemoglobin levels, and Karnofsky Performance Scale scores were observed in the experimental group. Long-term outcomes, including reduced tumor recurrence rates and enhanced economic efficiency, further underscore the clinical and economic viability of this approach. The findings emphasize the importance of nutritional risk screening and targeted protein-enriched therapy in cervical cancer care, suggesting an optimized postoperative recovery framework.
Keywords: High-protein nutritional support, Cervical cancer, Postoperative care, Nutritional risk screening, Tumor recurrence, Karnofsky Performance Scale, Protein-enriched therapy, Economic efficiency, Gynecologic oncology, Parenteral nutrition
Cite this paper: Raximov Nodir Maxammatkulovich, Khudayberdieva Shokhista Amirkul Qizi, High-Protein Parenteral Nutritional Support in the Postoperative Period of Cervical Cancer, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 193-196. doi: 10.5923/j.ajmms.20251501.37.
1. Introduction
- Cervical cancer remains one of the most prevalent malignancies among women worldwide, ranking as the fourth most common cancer in females. Despite advancements in early detection and treatment, it continues to pose a significant global health burden, particularly in low- and middle-income countries where access to preventive measures, such as HPV vaccination and routine screening, remains limited [3]. The pathogenesis of cervical cancer is multifactorial, with persistent infection by high-risk human papillomavirus (HPV) types being the primary etiological factor. However, other contributing factors such as genetic predisposition, lifestyle behaviors, and socioeconomic disparities play critical roles in its development [2].Epidemiological studies suggest that lifestyle and environmental factors contribute to up to 50–60% of cervical cancer cases, while hereditary factors account for only 10% of the etiology [7]. Among lifestyle factors, early sexual debut, multiple sexual partners, high parity, and poor sexual hygiene have been identified as significant risk factors. Additionally, infections with herpes simplex virus type 2 (HSV-2) and human immunodeficiency virus (HIV) further increase the risk of persistent HPV infection and progression to invasive cancer [5]. Beyond these, dietary habits, excessive caloric intake, and frequent consumption of processed and high-fat foods have emerged as important contributors to the disease. Alcohol and tobacco use exacerbate the risk by inducing chronic inflammation and immunosuppression [8].The role of nutrition in cancer treatment and recovery has gained increasing attention in recent years. Cancer-related malnutrition and cachexia, characterized by significant weight loss, muscle wasting, and impaired immune function, are observed in up to 70% of patients with advanced-stage gynecologic cancers [1]. These conditions not only reduce patients' quality of life but also worsen treatment outcomes by increasing susceptibility to infections, prolonging hospital stays, and delaying recovery. Postoperative nutritional support, particularly in cervical cancer patients, is critical for improving clinical outcomes, reducing complications, and enhancing overall recovery [4].Emerging evidence highlights the importance of individualized nutritional interventions tailored to the unique metabolic demands of cancer patients. High-protein nutritional support, specifically designed to address the elevated protein and energy requirements during the postoperative period, has shown promising results [6]. Protein-enriched diets have been associated with improved wound healing, reduced postoperative infections, and enhanced physical function. Additionally, integrating nutritional risk screening into standard care allows clinicians to identify patients at risk of malnutrition early and provide timely interventions, leading to better recovery and long-term outcomes [9].This study investigates the impact of high-protein parenteral nutritional support on the postoperative nutritional status, functional recovery, and quality of life in cervical cancer patients. The findings aim to establish an evidence-based framework for improving the postoperative management of cervical cancer, optimizing both clinical and economic outcomes in gynecologic oncology care.Purpose of the study: The goal is to study the impact of standard nutritional support based on nutritional risk screening on nutritional conditions and the quality of life of patients with cervical cancer in the postoperative period in a comparative aspect.
2. Materials and Methods
- The clinical data of 67 patients with Cervical cancer who underwent treatment at the Samarkand branch of the Republican Specialized Scientific-Practical Medical Center Of Oncology And Radiology, Samarkand for the period from February 2021 to February 2023 were studied in prospectus and retrospective order. Routine nutritional support (control): Patients were prescribed standard volumes of enteral and parenteral nutritional support - energy requirement of 20 kcal/kg, protein requirement of 1.1 g/kg/day, while the duration of the nutritional intervention did not exceed 5 days. The protein-saturated group (main) Patients were prescribed standard volumes of enteral and parenteral nutritional support - energy requirement of 30 kcal/kg, protein requirement of 1.5-2.0 g/kg/day, and the duration of the nutritional intervention did not exceed 6 days.
3. Results
- 35 (52.2%) patients with cervical cancer who received routine nutritional support after surgery were included in the control group, and the remaining 32 (47.8%) patients who received protein-rich nutritional support after surgery were included in the main group. No significant differences were found between the two groups in terms of age (control group/main group respectively) 39.5±5.2/41.12±3.9 p=0.31, BMI (kg/m2) 20.1±1.19/21.6±1.78, p=0.388, tumor localization p=0.874, tumor diameter p=0.235, differentiation level p=0.513, (all P > 0.05) (see Figure 1).
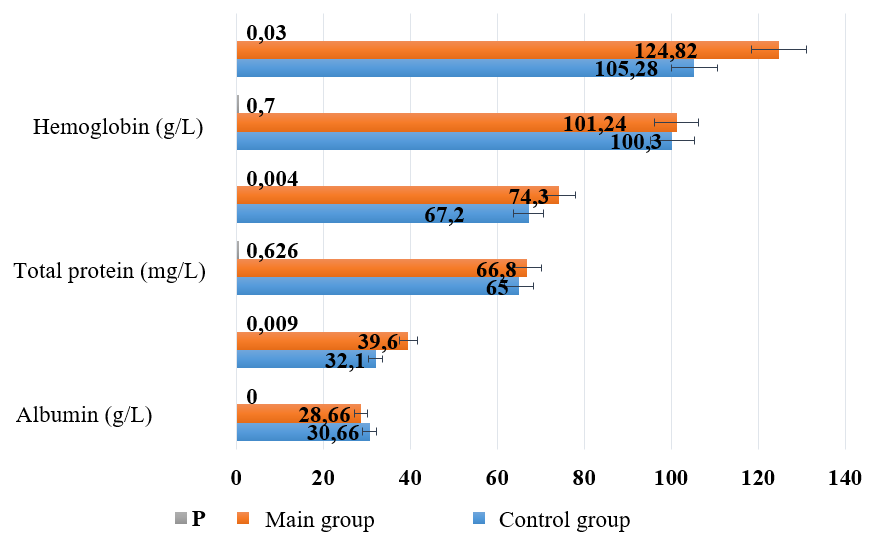 | Figure 1. Comparison of nutritional indicators between the two groups |
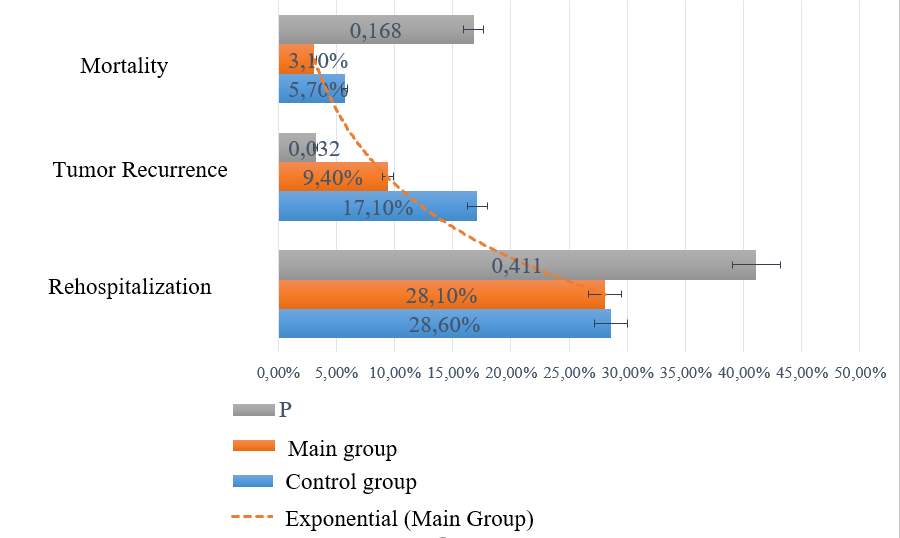 | Figure 2. Comparison of the short-term forecast between two groups |
4. Conclusions
- Summarizing the obtained results, high-protein nutritional intervention, based on nutritional risk screening, can benefit patients with cervical cancer (CC), helping to improve postoperative nutritional status and quality of life while reducing the risk of postoperative tumor recurrence. Nutritional risk screening in patients with cervical cancer and providing appropriate nutritional support holds critical clinical significance.Adding protein-enriched therapy to the standard volume of enteral nutrition, aimed at meeting energy requirements of 30 kcal/kg and protein requirements of 1.5–2.0 g/kg/day, while limiting the duration of nutritional intervention to no more than 6 days, is a more effective and rational approach.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML