Erkin A. Eshbaev1, Aziz A. Zufarov2, Makhzuna Kh. Mukhsinova3
1DSc, Associate Professor, Department of Pathological Anatomy, Tashkent Medical Academy, Tashkent, Uzbekistan
2DMS, Associate Professor, Department of Propaedeutics of Childhood Diseases and Hematology, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
3PhD, Associate Professor, Head of the Department of Therapeutic No.1, Tashkent State Dental Institute, Tashkent, Uzbekistan
Correspondence to: Makhzuna Kh. Mukhsinova, PhD, Associate Professor, Head of the Department of Therapeutic No.1, Tashkent State Dental Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Although the clinical and morphological frequency of atresia, which is the 4th variant of esophageal malformation and continues mainly with esophageal wall stenosis, is relatively low, in most cases patients experience a sudden decrease in quality of life. Morphologically, all anatomical walls of the esophagus of this type contain formed tissue components mainly in those areas that have not undergone stenosis, and in those areas where stenosis is detected, areas that have undergone dysplasia in the esophageal wall are identified. In particular, myodysplasia on the muscular bottoms is characterized by the fact that there are very few alveolar tubular glands on the mucosa and mucous membranes, there are 1-3-layered cuboid and prismatic epithelium on the surface of the mucous membrane, as well as cuboid epithelium cells that undergo metaplasia.
Keywords:
Esophageal atresia, Stenosis, Morphology, Dysplasia, Morphological paralysis
Cite this paper: Erkin A. Eshbaev, Aziz A. Zufarov, Makhzuna Kh. Mukhsinova, Pathomorphological Changes Developing in the Stenosing Variant of Esophageal Atresia in Infants, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 188-192. doi: 10.5923/j.ajmms.20251501.36.
1. Introduction
Anomalies in the development of the esophagus are a process in the embryonic period that continues the development of the esophagus and its structural formations with anatomical and histological changes. Worldwide the development of this pathology corresponds to 40 out of 100,000 infants. The detection of this pathology during early pregnancy screening in the United States and European countries, based on strict guidelines for termination of pregnancy, has an average incidence rate of 4-8 per 100,000 infants [4,6,15,16]. While the incidence of these pathologies in the CIS countries, including the Russian Federation, is 20-25 cases per 100,000, in the Republic of Uzbekistan this figure is 8-10 cases per 1,000 infants, which is manifested by a high mortality rate of an average of 60-78% of cases within a month after the birth of infants [3,5,9,17]. Currently, this issue is a problem for both pediatricians and neonatologists, since, according to foreign literature and anamnestic data, the incidence is 2.5 times higher in infants born to relatives with a higher genetic predisposition [10,11,13,18]. It is the fact that mortality in combined bronchoesophageal adhesions and oesophageal malformations exceeds 85% that causes infants to die from aspiration pneumonia in the early days of the early neonatal period [1,7,8,12,14]. This, in turn, requires focusing on the morphological aspects of finding a solution to the problem and developing methods for the expression of mutated genes and targeted therapy based on molecular genetic testing.
2. Materials and Methods of Research
As a material for the formation of materials for the autopsy of infants who died as a result of abnormalities in the development of the esophagus, and infants who underwent surgery on the esophagus and died without it. In 18 cases, esophageal contents were taken from them. The finished samples were examined morphologically. Morphology: hematoxylin was stained with eosin dye.
3. Research Aim
The study of specific pathomorphological changes that occur in the clinical and morphological variant of 3 anomalies of the esophagus.
4. Discussion and Conclusions
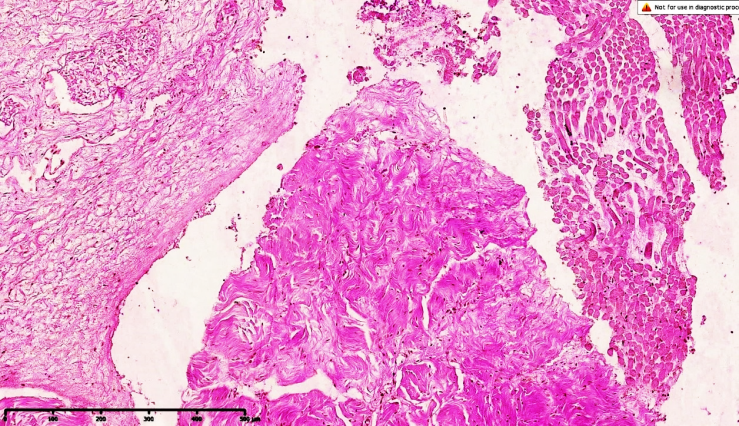
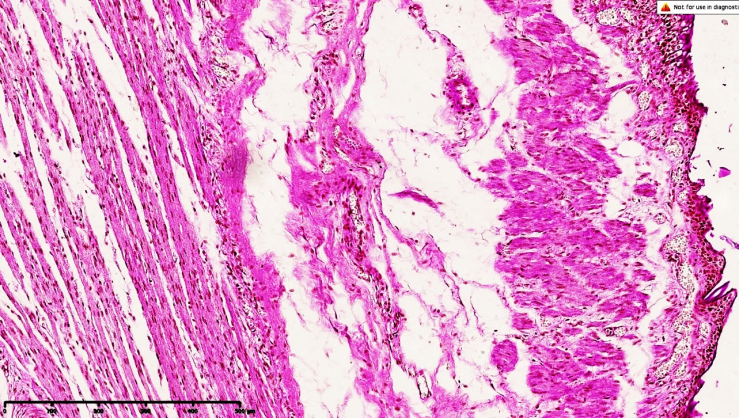
The 4th variant of esophageal atresia. The main morphological changes are atresia of the proximal trachea and esophagus, the total atresia of the esophagus is 2%. In this variant, the wall of the esophagus has dysplasia and a section of stenosis, and the patency of the esophagus is morphofunctionally impaired. In this species, esophageal atresia is incomplete and semi-permeable and can occur in the proximal, distal, and middle triads.We remind that the development of esophageal atresia is explained by the fact that in this 4th variant, if we take into account the development of esophageal atresia along with other systemic tissues around the complex or in the alloxide, the wall of the esophageal stenosed area is not fully formed in the perinatal development of anatomical layers, mainly morphofunctional parameters of the mucous membrane.The fact that the MALT structure located on the mucous and submucosa is not fully formed, and the number of intraepithelial lymphocytes is significantly reduced, means that primary and acquired immunodeficiency occurs on average in 30% of children born with this defect.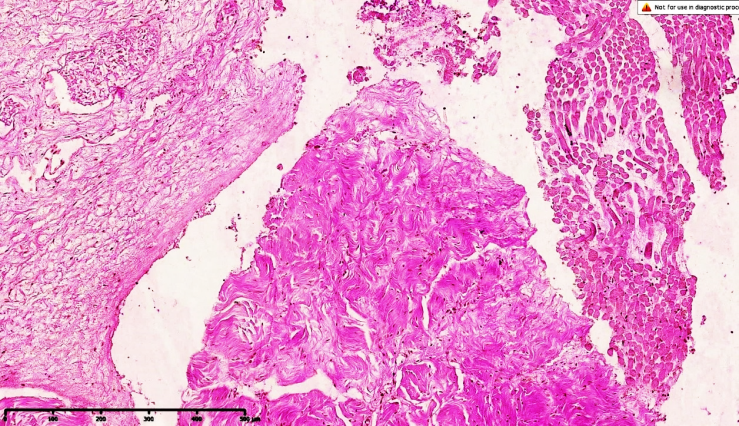 | Figure 1. Esophageal atresia in variant 4, morphological view of the upper part. Foci of trembling of transverse muscle bundles are found along the perimeter of the esophageal junction, and an increase in connective tissue components from sparse fibers is observed in the gap |
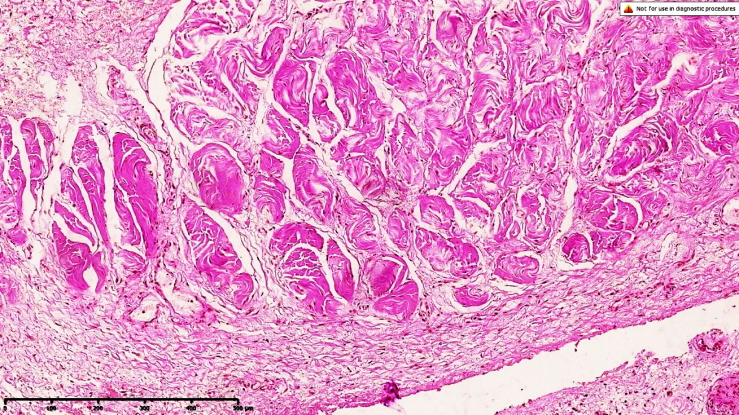
Undulating foci of elastic fibers appear on the mucous membrane. Interlayer tumors form on all floors, which are detected along with massive filling of blood vessels. Dye G.E. Is10x10 in size.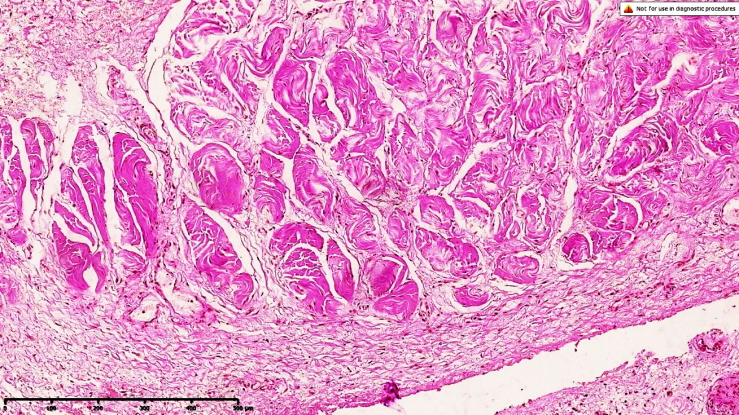 | Figure 2. Esophageal atresia in variant 4, foci of myofibrosis form between the transverse muscle bundles, the upper end of which is located on the muscular floor, elastic fibers in the adventitial floor tremble, interstitial edema in the lumbar region, there are signs of overflow of small-caliber blood vessels. Dye G.E. Is 10x10 in size |
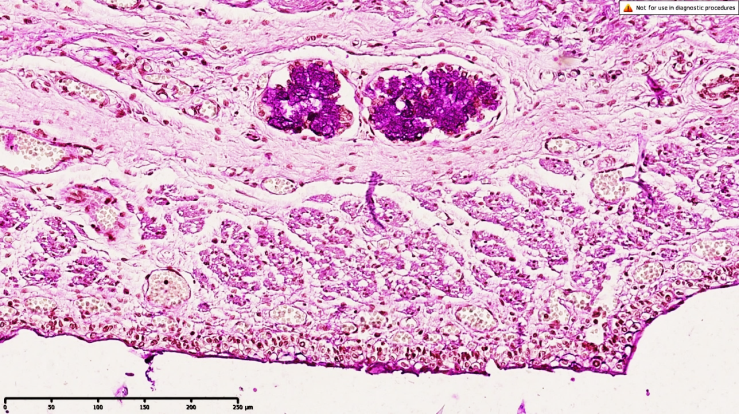
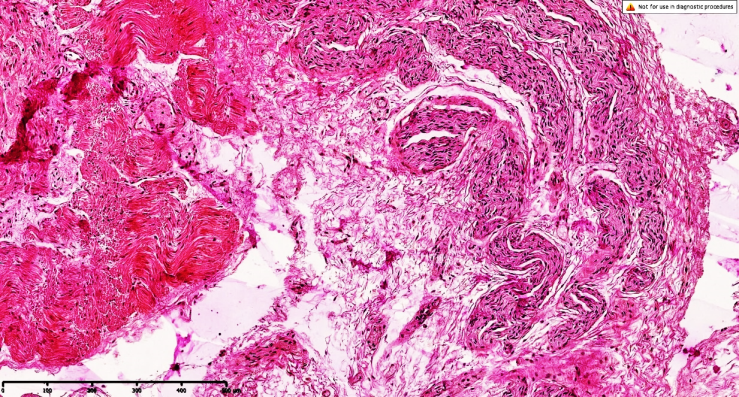
This is manifested clinically and morphologically in patients with esophageal stenosis. It consists, reflecting the essence of morphological changes in areas that have undergone stenosis, in the fact that anatomical floors are not fully formed, food residues stagnate in these areas, dysphagia and impaired peristalsis of the esophagus are clinically manifested.The study of morphological changes revealed the following. In particular, the multilayer squamous epithelium covering the mucous membranes of the esophagus is characterized by the presence in these areas of single-layered cuboid and desquamated prismatic epithelial cells, a thin fibrous boundary projection of the basement membrane between the mucous membrane and the mucous membranes lining the mucous membrane, in an unevenly thinned form. External view. The mucous membrane is manifested by superficial erosive changes in these areas, the formation of a local inflammatory infiltrate. This is evidenced by the fact that infants develop painful symptoms caused by the lesion of these areas with protein clots of dairy products.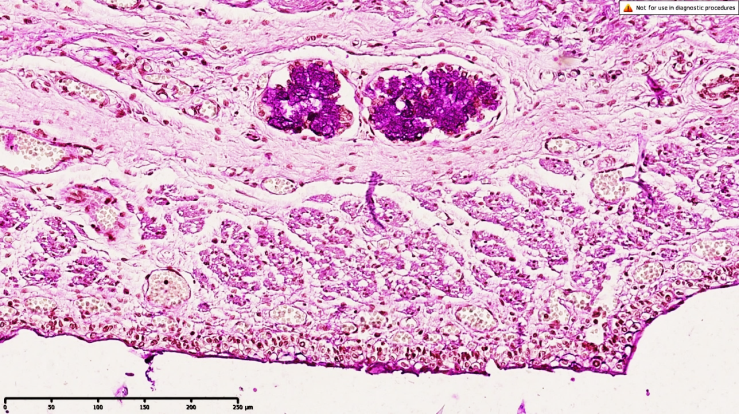 | Figure 3. Esophageal atresia in variant 4, tubular alveolar glandular tissue with a middle tip located on the mucous membrane, surrounded by sparse fibrous connective tissue forming a border around the perimeter of the gland, confirms the low morphofunctional activity of the gland, the presence of a small number of scattered intraepithelial lymphocytes on the mucous membranes and mucous membranes of the mucous membranes is determined. Intermediate tumors form at all anatomical levels, and the proliferation of connective tissue with sparse fibers is determined at all anatomical levels. On the surface of the mucous membrane, it is determined that the epithelial coating is not fully formed. Figure is 10x10 in size. The remaining areas of the mucous membranes appear to be formed in accordance with gestational age, and it is determined that these are multilayer squamous epithelial cells. At the borders of the enlarged and stenosed mucosa, a multilayer epithelial coating 200 times larger was found, consisting in appearance of 1-3 layers, with single-layered semi-prismatic and cuboid epithelial cells in the border area |
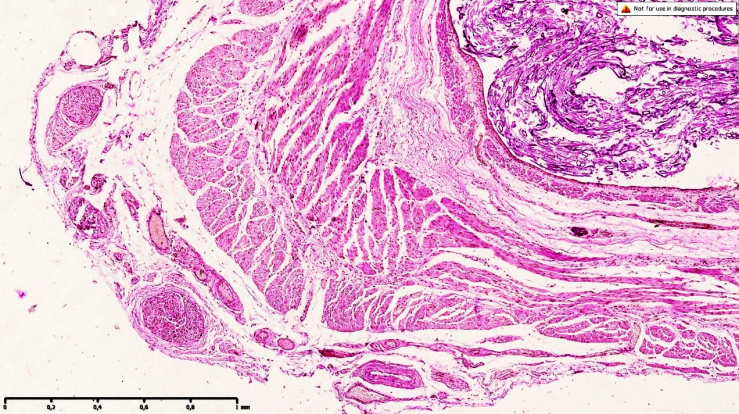
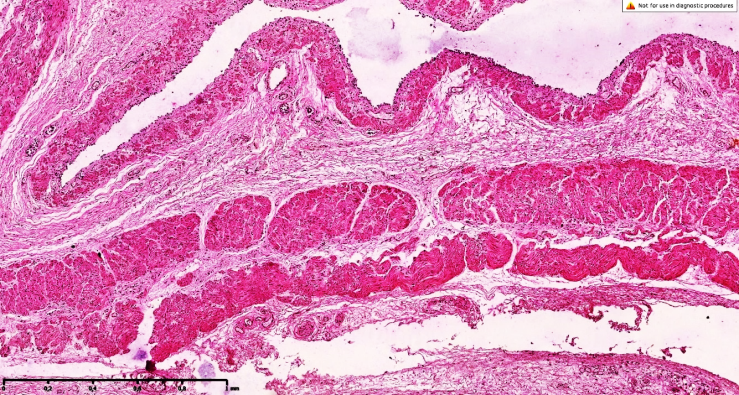
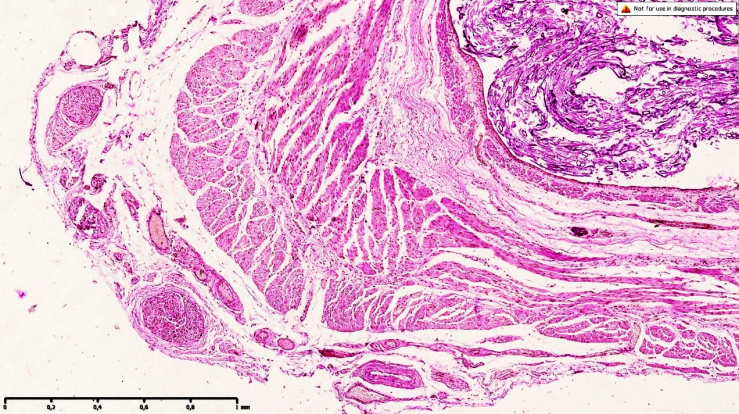 | Figure 4. Esophageal atresia in variant 4, morphological type of the middle triad. The thickness of the muscle layer of the esophagus is different, it is in the zones of myofibrosis and myosclerosis that foci of connective tissue are detected, revealing coarse fibrous tachylaxis, mucosa and mucus-like membranes of different thickness, on the adventitial floor there is a sharp fullness and preserved foci of unformed muscle rudiments. On the surface of the mucous membrane, it is determined that the epithelium is not fully formed. Dye G.E. Is 4x10 in size |
This is mainly manifested by permanent damage to the border areas during peristalsis of the esophagus. With stenoses of the distal esophagus at the border of the Z-shaped line, in the area of transition to multilayer and single-layered prismatic epithelium, fovea-like morphological features, prismatic epithelial plates with metaplasia are revealed. The persistence of intermediate tumors on the mucous membranes confirms the presence of hemodynamic disorders. It was found that there was a quantitative decrease in intraepithelial lymphocytes in the mucous membranes. It also determines the uneven filling of small-caliber and capillary blood vessels, the presence of perivascular tumors, mucoid staining in sparse fibrous structures, focal accumulation of histiocytes, fibroblasts in perivascular zones and the presence of mesenchymal cells along the perimeter of the mucous membrane of the basement membrane.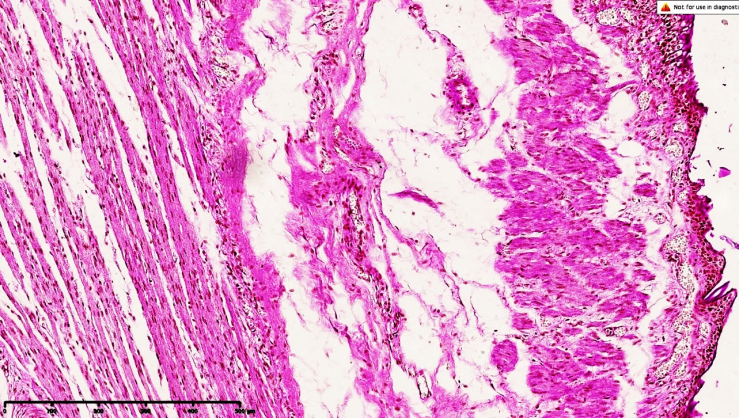 | Figure 5. Esophageal atresia in variant 4, morphological appearance of the middle triad. Foci of inflammatory infiltrate in the mucomuscular bottoms and areas of myofibrosis in the muscles are detected in the wall of the esophagus, and the histoarchitectonics of muscle tissue can be traced along the pelvis, with a sharp development of intermediate tumors around it, components of sparse fibrous connective tissue are isolated, trembling along the perimeter of the muscle bundles. identified. The surface of the mucous membrane has uneven thickness, which exactly corresponds to the areas where it undergoes stenosis. A general dye staining is 10x10 in size |
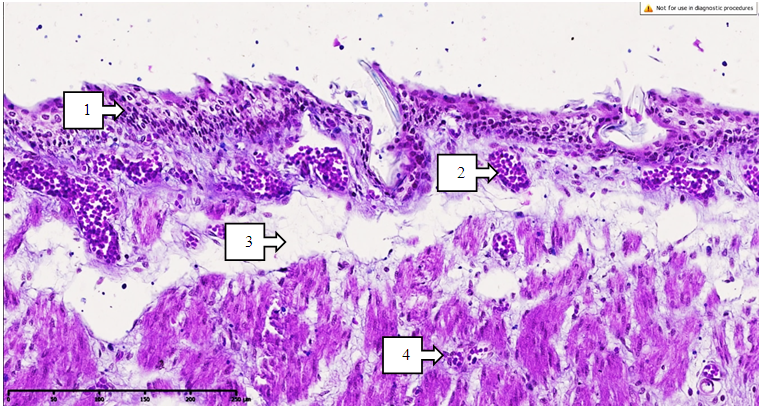
This confirms that the development of hypoxia in the process, increased synthesis of tropocollagen by fibroblasts, is clearly developed in stenosed areas. This means that the process ends with an increase in connective tissue formed by sparse fibers and a strong development of constrictions. The detection of glandular structures in these areas of the mucous membrane only in the deuterine focus, the formation of foci of cystic expansion of the formed glands and the absence of morphofunctional swollen secretions in the stenosed sacs, constant mechanical friction of the mucous membrane and the chronic occurrence of erosive foci (see Figure 3).The mucous membrane confirms that areas of contracture with a wave-like appearance in the muscle bundles, interstitial tumors formed in the gap, and chronic inflammation in which foci of lymphocytic infiltration form sluggishly around blood vessels (see Fig. 5), focal proliferation of histiocytes and fibroblasts in the muscle area also means that there is an increase in sparse and coarse fibrous structures during work.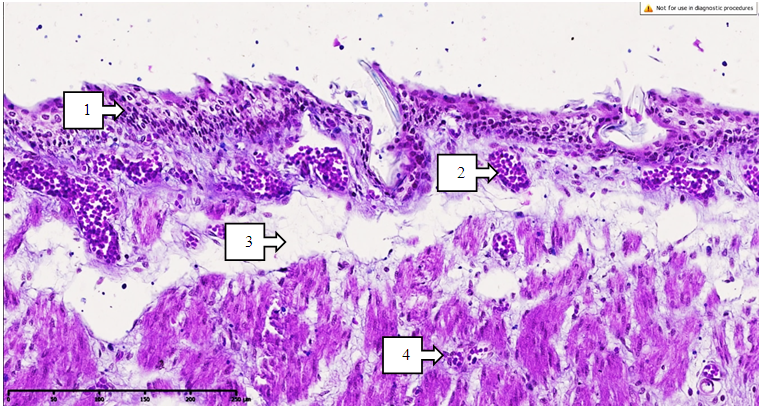 | Figure 6. Esophageal atresia in variant 4, the area of the middle triad is the surface of the mucous membrane. The mucous membrane is not fully formed, it is of different thickness (1), massive thickening has developed in the blood vessels (2), interstitial tumors have developed sharply at the borders of the mucous membrane and mucous membranes (3), sparse fibrous connective tissue between the private muscles of the layer has increased on the mucous membrane, foci of lymphocytic infiltration have formed (4). Dye G.E. Is 10x10 in size |
This confirms that the process of esophageal wall stenosis continues. Nerve plexuses are found in the mucous membrane, there is an increase in connective tissue with sparse fibers around the plexuses, fullness of blood vessels, the development of foci of lymphostasis in the lymph vessels, the morphofunctionality of the esophagus is manifested by a constant violation of peristalsis. One notable aspect is that very few glandular structures in the mucous membranes are undetectable, especially in areas that have undergone stenosis, making it difficult for mucus to reach the mucous membranes and changes the taste of food.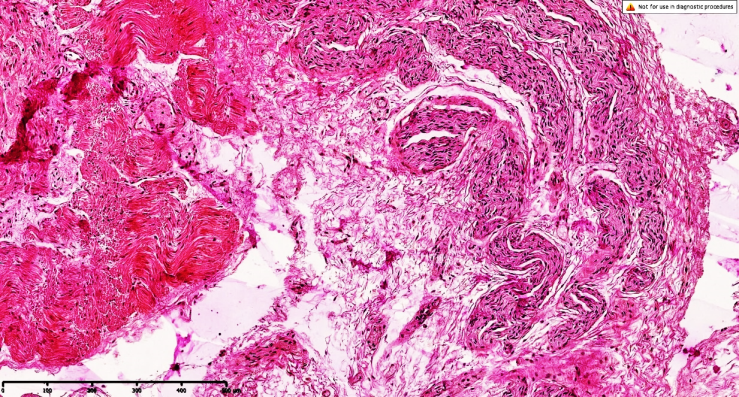 | Figure 7. Esophageal atresia in variant 4, morphological appearance of the middle triad. An increase in the components of sparse fibrous connective tissue is detected along the perimeter of the esophageal junction, the mucous membrane and mucous membranes are not fully formed. On the surface of the mucous membrane, it is determined that the epithelium is not fully formed. Dye is 10x10 in size |
Since thickening of the muscle layers is found in normal structures in the direction of the esophagus from the larynx to the stomach, these changes have different thicknesses in anomalies, which leads to the development of a stenosing process in the wall of the esophagus. At the moment, the essence of our research work also lies in the morphological determination of its manifestation, and in this case it is necessary to determine whether the treatment of patients manifests itself mainly in a conservative way, by stopping pathogenetic changes that prevent the occurrence of the above-mentioned morphological signs. Along the perimeter of the muscle bundles located on the muscular floor, most elastic fibers are characterized by the evolutionary appearance of foci of scarring in the form of elastofibrosis.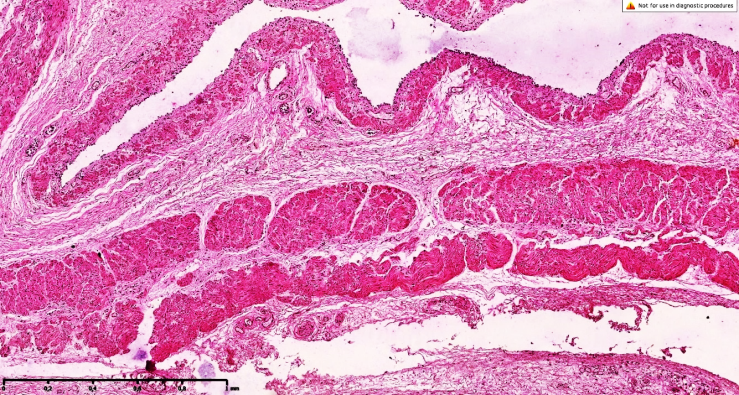 | Figure 8. Esophageal atresia in variant 4, morphological view of the lower part. An increase in connective tissue components with sparse fibers is detected along the perimeter of the esophageal junction, and the mucous membrane is not fully formed. On the surface of the mucous membrane, it is determined that the epithelium is not fully formed. Dye is 10x10 in size |
Morphological changes of a wave-like appearance, in which the mucous membrane trembles with muscle bundles and undergoes myofibrosis, confirm that disorders in the peristalsis of the esophagus occur constantly. Foci of connective tissue are found in the elastic fibers of the mucous membrane, which also undergo organization by detecting tachomyl with fibrous coarse fibers. The surface of the mucous membrane is also uneven, and weak foci of lymphohistiocytic infiltration are found in places of erosive damage. It is determined that a sharp hyperemia has developed on the mucous membrane of these areas, which is assessed macroscopically by foci of redness and erosive changes in the mucous membrane.The proximal part is located on the transverse muscular floor, the sutures are smooth, the boundaries of the circular and longitudinal muscles are clear, the average fullness of the blood vessels is determined. These morphological features are mainly found in those parts of the esophagus that have already formed. At the bottom of the muscles in the places of their stenosis, the tendons are uneven, the cytoplasm is light in color, and the transverse bulge is apparently absent, and these are signs of morphofunctional insufficiency. The muscle bundles have a wave-like character, mainly foci of contracture of 2-3 degrees. It is these foci that manifest clinically and morphologically as symptoms of dysphagia in existing areas, which means that during treatment, injury to these areas of the muscle tendons continues with the elimination of esophageal peristalsis.
5. Conclusions
Consequently, the following changes are observed in esophageal atresia in 4th variant: an increase in the sparse and coarse fibrous connective tissue between the muscle layers where the wall of the esophagus has a round and longitudinal shape, signs of impaired contractility of the muscle layers during atresia, myofibrosis, the appearance of foci of myosclerosis and thickening of the esophageal wall. They allow to strengthen the stenosis process and predict.At the same time, the presence of full-fledged venous outflows in the blood vessels of the muscular fundus allows us to assess whether peristalsis continues in the muscle layers during non-synchronous contractions. The presence of a basal layer of different thickness between the muscular and adventitial layers also confirms the morphological changes presented above.
References
| [1] | Sukalo A., Kozlovskiy A. Gastroenterologiya i diyetologiya v detskom vozraste. – Litres, 2022. Sukalo A., Kozlovsky A. Gastroenterology and dietetics in childhood. – Litres, 2022. |
| [2] | Akhrarova F. Vliyaniye displazii soyedinitel'noy tkani na techeniye gastroenterologicheskikh zabolevaniy u detey // Pediatriya. – 2023. – T. 1. – №. 1. – S. 380-386. Akhrarova F. The effect of connective tissue dysplasia on the course of gastroenterological diseases in children //Pediatrics. – 2023. – Vol. 1. – No. 1. – pp. 380-386. |
| [3] | Soboleva M. K., Kinsht D. A. Vrozhdennyye poroki i malyye anomalii razvitiya u novorozhdennykh v zavisimosti ot vida preodolennogo besplodiya i zdorov'ya roditeley // Meditsinskiy sovet. – 2021. – №. 11. – S. 22-28. Soboleva M. K., Kinsht D. A. Congenital malformations and minor developmental anomalies in newborns, depending on the type of infertility overcome and the health of parents //Medical Council. – 2021. – №. 11. – Pp. 22-28. |
| [4] | Choi G, Je BK, Kim YJ. Gastrointestinal Emergency in Neonates and Infants: A Pictorial Essay. Korean J Radiol. 2022 Jan; 23(1): 124-138. |
| [5] | Madeleine A, Audrey N, Rony S, David S, Frédéric G. Long term digestive outcome of oesophageal atresia. //Best Pract Res Clin Gastroenterol. 2022 Feb-Mar; 56-57. |
| [6] | Sadreameli SC, McGrath-Morrow SA. Respiratory Care of Infants and Children with Congenital Tracheo-Oesophageal Fistula and Oesophageal Atresia. Paediatr Respir Rev. 2016 Jan; 17: 16-23. |
| [7] | Boybeyi-Turer O, Iyigun I, Cagan M, Celik HT, Ozyuncu O, Soyer T. A rare congenital esophageal anomaly mimicking an isolated esophageal atresia: Kluth Type IV membranous esophageal atresia. Congenit Anom (Kyoto). 2021 Nov; 61(6): 208-211. |
| [8] | Ge Y, Xu B, Shi J, Tang W. Application value of high-frequency ultrasound combined with ultrasonography in the diagnosis of neonatal esophageal atresia. Afr Health Sci. 2023 Sep; 23(3): 547-553 |
| [9] | Chernetsova E, Agarwal A, Weir A, Oltean I, Barkey J, Demellawy DE. Diagnostic Value of Mid-oesophageal Biopsies in Pediatric Patients With Eosinophilic Esophagitis. Pediatr Dev Pathol. 2021 Jan-Feb; 24(1): 34-42. |
| [10] | Wechsler JB, Bolton SM, Gray E, Kim KY, Kagalwalla AF. Defining the Patchy Landscape of Esophageal Eosinophilia in Children with Eosinophilic Esophagitis. Clin Gastroenterol Hepatol. 2022 Sep; 20(9): 1971-1976.e2. |
| [11] | Rohanizadegan M, Tracy S, Galarreta CI, Poorvu T, Buchmiller TL, Bird LM, Estroff JA, Tan WH. Genetic diagnoses and associated anomalies in fetuses prenatally diagnosed with esophageal atresia. //Am J Med Genet A. 2020 Aug; 182(8): 1890-1895. |
| [12] | Best C, Sudel B, Foker JE, Krosch TC, Dietz C, Khan KM. Esophageal stenting in children: indications, application, effectiveness, and complications. //Gastrointest Endosc. 2009 Dec; 70(6): 1248-53. |
| [13] | Schmedding A, Wittekindt B, Schloesser R, Hutter M, Rolle U. Outcome of esophageal atresia in Germany. // Dis Esophagus. 2021 Apr 7; 34(4): doaa093. |
| [14] | Mukhsinova M.Kh., Eshbayev E.A., Zufarov A.A. Pathomorphological Changes in Esophageal Anomalies in Newborns. // American Journal of Medicine and Medical Sciences. 2024; 14(12): 3462-3464. |
| [15] | Gayle JA, Gómez SL, Baluch A, Fox C, Lock S, Kaye AD. Anesthetic considerations for the neonate with tracheoesophageal fistula. Middle East J Anaesthesiol. 2008 Oct; 19(6): 1241-54. |
| [16] | Pinheiro PF, Simões e Silva AC, Pereira RM. Current knowledge on esophageal atresia. //World J Gastroenterol. 2012 Jul 28; 18(28): 3662-72. |
| [17] | Paul M, Bamba C, Vinay V, Krishna B; Bharani Kumar B.1. Comparing Opioid with Opioid-free Anesthesia Technique in Neonates Undergoing Tracheoesophageal Fistula Repair. Oman Med J. 2023 Sep 28; 38(5): e547. |
| [18] | Fukuta A, Kamimura T, Furuno W, Yamamoto J, Yokota C, Omura S. Abdominal esophageal banding for esophageal atresia with tracheoesophageal fistula in neonates with severe associated anomalies. Pediatr Surg Int. 2021 Feb; 37(2): 261-266. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML