-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 165-168
doi:10.5923/j.ajmms.20251501.30
Received: Dec. 21, 2024; Accepted: Jan. 19, 2025; Published: Jan. 26, 2025

Parameters of the Complex of Retinal Ganglion Cells and Optic Disc During Phacoemulsification of Cataracts in the Background of Advanced Stage of Primary Glaucoma
Nabiev Abduvali Mirzaliyevich1, Zokhidov Obidbek Ulugbek Ugli2
1DSc, Chief Physician of the Tashkent regional branch of the Republican Specialized Scientific and Practical Medical Center for Eye Microsurgery, Tashkent, Uzbekistan
2PhD Student, Republican Specialized Scientific and Practical Medical Center for Eye Microsurgery, Tashkent, Uzbekistan
Correspondence to: Nabiev Abduvali Mirzaliyevich, DSc, Chief Physician of the Tashkent regional branch of the Republican Specialized Scientific and Practical Medical Center for Eye Microsurgery, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Relevance. Combined pathology such as primary glaucoma with complicated cataract is one of the leading causes of blindness in the world. Purpose of the study. To study the effect of ultrasound on the thickness of retinal ganglion cells and the optic disc during cataract phacoemulsification in patients with advanced (III) stage of primary glaucoma. Material and methods. We analyzed OCT parameters in 72 patients with advanced stage primary glaucoma before and after cataract phacoemulsification surgery. Results and conclusion. It was established that, after phacoemulsification of cataracts in patients with primary glaucoma, the study of the parameters of the GCC complex using optical coherence tomography showed a decrease in the average thickness of the GCC complex and the dependence of OCT parameters on the density of the cataract.
Keywords: Glaucoma, Cataract, GCC, Phaco, Optical coherence tomography
Cite this paper: Nabiev Abduvali Mirzaliyevich, Zokhidov Obidbek Ulugbek Ugli, Parameters of the Complex of Retinal Ganglion Cells and Optic Disc During Phacoemulsification of Cataracts in the Background of Advanced Stage of Primary Glaucoma, American Journal of Medicine and Medical Sciences, Vol. 5 No. 1, 2025, pp. 165-168. doi: 10.5923/j.ajmms.20251501.30.
1. Introduction
- The prevalence of combined pathology, such as primary glaucoma and cataracts, varies from 17.0 to 38.6% of cases. The main method of treating cataracts against the background of primary glaucoma (PG) is phacoemulsification of cataracts (phaco) with low-frequency ultrasound (US) [8,10].Studying the problem of the influence of low-frequency ultrasound on the internal structures of the eye remains one of the unsolved problems. The existing concept is based on the study of the relationship between ultrasound during phaco and changes in eye tissue, which is dose-dependent [2,6,9]. Even minimal exposure to low-frequency ultrasound has biological effects. This is explained by the fact that under the influence of low-frequency ultrasound during phaco, not only visible cavitation effects occur, described in the ophthalmological literature as causing structural morphological damage to eye tissue, but also sound-chemical reactions [1,4]. It has been experimentally proven that the threshold for the occurrence of intracellular sonochemical reactions is only 0.02-0.04 W/cm², and for the emulsification of two oil-water media at an ultrasound frequency of 40 kHz, an intensity of at least 0.3-0.4 W/cm² is required. The occurrence of sound-chemical reactions contributes to the emergence of collapsing microbands several microns in size that disrupt bimolecular bonds [3,5,7,10].However, the research conducted on this issue is not unambiguous. In this regard, the study of the effect of phaco on the visual-nervous apparatus of the organ of vision in patients with advanced stages of PG becomes particularly relevant and requires further studies. Financial transparency: None of the authors have a financial interest in the materials or methods presented.There is no conflict of interest. Purpose of the study. To study the effect of low-frequency ultrasound during phacoemulsification of cataract on the thickness of the complex of retinal ganglion cells and optic disc in patients with advanced stage of primary glaucoma.
2. Material and Methods
- We analyzed data from OCT studies in 72 patients (72 eyes) with advanced stage PG in combination with cataracts of II (40 eyes) and III degree (32 eyes) density (according to L. Buratto, 1999). Of these, 40 patients (55.5%) were diagnosed with primary open-angle glaucoma (POAG) and 32 (44.5%) were diagnosed with primary angle-closure glaucoma (PCAG). Distribution by gender: women - 38 and men -34. The age of the patients was from 40 to 69 years (average was 63.3±4.1 years). Of these: from 40 to 49 years old - 11 patients, from 50 to 59 - 15 patients and from 60 to 69 - 19 patients. The duration of the disease (glaucoma) ranged from 3 years to 12 years, on average 8.1 ± 3.4 years. In patients with POAG, the II degree of cataract density was established in 20 eyes, the III degree of density – in 18. Accordingly, with POAG, the II degree of cataract density was established in 18 and the II degree of density – in 10 eyes. The criterion for selecting patients was an OCT signal strength index of at least 18 (with a lower signal strength, the data obtained were unreliable). The control group consisted of 30 patients (40 eyes) with cataracts of density degrees II and III, corresponding to age and gender.Patients were examined by general ophthalmological and specific diagnostic methods: visometry, autorefractometry, non-contact tonometry, computer perimetry, ultrasound A, B - scanning, tonometry with a 5.0 g load (according to Maklakov), ultrasound biomicroscopy (UBM), biomicroscopy, optical coherence tomography (OCT) . OCT was performed using a 3D OCT-1 Maestro unit (TOPCON, Japan). The study of the optic disc area was performed using the “Optic Disc Cube 200x200” protocol with data processing using the “ONH and RNFL OU Analysis” protocol. The greatest importance was attached to the average thickness of the RNFL (Average RNFL Thickness). Scanning of the macular area was carried out according to the “Macular Cube 512x128” protocol, followed by analysis of retinal thickness “Macular Thickness Analysis”. The average GCC thickness (GCC Average) is calculated, its value for the upper (GCC Superior) and lower (GCC Inferior) segments. To assess the normality of the distribution of study results, the Kolmogorov–Smirnov test was used.The most convenient and optimal for all stages of work with the II degree of lens density were a needle with an angle of 30°, digital vacuum parameters of 350 mm Hg, ultrasound - 25-30%. With the third degree of lens density, the vacuum parameters were 350-400 mm Hg, ultrasound - 30-40%. Statistical processing was carried out using Excel (Microsoft). Differences were considered significant at p<0.05.
3. Results
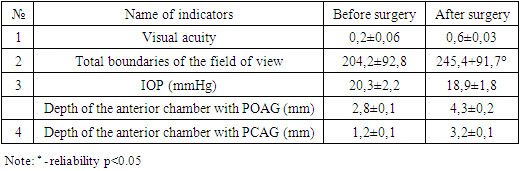
- During the initial examination of patients, regardless of the form of the disease, visual acuity with 2nd degree cataract density was at the level of 0.3 to 0.5, with 3rd degree density – 0.1-0.3. The boundaries of the visual field in 62 eyes along the nasal meridian were 10-15 degrees from the fixation point. In 8 eyes (5 eyes with PCAG and 3 eyes with POAG), the visual field was “tubular” and the boundaries ranged from 3 to 15 degrees along different meridians and on average the sum of visual field boundaries was 115.3±9.0°. In 53 patients (53 eyes), in preparation for phacoemulsification, antiglaucomatous operations were performed in advance and their IOP was at the level of 17.0-20.0 mm Hg. In 19 patients (19 eyes), IOP was normalized by one of the combined antihypertensive drugs and were at the level of 19.0 – 22.0 mm Hg. It should be noted that the above data did not differ significantly between POAG and PCAG. When performing phaco, the depth of the anterior chamber may have a certain significance, especially with PCAG. In the advanced stage of PCAG, the anterior chamber of the eye is shallow, damage to the corneal endothelium and the development of keratopathy are possible, which requires a gentle approach.The average data on visual acuity, visual field, IOP level, and anterior chamber depth before and after surgery are shown in Table 1.
|
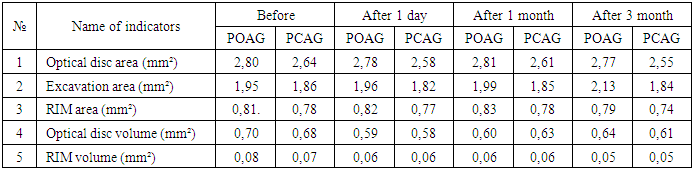
 | Table 2. Retinal thickness and GCC parameters before and after surgery |
|
4. Discussion
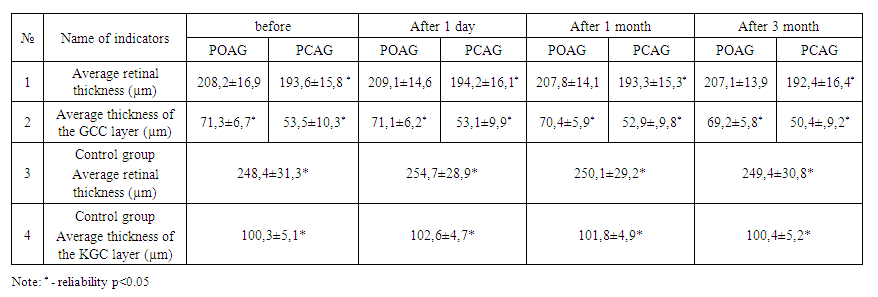
- Thus, 1 month after cataract FE with low-frequency ultrasound in 11.1% of cases and after 3 months in 19% of cases, the thickness of the retina and MCG became thinner. According to a number of authors, low-frequency ultrasound during FEC in PG can contribute to the occurrence of sound-chemical reactions on retinal nerve cells, thereby causing their death. These indicators indicate the possible role of low-frequency ultrasound in the development of GON. According to Quigley H.A. et al [2006], the death of retinal ganglion cells (RGCs) in PG begins long before the first manifestations of visual functional disorders. In advanced stages of primary glaucoma, a significant part of the RGCs are already damaged [11]. Thanks to the use of the diagnostic method optical coherence tomography (OCT), it became possible to separately analyze the thickness of the three inner layers of the retina that make up the ganglion cell complex: nerve fibers, ganglion cells and the inner plexiform layer, containing, respectively, axons, cell bodies and dendrites GCC [12,14]. The information content of the results of an OCT study in a combination of primary glaucoma and cataract can be significantly affected by the degree of opacification and density of the lens [13]. Our data on changes in retinal thickness and GCC in grade III cataract density against the background of an advanced stage of PG in patients with a “tubular” visual field indirectly confirm this opinion.
5. Conclusions
- The study of the parameters of the RGC complex using optical coherence tomography showed a high diagnostic accuracy of the indices and a decrease in the average thickness of the RGC complex in primary glaucoma and the dependence of OCT indicators on the density of the cataract. Data from OCT parameters in patients with PG showed changes within 3 months, in 19% of cases, and possibly reflect damage to the GCL complex by low-frequency ultrasound during phacoemulsification.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML