-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 140-144
doi:10.5923/j.ajmms.20251501.26
Received: Dec. 20, 2024; Accepted: Jan. 22, 2025; Published: Jan. 26, 2025

Improving Diagnostic and Treatment Methods for Valgus Deformity of the Elbow Joint
I. Y. Khodjanov1, Sh. F. Ubaidullaev2, Sh. K. Khakimov2
1Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics, Tashkent, Uzbekistan
2Bukhara State Medical Institute named after Abu Ali Ibn Sino, Bukhara, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article analyzes data from 46 patients with valgus deformity of the elbow joint who underwent two types of surgical intervention depending on the severity of the deformity, the duration of trauma, and the age of the patients. For the first group of patients (n=16), corrective supracondylar osteotomy of the humerus and osteosynthesis using the Ilizarov apparatus were performed. For the second group (n=30), pseudarthrosis resection combined with corrective supracondylar osteotomy of the humerus and osteosynthesis using the Ilizarov apparatus and screws was used. These methods contribute to forming the distal part of the humerus and restoring elbow joint function.
Keywords: Humeral condyle head, Pseudarthrosis, Osteotomy, Osteosynthesis
Cite this paper: I. Y. Khodjanov, Sh. F. Ubaidullaev, Sh. K. Khakimov, Improving Diagnostic and Treatment Methods for Valgus Deformity of the Elbow Joint, American Journal of Medicine and Medical Sciences, Vol. 5 No. 1, 2025, pp. 140-144. doi: 10.5923/j.ajmms.20251501.26.
Article Outline
1. Introduction
- Most musculoskeletal injuries in children involve damage to the elbow joint. Globally, the treatment of elbow joint injuries in children presents significant challenges and remains one of the pressing issues in pediatric traumatology [1,2,3]. These challenges are characterized by the diversity of elbow joint injuries in children, the reactive response of the elbow joint to trauma, and the accelerated reparative processes typical for this age group [4,5].In many cases, due to continued growth of the elbow area after treatment, surgical interventions, or even delayed treatment, these deformities persist into adulthood. Differences in bone healing times at various ages limit the possibility of treating deformities uniformly across all ages [6,7]. Diagnostic and treatment methods for elbow joint deformities are primarily designed for patients under 10–12 years of age, yielding better outcomes in this demographic. However, as patient age increases, treatment efficacy decreases, and the complication rate rises [8,9].The primary factor leading to valgus deformity of the elbow joint is peripheral neurotrophic changes resulting from axonotmesis of the ulnar nerve, typically caused by pseudarthrosis of the humeral condyle head. In complex cases of valgus deformity, the timing, scale, and selection of appropriate treatment strategies become significantly more challenging [10,11].ObjectiveTo improve treatment outcomes by enhancing diagnostic and therapeutic methods for patients of varying ages with valgus deformity of the elbow joint.
2. Materials and Methods
- This study observed 46 patients treated between 2018 and 2024 for valgus deformity of the elbow joint in the Second Department of General Orthopedics at the Republican Center of Traumatology and Orthopedics, Ministry of Health of the Republic of Uzbekistan. Clinical and laboratory studies, radiographic examinations, tomographic studies of the dynamically affected segment, and electromyography of the arm segment compared to the healthy limb were performed for all patients.An electronic calculation scheme was developed based on clinical and radiographic findings, enabling control over the severity of valgus deformity in the elbow joint caused by pseudarthrosis of the humeral condyle head.
3. Results and Discussion
- The distribution of patients admitted for valgus deformity of the elbow joint (following trauma sustained more than 12 months prior) was analyzed by age and sex. Patients’ ages ranged from 3 years and older. Based on the data, all patients were divided into five age groups according to the WHO classification (2019):• 3–7 years: 9 patients (5 boys and 4 girls)• 7–11 years: 20 patients (15 boys and 5 girls)• 11–15 years: 13 patients (9 boys and 4 girls)• 15 years and older: 4 patients (3 boys and 1 girl)A retrospective analysis revealed that the primary causes of pseudarthrosis in the humeral condyle head were late diagnosis or misinterpretation of clinical data, poor treatment strategy selection, reduced adherence to orthopedic regimens, and especially noncompliance among boys.
4. Surgical Techniques Applied
- Patients were divided into two groups based on the severity of the elbow joint deformity, the duration of trauma, and the age of the patients:Group 1 (Comparison Group)• Number of patients: 20 (43.5%; 16 boys, 4 girls).• Procedure: Two-stage surgery: 1. Stage 1: Resection of pseudarthrosis and osteosynthesis using the Ilizarov apparatus.2. Stage 2: Corrective supracondylar osteotomy of the humerus and osteosynthesis using the Ilizarov apparatus.This approach was predominantly applied to middle and older school-aged children, as these patients often exhibited peripheral neurotrophic conditions, leading to muscle atrophy in the hand and wrist, exacerbating valgus deformity. Over time, complete resorption of the distal humerus occurred, forming pseudarthrosis of the humeral condyle head. For this group, the surgical intervention primarily aimed to eliminate valgus deformity while preserving elbow joint range of motion. Performing intra-articular and extra-articular reconstructive surgeries in older children significantly increased the risk of contractures, which required lengthy recovery periods (3–3.5 months) and intensive physiotherapy.Group 2 (Main Group)• Number of patients: 26 (56.5%; 15 boys, 11 girls).• Procedure: Advanced surgical techniques for treating pseudarthrosis of the humeral condyle head and valgus deformity. This included pseudarthrosis resection, corrective supracondylar osteotomy of the humerus, and osteosynthesis using the Ilizarov apparatus and screws.Patients in this group predominantly presented with Grade 2 and 3 severity of valgus deformity (according to AKP classification). They also exhibited neurotrophic disorders and subsequent aseptic necrosis of the humeral condyle head. The new surgical method emphasized preserving soft tissue elements as a source of blood supply, performing corrective supracondylar osteotomy, and stabilizing bone fragments with screws and the Ilizarov apparatus. Fixation time using the Ilizarov apparatus was approximately 4–6 weeks.Postoperative recovery required correcting the arm's axis to fully restore elbow joint function. Younger patients showed faster and more complete recovery due to their higher regenerative capacity. Over 1–2 years, patients exhibited gradual reconstruction of the distal humerus and restoration of joint functionality. This method is recommended for children over 8–10 years, while younger children benefit from a single-stage surgery involving pseudarthrosis resection and corrective osteotomy using the Ilizarov apparatus.
5. Clinical Case Examples
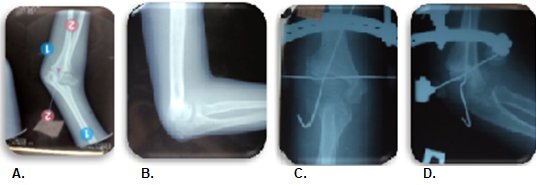
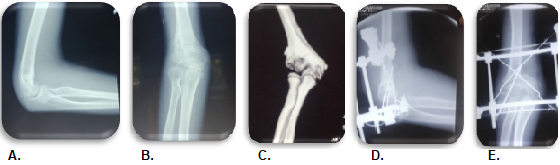
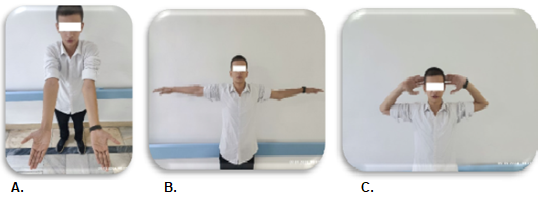
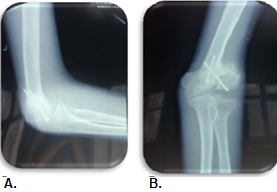
- Patient 1:• Age: 18 years.• History: Sustained trauma in 2016, treated with a plaster cast at a local hospital.• Preoperative findings: Valgus deformity (-38°), flexion (40°), extension (180°), range of motion (140°). Peripheral neurotrophic changes were absent.• Procedure: Pseudarthrosis resection, corrective osteotomy of the humerus, and osteosynthesis using the Ilizarov apparatus and screws.• Outcome: Satisfactory postoperative recovery with no early complications. Joint consolidation was observed within 6 weeks, and joint function improved significantly within 1–2 years.• The mobility and sensitivity of the fingers were preserved, with no peripheral neurotrophic changes detected. Based on clinical and instrumental examinations, the diagnosis was established as: pseudarthrosis of the right humeral condyle head and post-traumatic valgus deformity of the elbow joint (see Fig. 1.a, b, c and Fig. 2. a, b). • In September 2023, the patient underwent a "Resection of the pseudarthrosis and corrective supracondylar osteotomy of the humerus with osteosynthesis using the Ilizarov apparatus and screws" (see Fig. 2. c, d). • The postoperative period was satisfactory, without early postoperative complications. The patient received appropriate medication and physiotherapy. The postoperative wound was predominantly healed, and the patient was discharged on the 9 th day in satisfactory condition. • Analysis of the short- and long-term postoperative outcomes showed consolidation at the humeral joint surface and the distal part of the humerus, with successful anatomical reconstruction of the humeral joint surface (see Fig. 3. a, b, c and Fig. 4. a, b).
 | Figure 1. Patient K., a, b, c: clinical condition of the patient with valgus deformity |
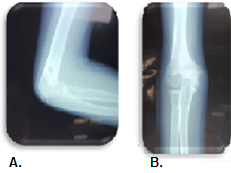
 | Figure 2. Patient K., a, b, c, d: X - rays of the patient, before surgery and postoperative X-rays |
 | Figure 3. Patient K., a, b, c: clinical condition of the patient with the satisfactory of the results |
 | Figure 4. Patient K., a, b, postoperative X - rays of the patient after 1.5 years of surgery |
6. Conclusions
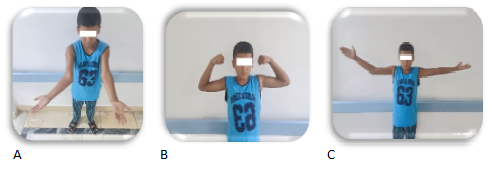
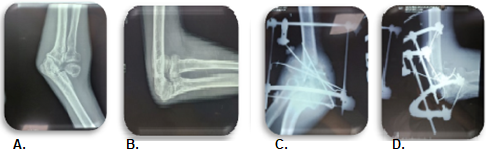
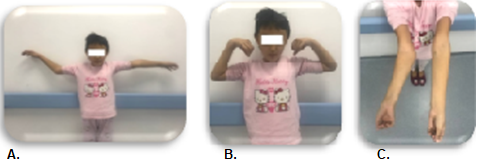
- 1. Valgus deformity of the elbow joint is a complex pathology affecting 7–8% of pediatric cases, leading to early disability in children.2. Tailoring surgical treatment to the severity of the deformity, trauma duration, and patient age significantly improves outcomes.3. Advanced surgical methods enable simultaneous anatomical restoration and functional recovery of the distal humerus, improving elbow joint function in children.4. Hybrid osteosynthesis methods allow for earlier restoration of elbow joint functionality.Second patient T., 14 years old (medical record No. 2459):From the anamnesis: 5 years before admission to our clinic in 2015, the patient sustained an injury, and a plaster cast was applied for the first time in a local hospital. Examination revealed valgus deformity of the elbow joint and weakness of the medial ligaments. Upon examination, the localization of the valgus deformity of the elbow joint showed:• Deformation angle: 35°• Flexion: 33°• Extension: 180°• Range of motion in the elbow joint: 147°The Marx line and Gunther’s triangle were significantly altered. Mobility and sensitivity of the fingers were preserved. Based on clinical and instrumental studies, the diagnosis was made: false joint of the left humeral condyle and post-traumatic valgus deformity of the elbow joint (Fig. 5. a, b, c and Fig. 6. a, b).In June 2021, the patient underwent "Resection of the false joint and osteosynthesis with the Ilizarov apparatus" (Fig. 6. c, d).
 | Figure 5. Patient T., a, b, c: clinical condition of the patient with valgus deformity |
 | Figure 7. Patient T., a, b, c: clinical condition of the patient after surgery (after healing of pseudoarthrosis) |
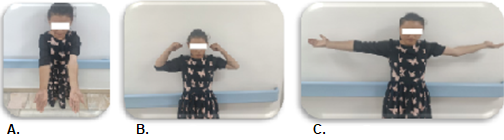 | Figure 9. Patient T., a, b, c: clinical condition of the patient after surgery (correctional osteotomy of the shoulder) |
 | Figure 10. Patient T., a, b: X - rays of the patient, postoperative X-rays (after recovery of the axis of upper extremity) |
7. Summary of the Study and Conclusions
- Introduction:The treatment of fractures of the humeral condyle head and their complications remains a complex and unresolved issue. Many questions, especially concerning the optimal treatment methods for complicated fractures of the humeral condyle head, remain open. This necessitates further research in pediatric traumatology and orthopedics, focusing on diagnostics, improving treatment methods, and preventing difficult-to-manage complications.Postoperative Outcomes:Long-term outcomes were studied for up to 6 years. For objective evaluation and standardization of clinical and radiological data defining pathology, results were compared with the literature. According to Y.P. Soldatov and V.D. Makushin (1997), anatomical and functional criteria were scored as follows:• 14-21 points: Good result• 8-13 points: Satisfactory• 0-7 points: UnsatisfactoryOut of 46 patients:• 40 patients (86.9%) achieved good results.• 6 patients (13.1%) had satisfactory results.Surgical Techniques:Significantly better outcomes were achieved in patients who underwent modified surgical techniques. Despite the traumatic nature of these surgeries, such methods were necessary for cases involving prolonged joint deformation and significant joint element dislocations. Reconstruction of the distal humerus in a “T” shape and fixation with screws or the Ilizarov apparatus were deemed optimal.Both types of surgical techniques should be selected based on the severity of elbow deformity, trauma duration, and the patient’s age. Severe complications like false joints and aseptic necrosis of the humeral condyle head require surgical intervention, such as reconstruction for progressive valgus elbow deformity or late-stage radial nerve neuritis. The use of external fixation devices enables bone fragment stabilization while preserving joint functionality, with complete consolidation requiring immobilization for 6–8 weeks.Conclusions:1. Valgus deformity of the elbow joint is a complex pathology affecting 7–8% of cases and causing early disability in children.2. Choice of surgical strategy based on deformity severity, trauma duration, and child’s age improves treatment outcomes.3. Advanced surgical techniques enable simultaneous restoration of anatomical structure and distal humeral end formation, thereby restoring elbow joint function in children.4. Hybrid osteosynthesis techniques facilitate early recovery of elbow joint function.This study underscores the importance of tailored, minimally invasive, and innovative approaches to managing pediatric elbow pathologies and associated complications.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML